NR4A Transcription Factors Limit CAR T Cell Function in Solid Tumors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Rise and Fall of the Bovine Corpus Luteum
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Spring 5-6-2017 The Rise and Fall of the Bovine Corpus Luteum Heather Talbott University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Biochemistry Commons, Molecular Biology Commons, and the Obstetrics and Gynecology Commons Recommended Citation Talbott, Heather, "The Rise and Fall of the Bovine Corpus Luteum" (2017). Theses & Dissertations. 207. https://digitalcommons.unmc.edu/etd/207 This Dissertation is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. THE RISE AND FALL OF THE BOVINE CORPUS LUTEUM by Heather Talbott A DISSERTATION Presented to the Faculty of the University of Nebraska Graduate College in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Biochemistry and Molecular Biology Graduate Program Under the Supervision of Professor John S. Davis University of Nebraska Medical Center Omaha, Nebraska May, 2017 Supervisory Committee: Carol A. Casey, Ph.D. Andrea S. Cupp, Ph.D. Parmender P. Mehta, Ph.D. Justin L. Mott, Ph.D. i ACKNOWLEDGEMENTS This dissertation was supported by the Agriculture and Food Research Initiative from the USDA National Institute of Food and Agriculture (NIFA) Pre-doctoral award; University of Nebraska Medical Center Graduate Student Assistantship; University of Nebraska Medical Center Exceptional Incoming Graduate Student Award; the VA Nebraska-Western Iowa Health Care System Department of Veterans Affairs; and The Olson Center for Women’s Health, Department of Obstetrics and Gynecology, Nebraska Medical Center. -

Assessment of NR4A Ligands That Directly Bind and Modulate the Orphan Nuclear Receptor Nurr1
bioRxiv preprint doi: https://doi.org/10.1101/2020.05.22.109017; this version posted May 25, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Assessment of NR4A Ligands that Directly Bind and Modulate the Orphan Nuclear Receptor Nurr1 Paola Munoz-Tello 1, Hua Lin 2,3, Pasha Khan 2, Ian Mitchelle S. de Vera 1,4, Theodore M. Kamenecka 2, and Douglas J. Kojetin 1,2,* 1 Department of Integrative Structural and Computational Biology, The Scripps Research Institute, Jupiter, FL, 33458, USA 2 Department of Molecular Medicine, The Scripps Research Institute, Jupiter, Florida 33458, USA 3 Current address: Biomedical Research Center of South China, College of Life Sciences, Fujian Normal University, Fuzhou 350117, China 4 Current address: Department of Pharmacology and Physiology, Saint Louis University School of Medicine, St. Louis, MO 63104, USA * Correspondence: [email protected] as ligands that increase Nurr1 transcription in human neuroblastoma SK- ABSTRACT N-BE(2)-C cells (11). Amodiaquine improves behavioral alterations in a Nurr1/NR4A2 is an orphan nuclear receptor transcription factor im- Parkinson’s disease animal model (11) and improves neuropathology and plicated as a potential drug target for neurological disorders including memory impairment in an Alzheimer’s disease animal model (12). Alzheimer’s and Parkinson’s diseases. Previous studies identified small molecule modulators of NR4A nuclear receptors including Nurr1 and Amodiaquine is the most potent and efficacious Nurr1 agonist of the Nur77/NR4A1; it remains unclear whether these ligands affect Nurr1 4-amino-7-chloroquinoline compounds, but these compounds are not through direct binding or indirect non-binding mechanisms. -

Chromosomal Instability in Acute Myeloid Leukemia
cancers Review Chromosomal Instability in Acute Myeloid Leukemia Mateus de Oliveira Lisboa 1 , Paulo Roberto Slud Brofman 1, Ana Teresa Schmid-Braz 2, Aline Rangel-Pozzo 3,* and Sabine Mai 3,* 1 Core for Cell Technology, School of Medicine, Pontifícia Universidade Católica do Paraná—PUCPR, Curitiba 80215-901, Paraná, Brazil; [email protected] (M.d.O.L.); [email protected] (P.R.S.B.) 2 Hospital das Clínicas, Universidade Federal do Paraná, Curitiba 80060-240, Paraná, Brazil; [email protected] 3 Department of Physiology and Pathophysiology, University of Manitoba, Cell Biology, CancerCare Manitoba Research Institute, Winnipeg, MB R3C 2B7, Canada * Correspondence: [email protected] (A.R.-P.); [email protected] (S.M.); Tel.: +1-(204)787-4125 (S.M.) Simple Summary: Chromosome instability (CIN) is an increased rate where chromosome acquire alterations due to errors in cell division. CIN creates genetic and cytogenetic diversity and is a common feature in hematological malignancies such as acute myeloid leukemia (AML). Low to moderate levels of CIN seems to be well tolerated and can promote cancer proliferation, genetic diversity, and tumor evolution. However, high levels of CIN seems to be lethal, where enhancing CIN could improve AML treatment. However, little is known about CIN in AML. Our review focus on CIN studies in AML, their prognostic results, as well as the use of CIN as a therapeutic target in AML. Abstract: Chromosomal instability (CIN), the increasing rate in which cells acquire new chromoso- mal alterations, is one of the hallmarks of cancer. Many studies highlighted CIN as an important Citation: de Oliveira Lisboa, M.; mechanism in the origin, progression, and relapse of acute myeloid leukemia (AML). -

By Submitted in Partial Satisfaction of the Requirements for Degree of in In
BCL6 maintains thermogenic capacity of brown adipose tissue during dormancy by Vassily Kutyavin DISSERTATION Submitted in partial satisfaction of the requirements for degree of DOCTOR OF PHILOSOPHY in Biomedical Sciences in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, SAN FRANCISCO Approved: ______________________________________________________________________________Eric Verdin Chair ______________________________________________________________________________Ajay Chawla ______________________________________________________________________________Ethan Weiss ______________________________________________________________________________ ______________________________________________________________________________ Committee Members Copyright 2019 by Vassily Kutyavin ii Dedicated to everyone who has supported me during my scientific education iii Acknowledgements I'm very grateful to my thesis adviser, Ajay Chawla, for his mentorship and support during my dissertation work over the past five years. Throughout my time in his lab, I was always able to rely on his guidance, and his enthusiasm for science was a great source of motivation. Even when he was traveling, he could easily be reached for advice by phone or e- mail. I am particularly grateful for his help with writing the manuscript, which was probably the most challenging aspect of graduate school for me. I am also very grateful to him for helping me find a postdoctoral fellowship position. Ajay's inquisitive and fearless approach to science have been a great inspiration to me. In contrast to the majority of scientists who focus narrowly on a specific topic, Ajay pursued fundamental questions across a broad range of topics and was able to make tremendous contributions. My experience in his lab instilled in me a deep appreciation for thinking about the entire organism from an evolutionary perspective and focusing on the key questions that escape the attention of the larger scientific community. As I move forward in my scientific career, there is no doubt that I will rely on him as a role model. -
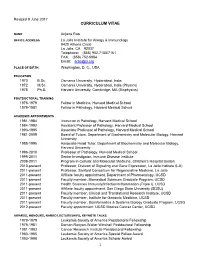
Revised January 2003
Revised 9 June 2017 CURRICULUM VITAE NAME Anjana Rao OFFICE ADDRESS La Jolla Institute for Allergy & Immunology 9420 Athena Circle La Jolla, CA 92037 Telephone: (858) 952-7155/7161 FAX: (858) 752-6984 Email: [email protected] PLACE OF BIRTH Washington, D. C., USA EDUCATION 1970 B.Sc. Osmania University, Hyderabad, India 1972 M.Sc. Osmania University, Hyderabad, India (Physics) 1978 Ph.D. Harvard University, Cambridge, MA (Biophysics) POSTDOCTORAL TRAINING 1978-1979 Fellow in Medicine, Harvard Medical School 1979-1981 Fellow in Pathology, Harvard Medical School ACADEMIC APPOINTMENTS 1981-1984 Instructor in Pathology, Harvard Medical School 1984-1992 Assistant Professor of Pathology, Harvard Medical School 1993-1995 Associate Professor of Pathology, Harvard Medical School 1981-2009 Board of Tutors, Department of Biochemistry and Molecular Biology, Harvard University 1988-1995 Associate Head Tutor, Department of Biochemistry and Molecular Biology, Harvard University 1996-2010 Professor of Pathology, Harvard Medical School 1995-2011 Senior Investigator, Immune Disease Institute 2009-2011 Program in Cellular and Molecular Medicine, Children’s Hospital Boston 2010-present Professor, Division of Signaling and Gene Expression, La Jolla Institute (LJI) 2011-present Professor, Sanford Consortium for Regenerative Medicine, La Jolla 2011-present Affiliate faculty appointment, Department of Pharmacology, UCSD 2011-present Faculty member, Biomedical Sciences Graduate Program, UCSD 2011-present Health Sciences Immunity/Infection/Inflammation (Triple I), UCSD -

Inhibition of Nr4a Receptors Enhances Anti-Tumor Immunity by Breaking Treg-Mediated Immune Tolerance
Author Manuscript Published OnlineFirst on March 20, 2018; DOI: 10.1158/0008-5472.CAN-17-3102 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Inhibition of Nr4a receptors enhances anti-tumor immunity by breaking Treg-mediated immune tolerance Sana Hibino1, Shunsuke Chikuma1, Taisuke Kondo1, Minako Ito1, Hiroko Nakatsukasa1, Setsuko Omata-Mise1, and Akihiko Yoshimura1,2 1Department of Microbiology and Immunology, Keio University School of Medicine 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan 2Correspondence to: Akihiko Yoshimura, PhD Department of Microbiology and Immunology Keio University School of Medicine 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan Phone: +81-3-5363-3483 Fax: +81-3-5360-1508 Email: [email protected] Running title: Promotion of anti-tumor immunity by Nr4a inhibition Keywords: regulatory T cell, immune tolerance, tumor immunology, transcription factors, animal models of cancer Conflict of Interest Statement: The authors declare no potential conflicts of interest. Acknowledgements: We thank N. Shiino, M. Ohkura, Y. Tokifuji, and Y. Hirata for their technical assistance. This work was supported by JSPS KAKENHI (S) 17H06175 (to A. Yoshimura), Advanced Research & Development Programs for Medical Innovation (AMED-CREST) JP17gm0510019 (to A. Yoshimura), the Takeda Science Foundation (to A. Yoshimura), the Uehara Memorial Foundation (to A. Yoshimura), the SENSHIN Medical Research Foundation (to A. Yoshimura), and Grant-in-Aid for Scientific Research on Innovative Areas 17H05801 (to S. Chikuma). 1 Downloaded from cancerres.aacrjournals.org on October 7, 2021. © 2018 American Association for Cancer Research. Author Manuscript Published OnlineFirst on March 20, 2018; DOI: 10.1158/0008-5472.CAN-17-3102 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Supplemental Text and Figures
Supplemental Materials and Methods Experimental bone metastasis assay Primary PCa cells were sorted by GFP marker from mTmG+ tumors, and 105 cells in 20μL PBS were injected using Hamilton syringe into the tibia of 6-week old NSG mice. Mice were monitored biweekly for moribund signs for euthanasia and organ harvest. Noninvasive mouse and ex vivo imaging MRI imaging with Bruker ICON and fluorescence imaging of fresh organs with metastasis enumeration were recently described (Lu et al. 2017). Primary prostate cell sphere formation assay Isolate of primary cells from prostate, culture and counting of prostatospheres on Matrigel were performed as described (Lukacs et al. 2010). For organoid culture assay, we followed a published matrigel embedding method (Chua et al. 2014). RNA-Seq and differential gene expression Total RNA was isolated from prostate tumors using Direct-zol RNA MiniPrep Kit (Zymo Research) and processed for stranded total RNA-Seq using Illumina HiSeq 4000 at Sequencing and Microarray Facility at MD Anderson Cancer Center. The differential expression analysis was performed using the DESeq2 package of R. P-values obtained after multiple binomial tests were adjusted using BH method. Significant genes are defined by using a cut-off of 0.05 on the BH corrected p-value and an absolute log2 fold change value of at least 1.5. Histology and western blot H&E stain, immunohistochemical (IHC) and western blot were performed as previously described (Ding et al. 2011; Wang et al. 2016). Primary antibodies for IHC include Ki67 (Fisher, RM-9106-S1), cleaved caspase 3 (Cell Signaling Technology aka CST, 9661), cyclin D1 (Fisher, clone SP4), TGFBR2 (Abcam, ab61213), BMPR2 (Abcam, ab130206), AR (EMD Millipore, 06-680), phospho- Akt (CST, 4060), GFP (CST, 2956), E-Cadherin (CST, 14472). -

The CBP KIX Domain Regulates Long-Term Memory and Circadian Activity Snehajyoti Chatterjee1,2,3†, Christopher C
Chatterjee et al. BMC Biology (2020) 18:155 https://doi.org/10.1186/s12915-020-00886-1 RESEARCH ARTICLE Open Access The CBP KIX domain regulates long-term memory and circadian activity Snehajyoti Chatterjee1,2,3†, Christopher C. Angelakos4,5†, Ethan Bahl6,7, Joshua D. Hawk4,5, Marie E. Gaine3, Shane G. Poplawski4,5,8, Anne Schneider-Anthony1,2, Manish Yadav3, Giulia S. Porcari5, Jean-Christophe Cassel1, K. Peter Giese9, Jacob J. Michaelson6,10,11,12, Lisa C. Lyons3,13, Anne-Laurence Boutillier1,2* and Ted Abel3* Abstract Background: CREB-dependent transcription necessary for long-term memory is driven by interactions with CREB- binding protein (CBP), a multi-domain protein that binds numerous transcription factors potentially affecting expression of thousands of genes. Identifying specific domain functions for multi-domain proteins is essential to understand processes such as cognitive function and circadian clocks. We investigated the function of the CBP KIX domain in hippocampal memory and gene expression using CBPKIX/KIX mice with mutations that prevent phospho- CREB (Ser133) binding. Results: We found that CBPKIX/KIX mice were impaired in long-term memory, but not learning acquisition or short- term memory for the Morris water maze. Using an unbiased analysis of gene expression in the dorsal hippocampus after training in the Morris water maze or contextual fear conditioning, we discovered dysregulation of CREB, CLOCK, and BMAL1 target genes and downregulation of circadian genes in CBPKIX/KIX mice. Given our finding that the CBP KIX domain was important for transcription of circadian genes, we profiled circadian activity and phase resetting in CBPKIX/KIX mice. -

Milk's Role As an Epigenetic Regulator in Health and Disease
Review Milk’s Role as an Epigenetic Regulator in Health and Disease Bodo C. Melnik 1,* and Gerd Schmitz 2 1 Department of Dermatology, Environmental Medicine and Health Theory, Faculty of Human Sciences, University of Osnabrück, Am Finkenhügel 7a, D-49076 Osnabrück, Germany 2 Institute for Clinical Chemistry and Laboratory Medicine, University Hospital Regensburg, University of Regensburg, Franz-Josef-Strauß-Allee 11, D-93053 Regensburg, Germany; [email protected] * Correspondence: [email protected]; Tel.: +49-5241-988-060; Fax: +49-5241-25801 Academic Editor: Takeo Kubota Received: 7 January 2017; Accepted: 7 March 2017; Published: 15 March 2017 Abstract: It is the intention of this review to characterize milk’s role as an epigenetic regulator in health and disease. Based on translational research, we identify milk as a major epigenetic modulator of gene expression of the milk recipient. Milk is presented as an epigenetic “doping system” of mammalian development. Milk exosome-derived micro-ribonucleic acids (miRNAs) that target DNA methyltransferases are implicated to play the key role in the upregulation of developmental genes such as FTO, INS, and IGF1. In contrast to miRNA-deficient infant formula, breastfeeding via physiological miRNA transfer provides the appropriate signals for adequate epigenetic programming of the newborn infant. Whereas breastfeeding is restricted to the lactation period, continued consumption of cow’s milk results in persistent epigenetic upregulation of genes critically involved in the development of diseases of civilization such as diabesity, neurodegeneration, and cancer. We hypothesize that the same miRNAs that epigenetically increase lactation, upregulate gene expression of the milk recipient via milk-derived miRNAs. -

BI1071, a Novel Nur77 Modulator, Induces Apoptosis of Cancer Cells
Published OnlineFirst March 29, 2019; DOI: 10.1158/1535-7163.MCT-18-0918 Small Molecule Therapeutics Molecular Cancer Therapeutics BI1071, a Novel Nur77 Modulator, Induces Apoptosis of Cancer Cells by Activating the Nur77-Bcl-2 Apoptotic Pathway Xiaohui Chen1, Xihua Cao2, Xuhuang Tu1, Gulimiran Alitongbieke1, Zebin Xia2, Xiaotong Li1, Ziwen Chen1,MeimeiYin,DanXu1, Shangjie Guo1, Zongxi Li1, Liqun Chen1,XindaoZhang1,DingyuXu1, Meichun Gao1,JieLiu1, Zhiping Zeng1, Hu Zhou1,YingSu2, and Xiao-kun Zhang1,2 Abstract Nur77 (also called TR3 or NGFI-B), an orphan member of indole-3-carbinol metabolite, as a modulator of the Nur77- the nuclear receptor superfamily, induces apoptosis by trans- Bcl-2 apoptotic pathway. BI1071 binds Nur77 with high locating to mitochondria where it interacts with Bcl-2 to affinity, promotes Nur77 mitochondrial targeting and inter- convert Bcl-2 from an antiapoptotic to a pro-apoptotic mol- action with Bcl-2, and effectively induces apoptosis of cancer ecule. Nur77 posttranslational modification such as phos- cells in a Nur77- and Bcl-2–dependent manner. Studies with phorylation has been shown to induce Nur77 translocation animal model showed that BI1071 potently inhibited the from the nucleus to mitochondria. However, small molecules growth of tumor cells in animals through its induction of that can bind directly to Nur77 to trigger its mitochondrial apoptosis. Our results identify BI1071 as a novel Nur77- localization and Bcl-2 interaction remain to be explored. Here, binding modulator of the Nur77-Bcl-2 apoptotic pathway, we report our identification and characterization of DIM-C- which may serve as a promising lead for treating cancers with þ À pPhCF3 MeSO3 (BI1071), an oxidized product derived from overexpression of Bcl-2. -

Internet-Oheis Aineiston Taulukko. Valon Indusoimien Ja
INTERNET-OHEIS AINEISTON TAULUKKO. Valon indusoimien ja kellokoneiston avainmolekyylien yhteydet sairauksiin. Geeni Eläinmallin ilmiasu Ihmisen sairaus Homer1 Masennus [1] ? Psykoosi [2] Oppimishäiriöt [3] Dementia [4] Nr4a1 Apoptoosin häiriöt [5] Masennus [26] Ylivilkkaus [6] Kaksisuuntainen mielialahäiriö [27] Sokeriaineenvaihdunnan häiriöt [7] Psykoosi [27] Ateroskleroosi [8] Akuutti myelooinen leukemia [28] Dementia [4] Rintasyöpä [29] Eturauhassyöpä [30] Melanooma [31] Alzheimerin tauti [32] Ateroskleroosi [33] Arntl1 Hedelmättömyys [9] Kaamosmasennus [34] Sokeriaineenvaihdunnan häiriöt [10] Kaksisuuntainen mielialahäiriö [35] Rasva-aineenvaihdunnan häiriöt [11] Verenpainetauti [36] Unihäiriöt [12] Tyypin 2 diabetes [36] Artropatia [13] Krooninen myelooinen leukemia [37] Sisäisen kellon arytmia [14] Clock Mania [15] Unihäiriöt [38] Metabolinen oireyhtymä [16] Metabolinen oireyhtymä [39] Kokaiiniriippuvuus [17] Lihavuus [39, 40] Rasvamaksa [41] Psykoosi [42] Npas2 Sisäisen kellon joustamattomuus [18] Kaamosmasennus [34] Muistihäiriöt [19] Non-Hodgkin-lymfooma [43] Rintasyöpä [44] Eturauhassyöpä [45] Autismi [46] Per1 Glukokortikoidituotannon häiriöt [20] Rintasyöpä [47,48] Ei-pienisoluinen keuhkosyöpä [49] Kohtusyöpä [50] Haimasyöpä [51] Krooninen myelooinen leukemia [37] Autismi [46] Per2 Alkoholin suurkulutus [21] Kaamosmasennus [34] Pahanlaatuinen lymfooma [22] Aikaistuneen univaiheen oireyhtymä [52] Endoteelin toimintahäiriöt [23] Akuutti myelooinen leukemia [53] Krooninen myelooinen leukemia [37] Rintasyöpä [47] Cry1, Cry2 Unihäiriöt [24] Krooninen myelooinen leukemia [37] Sokeriaineenvaihdunnan häiriöt [25] Eturauhassyöpä [45] 42 INTERNET-OHEISAINEISTON LÄHTEET 14) Bunger M, Wilsbacher L,Moran S, ym. receptors Nr4a3 and Nr4a1 leads to de- 1) Orsetti M, Di Brisco F, Canonico PL, Mop3 is an essential component of the velopment of acute myeloid leukemia. Genazzani AA, Ghi P. Gene regulation master circadian pacemaker in mam- Nat Med 2007;13:730–5. in the frontal cortex of rats exposed to mals. Cell 200;103:1009–17. -

Tet2 and Tet3 Cooperate with B-Lineage Transcription Factors To
RESEARCH ARTICLE Tet2 and Tet3 cooperate with B-lineage transcription factors to regulate DNA modification and chromatin accessibility Chan-Wang Lio1†, Jiayuan Zhang2†, Edahı´Gonza´ lez-Avalos1, Patrick G Hogan1, Xing Chang1,2,3*, Anjana Rao1,3,4,5* 1Division of Signaling and Gene Expression, San Diego, United States; 2Key Laboratory of Stem Cell Biology, Institute of Health Sciences, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences and Shanghai Jiao Tong University School of Medicine, Shanghai, China; 3Sanford Consortium for Regenerative Medicine, San Diego, United States; 4Department of Pharmacology, University of California, San Diego, San Diego, United States; 5Moores Cancer Center, University of California, San Diego, San Diego, United States Abstract Ten-eleven translocation (TET) enzymes oxidize 5-methylcytosine, facilitating DNA demethylation and generating new epigenetic marks. Here we show that concomitant loss of Tet2 and Tet3 in mice at early B cell stage blocked the pro- to pre-B cell transition in the bone marrow, decreased Irf4 expression and impaired the germline transcription and rearrangement of the Igk locus. Tet2/3-deficient pro-B cells showed increased CpG methylation at the Igk 3’ and distal enhancers that was mimicked by depletion of E2A or PU.1, as well as a global decrease in chromatin accessibility at enhancers. Importantly, re-expression of the Tet2 catalytic domain in *For correspondence: Tet2/3-deficient B cells resulted in demethylation of the Igk enhancers and restored their chromatin [email protected] (XC); arao@ accessibility. Our data suggest that TET proteins and lineage-specific transcription factors lji.org (AR) cooperate to influence chromatin accessibility and Igk enhancer function by modulating the modification status of DNA.