UC San Diego UC San Diego Electronic Theses and Dissertations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
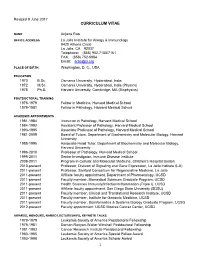
Revised January 2003
Revised 9 June 2017 CURRICULUM VITAE NAME Anjana Rao OFFICE ADDRESS La Jolla Institute for Allergy & Immunology 9420 Athena Circle La Jolla, CA 92037 Telephone: (858) 952-7155/7161 FAX: (858) 752-6984 Email: [email protected] PLACE OF BIRTH Washington, D. C., USA EDUCATION 1970 B.Sc. Osmania University, Hyderabad, India 1972 M.Sc. Osmania University, Hyderabad, India (Physics) 1978 Ph.D. Harvard University, Cambridge, MA (Biophysics) POSTDOCTORAL TRAINING 1978-1979 Fellow in Medicine, Harvard Medical School 1979-1981 Fellow in Pathology, Harvard Medical School ACADEMIC APPOINTMENTS 1981-1984 Instructor in Pathology, Harvard Medical School 1984-1992 Assistant Professor of Pathology, Harvard Medical School 1993-1995 Associate Professor of Pathology, Harvard Medical School 1981-2009 Board of Tutors, Department of Biochemistry and Molecular Biology, Harvard University 1988-1995 Associate Head Tutor, Department of Biochemistry and Molecular Biology, Harvard University 1996-2010 Professor of Pathology, Harvard Medical School 1995-2011 Senior Investigator, Immune Disease Institute 2009-2011 Program in Cellular and Molecular Medicine, Children’s Hospital Boston 2010-present Professor, Division of Signaling and Gene Expression, La Jolla Institute (LJI) 2011-present Professor, Sanford Consortium for Regenerative Medicine, La Jolla 2011-present Affiliate faculty appointment, Department of Pharmacology, UCSD 2011-present Faculty member, Biomedical Sciences Graduate Program, UCSD 2011-present Health Sciences Immunity/Infection/Inflammation (Triple I), UCSD -
NR4A Transcription Factors Limit CAR T Cell Function in Solid Tumors
LETTER https://doi.org/10.1038/s41586-019-0985-x NR4A transcription factors limit CAR T cell function in solid tumours Joyce Chen1,2,3,4*, Isaac F. López-Moyado1,4,5, Hyungseok Seo1, Chan-Wang J. Lio1, Laura J. Hempleman1, Takashi Sekiya6, Akihiko Yoshimura7, James P. Scott-Browne1,4,9,10* & Anjana Rao1,3,4,8,10* T cells expressing chimeric antigen receptors (CAR T cells) targeting CD8+CD45.1+ OT-I cells (specific for chicken ovalbumin (OVA) human CD19 (hCD19) have shown clinical efficacy against B cell SIINFEKL peptide presented by H-2Kb; Extended Data Fig. 2a, b) malignancies1,2. CAR T cells have been less effective against solid showed similar tumour growth rates (Extended Data Fig. 2c); low tumours3–5, in part because they enter a hyporesponsive (‘exhausted’ numbers of CAR T cells were transferred to minimize tumour rejec- or ‘dysfunctional’) state6–9 triggered by chronic antigen stimulation tion (Extended Data Fig. 2d). Eight days after adoptive transfer, CAR and characterized by upregulation of inhibitory receptors and loss of and OT-I tumour-infiltrating lymphocytes (TILs) (Fig. 1b, Extended effector function. To investigate the function of CAR T cells in solid Data Fig. 2b, e, f) comprised around 18% and 9%, respectively, of CD8+ tumours, we transferred hCD19-reactive CAR T cells into hCD19+ TILs (Fig. 1c) and exhibited similar proportions of PD-1hiTIM3hi cells tumour-bearing mice. CD8+CAR+ tumour-infiltrating lymphocytes compared to endogenous TILs (Fig. 1b, Extended Data Fig. 2b). All and CD8+ endogenous tumour-infiltrating lymphocytes expressing TILs produced low levels of TNF and IFNγ upon re-stimulation with the inhibitory receptors PD-1 and TIM3 exhibited similar profiles PMA and ionomycin (Fig. -

Tet2 and Tet3 Cooperate with B-Lineage Transcription Factors To
RESEARCH ARTICLE Tet2 and Tet3 cooperate with B-lineage transcription factors to regulate DNA modification and chromatin accessibility Chan-Wang Lio1†, Jiayuan Zhang2†, Edahı´Gonza´ lez-Avalos1, Patrick G Hogan1, Xing Chang1,2,3*, Anjana Rao1,3,4,5* 1Division of Signaling and Gene Expression, San Diego, United States; 2Key Laboratory of Stem Cell Biology, Institute of Health Sciences, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences and Shanghai Jiao Tong University School of Medicine, Shanghai, China; 3Sanford Consortium for Regenerative Medicine, San Diego, United States; 4Department of Pharmacology, University of California, San Diego, San Diego, United States; 5Moores Cancer Center, University of California, San Diego, San Diego, United States Abstract Ten-eleven translocation (TET) enzymes oxidize 5-methylcytosine, facilitating DNA demethylation and generating new epigenetic marks. Here we show that concomitant loss of Tet2 and Tet3 in mice at early B cell stage blocked the pro- to pre-B cell transition in the bone marrow, decreased Irf4 expression and impaired the germline transcription and rearrangement of the Igk locus. Tet2/3-deficient pro-B cells showed increased CpG methylation at the Igk 3’ and distal enhancers that was mimicked by depletion of E2A or PU.1, as well as a global decrease in chromatin accessibility at enhancers. Importantly, re-expression of the Tet2 catalytic domain in *For correspondence: Tet2/3-deficient B cells resulted in demethylation of the Igk enhancers and restored their chromatin [email protected] (XC); arao@ accessibility. Our data suggest that TET proteins and lineage-specific transcription factors lji.org (AR) cooperate to influence chromatin accessibility and Igk enhancer function by modulating the modification status of DNA. -

NFAT Transcription Factors Promote the Generation of Follicular Helper T Cells in Response to Acute Viral Infection
Cutting Edge: NFAT Transcription Factors Promote the Generation of Follicular Helper T Cells in Response to Acute Viral Infection This information is current as Gustavo J. Martinez, Joyce K. Hu, Renata M. Pereira, Jordan of September 28, 2021. S. Crampton, Susan Togher, Nicholas Bild, Shane Crotty and Anjana Rao J Immunol published online 5 February 2016 http://www.jimmunol.org/content/early/2016/02/04/jimmun ol.1501841 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2016/02/04/jimmunol.150184 Material 1.DCSupplemental http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 28, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published February 5, 2016, doi:10.4049/jimmunol.1501841 Th eJournal of Cutting Edge Immunology Cutting Edge: NFAT Transcription Factors Promote the Generation of Follicular Helper T Cells in Response to Acute Viral Infection † ,1 † Gustavo J. Martinez,* Joyce K. -

Remembrances of Guido As Teacher Are Provided in Appendix V
Contents page Introduction 4 Overview 5 Comment 6 Phase I. Hemoglobin 7 Phase II. A new challenge: membrane proteins 8 First prong - red blood cell membranes 10 Band 3 The cytoskeleton A link The glucose transporter Second prong - the (Na+,K+)-ATPase 12 Thirty years of the sodium pump Extensions More methods Phase III. The next frontier: hormonal regulation of membrane transporters 15 First prong - regulation of adenylate cyclase by vasopressin 15 Second prong - regulation by insulin 15 Insulin stimulation of the sodium pump Hypokalemic periodic paralysis (HPP) The insulin receptor Phase IV. Pièce de Résistance: ecto-ATPase CD39 (now ENTPDase1) 18 Discovery 19 General conceptual framework 20 Extensions 21 ATP transport 22 Regulation 24 By vacuolar H+-ATPase assembly in yeast By N-glycosylation-dependent localization in mammalian cells Mechanism 25 Two terminal transmembrane domains Functional interplay between the transmembrane domains and the ATPase active site and modulation of substrate preference Dynamic rotation of the transmembrane helices Modulation by membrane elasticity and biological implications Off the beaten path 30 Carbonic anhydrase; proteolytic artifacts; yeast Mg2+-ATPase; mitochondrial and nuclear membranes; chloride transport; MalK; ATPase activity of the retina; invertebrate oxygen carriers; and space polymers Summary 32 In the words of his students and colleagues. 32 Ted Abraham; Alessandro Alessandrini; Laurie Bankston; Bob Bloch; James Booth; David Brandon; Jeff Brodsky; Gilbert Chin; Steve Clarke; Kurt Drickamer; Betty Eipper; Adam Faye; Mike Forgac; Michael Gottesman; Alison Grinthal; Mas Handa; Renate Hellmiss; Yen-Ming Hsu; Dan Jay; (see next page) 2 Lee Josephson; Nancy Kleckner; Minjeong Kim; Christine Li; Jia Liu; Sisto Luciani; Jonathan Lytton; Yvonne Ou; Rajeev Malhotra; Julie EM McGeoch; Diana McGill; Eric Mortensen; Sari Paavilainen; Debbie Peattie; Anjana Rao; Reinhart Reithmeier; Marilyn Resh; Simon Robson; Howie Shuman; Scott Thacher; Bill Tsai; Gonul Velicelebi; Chung Wang; Ting-Fang Wang; Gail Willsky; Xiaotian Zhong. -

October 27, 2020 PROFESSOR STEPHEN HEDRICK, Professor
ACADEMIC SENATE: SAN DIEGO DIVISION, 0002 UCSD, LA JOLLA, CA 92093-0002 (858) 534-3640 FAX (858) 534-4528 October 27, 2020 PROFESSOR STEPHEN HEDRICK, Professor Division of Biological Sciences PROFESSOR MITCHELL KRONENBERG, Professor Division of Biological Sciences PROFESSOR KIT POGLIANO, Dean Division of Biological Sciences PROFESSOR ASA GUSTAFSSON, Chair Biomedical Sciences Graduate Program SUBJECT: Proposal to establish PhD Specialization in Immunology At its October 12, 2020 meeting, the Graduate Council approved the proposal to establish a PhD specialization in Immunology, to be offered to students in the Division of Biological Sciences and the Biomedical Sciences Graduate Program. The Council supports the creation of the following degree titles: PhD in Biology with a Specialization in Immunology PhD in Biomedical Sciences with a Specialization in Immunology Final approval from the Representative Assembly is required to establish the new degree titles. Prior to forwarding the proposal for placement on an upcoming Representative Assembly agenda, please provide an addendum to the proposal that clarifies the requirements for doctoral committee membership for the specialization to Senate Associate Director Lori Hullings ([email protected]). Rather than provide links to the committee membership for each program, please clearly state the committee membership for a student in the Immunology specialization. It would be helpful to include if a co-chair is required if the Immunology faculty advisor is not from the student’s home department and who is eligible to serve as the tenured outside member. If approved, the new degree titles will be available to students in Fall Quarter 2021. Sincerely, Lynn Russell, Chair Graduate Council cc: M. -

T Cell Exhaustion’ Autoreactivity; Thus, Exhausted T Cells Are Not Inherently Good Or Bad
VIEWPOINT chronic antigen stimulation that is probably important to limit immunopathology or Defining ‘T cell exhaustion’ autoreactivity; thus, exhausted T cells are not inherently good or bad. Christian U. Blank , W. Nicholas Haining, Werner Held , Patrick G. Hogan , Pamela L. Schwartzberg. Axel Kallies , Enrico Lugli , Rachel C. Lynn , Mary Philip , Anjana Rao, Yes, although exhaustion is often seen as a dysfunctional Nicholas P. Restifo, Andrea Schietinger , Ton N. Schumacher , state, it also allows T cells to persist and Pamela L. Schwartzberg , Arlene H. Sharpe , Daniel E. Speiser , partially contain chronic infections without E. John Wherry , Benjamin A. Youngblood and Dietmar Zehn causing immunopathology. Abstract | ‘T cell exhaustion’ is a broad term that has been used to describe the Mary Philip and Andrea Schietinger. Like response of T cells to chronic antigen stimulation, first in the setting of chronic viral our colleagues, we define T cell exhaustion infection but more recently in response to tumours. Understanding the features of as a differentiation state that is observed and pathways to exhaustion has crucial implications for the success of checkpoint during chronic infections in the presence blockade and adoptive T cell transfer therapies. In this Viewpoint article, 18 experts of persistent antigen and chronic T cell receptor (TCR) stimulation. Exhausted in the field tell us what exhaustion means to them, ranging from complete lack of T cells express inhibitory receptors but can effector function to altered functionality to prevent immunopathology, with retain some antipathogen effector function, potential differences between cancer and chronic infection. Their responses resulting in a pathogen–host ‘stalemate’4. highlight the dichotomy between terminally differentiated exhausted T cells that E.J.W. -

TOX and TOX2 Transcription Factors Cooperate with NR4A Transcription Factors to Impose CD8+ T Cell Exhaustion
Correction IMMUNOLOGY AND INFLAMMATION Correction for “TOX and TOX2 transcription factors cooper- Wu, Li-Fan Lu, Patrick G. Hogan, Avinash Bhandoola, and + ate with NR4A transcription factors to impose CD8 T Anjana Rao, which was first published May 31, 2019; cell exhaustion,” by Hyungseok Seo, Joyce Chen, Edahí 10.1073/pnas.1905675116 (Proc. Natl. Acad. Sci. U.S.A. 116, González-Avalos, Daniela Samaniego-Castruita, Arundhoti 12410–12415). Das, Yueqiang H. Wang, Isaac F. López-Moyado, Romain The authors note that Fig. 1 appeared incorrectly. The cor- O. Georges, Wade Zhang, Atsushi Onodera, Cheng-Jang rected figure and its legend appear below. A B B16-hCD19 TumorCAR T cellCAR TIL Analysis D24 D24 inoculation Adoptive Transfer D20 D20 D0 D12 D16 D20 D24 D16 D16 C57BL/6 D12 D12 TOX Relative cell number TOX: PE PD-1: APC PD-1 CD CORRECTION in vitro CAR T 20 100 in vitro CAR T ** CAR TIL ** 15 80 CAR TIL 60 ** 10 ** ** 40 (v.s. hprt) (v.s. 5 20 Relative expression 0 TNF: BV421 0 Tox Tox2 IFN-APC cells T Cytokine+ CAR TNF IFN E 60 **** In vitro CAR T TNF+IFN- CAR TIL p<0.0001 30 Specific lysis (%) 0 10:1 3:1 1:1 Effector:Target ratio Fig. 1. TOX transcription factors are highly expressed in exhausted CAR TILs in solid tumors. (A) Experimental scheme for analyzing tumor-infiltrating CAR T cells (CAR TILs); 5 × 105 B16-hCD19 tumor cells were inoculated subcutaneously into C57BL/6 mice. Twelve days later, 1.5 × 106 CAR T cells were adoptively transferred into the tumor-bearing mice by intravenous injection. -

Cover Legend: João P.B
Viola-r.qxd 26/1/2011 12:03 ÌÌ ™ÂÏ›‰·1 INTERNATIONAL JOURNAL OF ONCOLOGY 38: 591-592, 2011 1 Cover legend: João P.B. Viola; a member of The Editorial Academy of The International Journal of Oncology NFAT1. Dr Viola and colleagues demonstrated that NFAT- deficient mice consistently showed a marked increase in their immune response; likewise, CD4+ T cells from NFAT1-/- mice displayed an enhanced Th2 immunity, as evidenced by an overexpression of IL-4. These data suggested for the first time that the NFAT1 transcription factor might have a negative role in regulating T cell proliferation and cytokine gene expression during the immune response. His studies were very well received, resulting in publications in Science, Immunity and Blood. He also took on a much more biochemical project while he was at Dr Rao's laboratory, mapping the in vivo phosphorylation sites of the NFAT1 transcription factor in resting and activated T cells. This work still stands as the best example of how to identify all the functionally relevant phosphorylation sites of a heavily phosphorylated protein. It João P.B. Viola is a Senior Scientist at the National Cancer was incorporated into two papers, published in Journal of Institute (INCA), Rio de Janeiro, Brazil. The long-term interest Biological Chemistry and Molecular Cell, which described the of Dr Viola's laboratory is to study the cellular and molecular biochemical mechanisms of NFAT1 regulation by phospho- mechanisms of inducible gene transcription in cell activation rylation and calcineurin-mediated dephosphorylation. and transformation. The main area of investigation is focused As an independent investigator at the Brazilian National on studying the role of NFAT (Nuclear Factor of Activated Cancer Institute, Dr Viola focused his studies on better under- T cells) transcription factors in cell cycle progression, cell standing the molecular mechanisms of the NFAT proteins in differentiation and apoptosis, and their relation to malignant lymphocyte proliferation and cell cycle regulation. -

TRANSCRIPTION FACTORS of the NFAT FAMILY: Regulation and Function
P1: MBL/plb P2: MBL/rsk QC: MBL/uks T1: MBL February 12, 1997 16:24 Annual Reviews AR026-27 AR26-27 Annu. Rev. Immunol. 1997. 15:707–47 Copyright c 1997 by Annual Reviews Inc. All rights reserved TRANSCRIPTION FACTORS OF THE NFAT FAMILY: Regulation and Function Anjana Rao∗, Chun Luo∗, and Patrick G. Hogan Center for Blood Research and the ∗Department of Pathology, Harvard Medical School, 200 Longwood Avenue, Boston, Massachusetts 02115; email: [email protected] KEY WORDS: nuclear factor of activated T cells, immunosuppression, cytokine gene regula- tion, inducible gene transcription, signal transduction, lymphocyte activation, calcineurin ABSTRACT As targets for the immunosuppressive drugs cyclosporin A and FK506, transcrip- tion factors of the NFAT (nuclear factor of activated T cells) family have been the focus of much attention. NFAT proteins, which are expressed in most immune- system cells, play a pivotal role in the transcription of cytokine genes and other genes critical for the immune response. The activity of NFAT proteins is tightly regulated by the calcium/calmodulin-dependent phosphatase calcineurin, a pri- mary target for inhibition by cyclosporin A and FK506. Calcineurin controls the translocation of NFAT proteins from the cytoplasm to the nucleus of activated cells by interacting with an N-terminal regulatory domain conserved in the NFAT family. The DNA-binding domains of NFAT proteins resemble those of Rel- family proteins, and Rel and NFAT proteins show some overlap in their ability to bind to certain regulatory elements in cytokine genes. NFAT is also notable for its ability to bind cooperatively with transcription factors of the AP-1 (Fos/Jun) family to composite NFAT:AP-1 sites, found in the regulatory regions of many genes that are inducibly transcribed by immune-system cells. -

NFAT Transcription Factors Promote the Generation of Follicular Helper T Cells in Response to Acute Viral Infection
Cutting Edge: NFAT Transcription Factors Promote the Generation of Follicular Helper T Cells in Response to Acute Viral Infection This information is current as Gustavo J. Martinez, Joyce K. Hu, Renata M. Pereira, Jordan of September 25, 2021. S. Crampton, Susan Togher, Nicholas Bild, Shane Crotty and Anjana Rao J Immunol 2016; 196:2015-2019; Prepublished online 5 February 2016; doi: 10.4049/jimmunol.1501841 Downloaded from http://www.jimmunol.org/content/196/5/2015 Supplementary http://www.jimmunol.org/content/suppl/2016/02/04/jimmunol.150184 Material 1.DCSupplemental http://www.jimmunol.org/ References This article cites 32 articles, 12 of which you can access for free at: http://www.jimmunol.org/content/196/5/2015.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 25, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Th eJournal of Cutting Edge Immunology Cutting Edge: NFAT Transcription Factors Promote the Generation of Follicular Helper T Cells in Response to Acute Viral Infection † ,1 † Gustavo J. -

Downloaded from GEO (GSE54191)
bioRxiv preprint doi: https://doi.org/10.1101/2021.03.01.433424; this version posted March 1, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 2+ Non-canonical Hedgehog signaling through L-type voltage gated Ca channels controls CD8+ T cell killing Joachim Hanna, Chrysa Kapeni, Louise O’Brien, Valentina Carbonaro, Flavio Beke, 5 Chandra Chilamakuri, and Maike de la Roche§ University of Cambridge, Cancer Research UK Cambridge Institute, Robinson Way, Cambridge CB2 0RE, UK 10 §Corresponding author. Email: [email protected] (M.d.l.R.) 15 ABSTRACT Cytotoxic CD8+ T lymphocytes (CTLs) are critical to the immune response against intracellular pathogens and cancer and act by eliminating infected and malignant cells through targeted secretion of cytotoxic granules. Hedgehog (Hh) signaling has been shown to be critical for CTL killing. Interestingly, Hh signaling in CD8+ T cells is not 20 induced by extracellular Hh ligands but is initiated upon T cell receptor (TCR) engagement. How the TCR induces the Hh pathway independently of extracellular Hh ligands is unknown. Here we show that the Hh transcription factor Gli1 is essential for efficient CTL function and is induced downstream of the TCR by an extracellular Ca2+ influx selectively controlled by L-type voltage gated Ca2+ channels localized at the plasma 25 membrane. We demonstrate that this novel mode of Hh signaling induction is independent of the canonical Hh pathway and represents the primary mechanism of Gli1 induction in naïve CD8+ T cells, while CTLs can also activate Gli1 via MAP Kinase signaling.