A Complete Solution for Broad Microbial Identification Debbie Boldt-Houle, Ph.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bartonella Apis Sp. Nov., a Honey Bee Gut Symbiont of the Class Alphaproteobacteria
Serveur Academique´ Lausannois SERVAL serval.unil.ch Author Manuscript Faculty of Biology and Medicine Publication This paper has been peer-reviewed but does not include the final publisher proof-corrections or journal pagination. Published in final edited form as: Title: Bartonella apis sp. nov., a honey bee gut symbiont of the class Alphaproteobacteria. Authors: Keˇsnerov´aL, Moritz R, Engel P Journal: International journal of systematic and evolutionary microbiology Year: 2016 Jan Issue: 66 Volume: 1 Pages: 414-21 DOI: 10.1099/ijsem.0.000736 In the absence of a copyright statement, users should assume that standard copyright protection applies, unless the article contains an explicit statement to the contrary. In case of doubt, contact the journal publisher to verify the copyright status of an article. 1 Bartonella apis sp. nov., a honey bee gut symbiont of the 2 class Alphaproteobacteria 3 4 Lucie Kešnerová, Roxane Moritz, Philipp Engel* 5 6 Department of Fundamental Microbiology, University of Lausanne, CH-1015 7 Lausanne, Switzerland 8 9 Running title: Description of a bee gut symbiont 10 11 *Correspondence: 12 Prof. Philipp Engel 13 Department of Fundamental Microbiology 14 University of Lausanne, CH-1015 Lausanne, Switzerland 15 Tel.: +41 (0)21 692 56 12 16 e-mail: [email protected] 17 18 Category: New Taxa – Proteobacteria 19 Keywords: Apis mellifera; insect; Bartonella; gut microbiota; Alpha-1 20 21 Sequence deposition: The 16S rRNA gene sequences and protein-coding gene 22 sequences of the bacterial strains PEB0122T, PEB0149, PEB0150, BBC0104, and 23 BBC0108 from Apis mellifera, and the uncultured Rhizobiales bacterium from 24 Herpagnathos saltator are deposited in GenBank with accession numbers KP987849 25 – KP987886 and KT315729 – KT315734. -
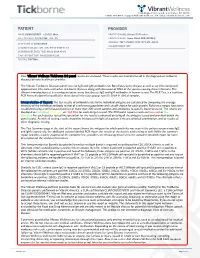
View Tickborne Diseases Sample Report
1360 Bayport Ave, Ste B. San Carlos, CA 94070 1(866) 364-0963 | [email protected] | www. vibrant-wellness.com PATIENT PROVIDER NAME: DEMO REPORT GENDER: Male PRACTICE NAME: Vibrant IT4 Practice DATE OF BIRTH: 04/14/1998 AGE: 22 PROVIDER NAME: Demo Client, DDD (999994) ADDRESS: TEST STREET, TEST CITY, KY- 42437. ACCESSION ID: 2009220006 PHLEBOTOMIST: 607 SPECIMEN COLLECTION TIME: 09-21-2020 11:14 SPECIMEN RECEIVED TIME: 09-22-2020 05:14 FINAL REPORT TIME: 09-25-2020 15:56 FASTING: FASTING Your Vibrant Wellness TickBorne 2.0 panel results are enclosed. These results are intended to aid in the diagnosis of tickborne diseases by your healthcare provider. The Vibrant Tickborne Diseases panel tests for IgG and IgM antibodies for Borreliosis/Lyme disease as well as co-infection(s) and opportunistic infections with other tick-borne illnesses along with detection of DNA of the species causing these infections. The Vibrant Immunochip test is a semiquantitative assay that detects IgG and IgM antibodies in human serum. The PCR Test is a real-time PCR Assay designed for qualitative detection of infectious group- specific DNA in clinical samples. Interpretation of Report: The test results of antibody levels to the individual antigens are calculated by comparing the average intensity of the individual antibody to that of a reference population and cut-off chosen for each protein. Reference ranges have been established using a well characterized set of more than 300 serum samples and antibodies to specific bacteria tested. The results are displayed as In Control, Moderate, or High Risk.for each antigen tested. -

Abstract Pultorak, Elizabeth Lauren
ABSTRACT PULTORAK, ELIZABETH LAUREN. The Epidemiology of Lyme Disease and Bartonellosis in Humans and Animals. (Under the direction of Edward B. Breitschwerdt). The expansion of vector borne diseases in humans, a variety of mammalian hosts, and arthropod vectors draws attention to the need for enhanced diagnostic techniques for documenting infection in hosts, effective vector control, and treatment of individuals with associated diseases. Through improved diagnosis of vector-borne disease in both humans and animals, epidemiological studies to elucidate clinical associations or spatio-temporal relationships can be assessed. Veterinarians, through the use of the C6 peptide in the SNAP DX test kit, may be able to evaluate the changing epidemiology of borreliosis through their canine population. We developed a survey to evaluate the practices and perceptions of veterinarians in North Carolina regarding borreliosis in dogs across different geographic regions of the state. We found that veterinarians’ perception of the risk of borreliosis in North Carolina was consistent with recent scientific reports pertaining to geographic expansion of borreliosis in the state. Veterinarians should promote routine screening of dogs for Borrelia burgdorferi exposure as a simple, inexpensive form of surveillance in this transitional geographic region. We next conducted two separate studies to evaluate Bartonella spp. bacteremia or presence of antibodies against B. henselae, B. koehlerae, or B. vinsonii subsp. berkhoffii in 296 patients examined by a rheumatologist and 192 patients with animal exposure (100%) and recent animal bites and scratches (88.0%). Among 296 patients examined by a rheumatologist, prevalence of antibodies (185 [62%]) and Bartonella spp. bacteremia (122 [41.1%]) was high. -

Detection and Partial Molecular Characterization of Rickettsia and Bartonella from Southern African Bat Species
Detection and partial molecular characterization of Rickettsia and Bartonella from southern African bat species by Tjale Mabotse Augustine (29685690) Submitted in partial fulfillment of the requirements for the degree MAGISTER SCIENTIAE (MICROBIOLOGY) in the Department of Microbiology and Plant Pathology Faculty of Natural and Agricultural Sciences University of Pretoria Pretoria, South Africa Supervisor: Dr Wanda Markotter Co-supervisors: Prof Louis H. Nel Dr Jacqueline Weyer May, 2012 I declare that the thesis, which I hereby submit for the degree MSc (Microbiology) at the University of Pretoria, South Africa, is my own work and has not been submitted by me for a degree at another university ________________________________ Tjale Mabotse Augustine i Acknowledgements I would like send my sincere gratitude to the following people: Dr Wanda Markotter (University of Pretoria), Dr Jacqueline Weyer (National Institute for Communicable Diseases-National Health Laboratory Service) and Prof Louis H Nel (University of Pretoria) for their supervision and guidance during the project. Dr Jacqueline Weyer (Centre for Zoonotic and Emerging diseases (Previously Special Pathogens Unit), National Institute for Communicable Diseases (National Heath Laboratory Service), for providing the positive control DNA for Rickettsia and Dr Jenny Rossouw (Special Bacterial Pathogens Reference Unit, National Institute for Communicable Diseases-National Health Laboratory Service), for providing the positive control DNA for Bartonella. Dr Teresa Kearney (Ditsong Museum of Natural Science), Gauteng and Northern Region Bat Interest Group, Kwa-Zulu Natal Bat Interest Group, Prof Ara Monadjem (University of Swaziland), Werner Marias (University of Johannesburg), Dr Francois du Rand (University of Johannesburg) and Prof David Jacobs (University of Cape Town) for collection of blood samples. -

Anaplasma Platys Diagnosis in Dogs
Anaplasma platys Diagnosis in Dogs: Comparison Between Morphological and Molecular Tests Renata Fernandes Ferreira, VMD, MSc1 Aloysio de Mello Figueiredo Cerqueira, VMD, MSc, DSc2 Ananda Müller Pereira, VMD1 Cecília Matheus Guimarães BSc2 Alexandre Garcia de Sá, VMD, MSc1 Fabricio da Silva Abreu, VMD, MSc1 Carlos Luiz Massard, VMD, MSc, PhD3 Nádia Regina Pereira Almosny, VMD, MSc, PhD1 1Departamento de Patologia e Clínica Veterinária Universidade Federal Fluminense Niterói, Rio de Janeiro, Brazil 2Departamento de Microbiologia e Parasitologia Universidade Federal Fluminense Niterói, Rio de Janeiro, Brazil 3Departamento de Parasitologia Animal Universidade Federal Rural do Rio de Janeiro Seropédica, Rio de Janeiro, Brazil KEY WORDS: Anaplasma platys, PCR, ickettsia helminthoeca (PCR1). The second inclusions stage consisted of the utilization of specific primers for the detection of the species A ABSTRACT platys (PCR2). Upon comparison of the re- Anaplasma platys is related to the appear- sults, 18.81% of the studied animals showed ance of inclusion bodies in blood platelets; positive for PCR1. For PCR2, 15.84% of the however, this may be a nonspecific occur- studied animals had a positive result. In the rence as there are nonparasitic inclusion morphological analysis of the inclusion bod- bodies within these figured elements. Aiming ies, 14.85% of the animals showed positive to validate the morphological diagnosis for for A platys. The other inclusion bodies were A platys, 101 dogs were selected due to the considered as nonspecific, therefore nega- appearance of inclusion bodies, indepen- tive. When compared to the morphological dently from suggestive parasites, which analysis, the results of the molecule analysis were submitted to polymerase chain reac- by means of the MacNemar test led to the tion (PCR) carried out in 2 stages. -

Human Case of Bartonella Alsatica Lymphadenitis
LETTERS (6). The sequence is distinct from a DOI: 10.3201/eid1412.080944 Human Case of small number of sequences derived from rabies viruses in Vietnam, which References Bartonella alsatica suggests that China is a stronger can- Lymphadenitis 1. Smith JS, Fishbein DB, Rupprecht CE, didate for the source of the virus than Clark K. Unexplained rabies in three To the Editor: Lymph node en- her native country. immigrants in the United States: a vi- Although the case history could rologic investigation. N Engl J Med. largement is a common medical prob- not provide evidence for interaction 1991;324:205–11. lem that is usually caused by bacterial, 2. Grattan-Smith PJ, O’Regan WJ, Ellis PS, with a dog while her family was in viral, fungal, or protozoal agents (1). O’Flaherty SJ, McIntyre PB, Barnes CJ. A Malignancies or lymphoproliferative Hong Kong Special Administrative second Australian case, with a long incuba- Region, rabies was endemic within tion period. Med J Aust. 1992;156:651–4. diseases are often found, especially in the colony at the time that the pa- 3. McColl KA, Gould AR, Selleck PW, elderly patients (1). Bartonella hense- Hooper PT, Westbury HA, Smith JS. tient’s family was resident. From 1980 lae, the main causative agent of cat- Polymerase chain reaction and other labo- scratch disease (CSD), appears to be through 1984, 5 human cases were re- ratory techniques in the diagnosis of long corded (9). Only 2 case-patients had incubation rabies in Australia. Aust Vet the most common organism respon- clear evidence of a dog bite; histories J. -

Appendix B the Following List Represents 29 Zoonotic/Anthroponotic Pathogens Denoted As Grey-Zone Pathogens
Appendix B The following list represents 29 zoonotic/anthroponotic pathogens denoted as Grey-Zone Pathogens. These represent any pathogen where there is some evidence the dog is involved in transmission, maintenance or detection of the pathogen, but current research has not definitively proven the dog’s role at the time of this study. There were no sapronoses in this group. Of these pathogens, those that have been reported in Canada are marked with a 1. Those pathogens that have the potential to occur in Canada but have not yet been reported are marked with a 2. Bacteria Protozoa Acinetobacter baumannii 1 Babesia canis canis Borrelia turicatae 1 Babesia canis rossi Campylobacter gracilis 1 Babesia canis vogeli 1 Campylobacter lari 1 Blastocystis hominis 1 Helicobacter bizzozeronii 2 Blastocystis spp. 1 Mycoplasma canis 2 Cryptosporidium parvum 1 Mycoplasma maculosum 2 Leishmania donovani 1 Rhodococcus equi 1 Staphylococcus schleiferi coagulans Rickettsia Anaplasma platys 1 Fungi Ehrlichia chaffeensis 2 Encephalitozoon cuniculi 1 Ehrlichia ewingii 2 Encephalitozoon intestinalis 2 Enterocytozoon bieneusi 2 Viruses Reovirus MRV (Mammalian Reovirus) serotype 1 1 Helminths Reovirus MRV (Mammalian Reovirus) serotype 2 1 Ascaris lumbricoides 1 Reovirus MRV (Mammalian Reovirus) serotype 3 1 Trichinella spiralis 1 West Nile virus1 Trichuris vulpis 1 Only a portion of the information obtained in this study is presented here. Please contact the authors for additional reference material on why a pathogen was or was not included in a particular step. Appendix C The following list represents 74 zoonotic/sapronotic pathogens where the dog is involved in transmission, maintenance, or detection of the pathogen and the pathogen has been reported to have historically occurred in Canada, however, Canadian canine-specific reports are lacking (Tier 2). -

Molecular Detection and Identification of Rickettsiales Pathogens in Dog Ticks from Costa Rica
Accepted Manuscript Title: Molecular detection and identification of Rickettsiales pathogens in dog ticks from Costa Rica Author: Liliana Campos-Calderon´ Leyda Abrego-S´ anchez´ Antony Solorzano-Morales´ Alberto Alberti Gessica Tore Rosanna Zobba Ana E. Jimenez-Rocha´ Gaby Dolz PII: S1877-959X(16)30120-0 DOI: http://dx.doi.org/doi:10.1016/j.ttbdis.2016.07.015 Reference: TTBDIS 700 To appear in: Received date: 29-2-2016 Revised date: 1-7-2016 Accepted date: 24-7-2016 Please cite this article as: Campos-Calderon,´ Liliana, Abrego-S´ anchez,´ Leyda, Solorzano-Morales,´ Antony, Alberti, Alberto, Tore, Gessica, Zobba, Rosanna, Jimenez-Rocha,´ Ana E., Dolz, Gaby, Molecular detection and identification of Rickettsiales pathogens in dog ticks from Costa Rica.Ticks and Tick-borne Diseases http://dx.doi.org/10.1016/j.ttbdis.2016.07.015 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. Molecular detection and identification of Rickettsiales pathogens in dog ticks from Costa Rica Liliana Campos-Calderóna, Leyda Ábrego-Sánchezb, Antony Solórzano- Moralesa, Alberto Albertic, Gessica Torec, Rosanna Zobbac, Ana E. Jiménez- Rochaa, Gaby Dolza,b,* aEscuela de Medicina Veterinaria, Universidad Nacional, Campus Benjamín Núñez, Barreal de Heredia, Costa Rica ([email protected], [email protected], [email protected]). -

Tick-Borne Pathogens in Removed Ticks Veneto, Northeastern Italy
Tick-borne pathogens in removed ticks Veneto, northeastern Italy: A cross-sectional investigation Anna Beltrame, Maureen Laroche, Monica Degani, Francesca Perandin, Zeno Bisoffi, Didier Raoult, Philippe Parola To cite this version: Anna Beltrame, Maureen Laroche, Monica Degani, Francesca Perandin, Zeno Bisoffi, et al.. Tick- borne pathogens in removed ticks Veneto, northeastern Italy: A cross-sectional investigation. Travel Medicine and Infectious Disease, Elsevier, 2018, 26, pp.58-61. 10.1016/j.tmaid.2018.08.008. hal- 01970220 HAL Id: hal-01970220 https://hal.archives-ouvertes.fr/hal-01970220 Submitted on 10 Apr 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Travel Medicine and Infectious Disease 26 (2018) 58–61 Contents lists available at ScienceDirect Travel Medicine and Infectious Disease journal homepage: www.elsevier.com/locate/tmaid Tick-borne pathogens in removed ticks Veneto, northeastern Italy: A cross- sectional investigation T ∗ Anna Beltramea, , Maureen Larocheb, Monica Degania, Francesca Perandina, Zeno Bisoffia, Didier Raoultc, Philippe Parolab a Centre for Tropical Diseases, IRCCS Sacro Cuore Don Calabria Hospital, Via Sempreboni 5, 37024, Negrar, Italy b Aix Marseille Univ, AP-HM, SSA, VITROME, IHU-Méditerranée Infection, 19-21 Bd Jean Moulin, 13005, Marseille, France c Aix Marseille Univ, AP-HM, MEPHI, IHU-Méditerranée Infection, 19-21 Bd Jean Moulin, 13005, Marseille, France ARTICLE INFO ABSTRACT Keywords: Background: In Italy, the incidence of tick-borne diseases in humans is underestimated, as they are not ob- Tick-borne diseases ligatorily notifiable. -
Molecular Detection of Tick-Borne Pathogen Diversities in Ticks From
ORIGINAL RESEARCH published: 01 June 2017 doi: 10.3389/fvets.2017.00073 Molecular Detection of Tick-Borne Pathogen Diversities in Ticks from Livestock and Reptiles along the Shores and Adjacent Islands of Lake Victoria and Lake Baringo, Kenya David Omondi1,2,3, Daniel K. Masiga1, Burtram C. Fielding 2, Edward Kariuki 4, Yvonne Ukamaka Ajamma1,5, Micky M. Mwamuye1, Daniel O. Ouso1,5 and Jandouwe Villinger 1* 1International Centre of Insect Physiology and Ecology (icipe), Nairobi, Kenya, 2 University of Western Cape, Bellville, South Africa, 3 Egerton University, Egerton, Kenya, 4 Kenya Wildlife Service, Nairobi, Kenya, 5 Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya Although diverse tick-borne pathogens (TBPs) are endemic to East Africa, with recog- nized impact on human and livestock health, their diversity and specific interactions with Edited by: tick and vertebrate host species remain poorly understood in the region. In particular, Dirk Werling, the role of reptiles in TBP epidemiology remains unknown, despite having been impli- Royal Veterinary College, UK cated with TBPs of livestock among exported tortoises and lizards. Understanding TBP Reviewed by: Timothy Connelley, ecologies, and the potential role of common reptiles, is critical for the development of University of Edinburgh, UK targeted transmission control strategies for these neglected tropical disease agents. Abdul Jabbar, University of Melbourne, Australia During the wet months (April–May; October–December) of 2012–2013, we surveyed Ria Ghai, TBP diversity among 4,126 ticks parasitizing livestock and reptiles at homesteads along Emory University, USA the shores and islands of Lake Baringo and Lake Victoria in Kenya, regions endemic *Correspondence: to diverse neglected tick-borne diseases. -

Co-Infection of Bacteria and Protozoan Parasites in Ixodes Ricinus Nymphs Collected in the Alsace Region, France
Ticks and Tick-borne Diseases 10 (2019) 101241 Contents lists available at ScienceDirect Ticks and Tick-borne Diseases journal homepage: www.elsevier.com/locate/ttbdis Short communication Co-infection of bacteria and protozoan parasites in Ixodes ricinus nymphs T collected in the Alsace region, France Amira Nebbaka,b, Handi Dahmanaa, Lionel Almerasa,c, Didier Raoultd, Nathalie Boulangere,f, ⁎ Benoit Jaulhace,f, Oleg Mediannikovd, Philippe Parolaa,d, a Aix Marseille Univ, IRD, AP-HM, SSA, VITROME, Marseille, France b Centre de Recherche Scientifique et Technique en Analyses Physico-Chimiques (CRAPC). Zone Industrielle, BP 384 Bou-Ismail, Tipaza Algeria c Unité de Parasitologie et Entomologie, Département des Maladies Infectieuses, Institut de Recherche Biomédicale des Armées, Marseille, France d IHU-Méditerranée Infection, Marseille, France e Centre National de Reference Borrelia, Centre Hospitalier Universitaire, Strasbourg, France f EA7290Virulence bactérienne précoce: groupe borréliose de Lyme, Facultés de pharmacie et de médecine, Université de Strasbourg, France ARTICLE INFO ABSTRACT Keywords: Fifty nymphal Ixodes ricinus ticks collected in Alsace, France, identified by morphological criteria and using Ixodes ricinus MALDI-TOF MS, were tested by PCR to detect tick-associated bacteria and protozoan parasites. Seventy percent Co-infection (35/50) of ticks contained at least one microorganism; 26% (9/35) contained two or more species. Several Bacterial pathogens human pathogens were identified including Borrelia burgdorferi s.s. (4%), Borrelia afzelii (2%), Borrelia garinii Protozoan parasites (2%), Borrelia valaisiana (4%), Borrelia miyamotoi (2%), Rickettsia helvetica (6%) and “Babesia venatorum” (2%). MALDI-TOF MS Bartonella spp. (10%) and a Wolbachia spp. (8%) were also detected. The most common co-infections involved Anaplasmataceae with Borrelia spp. -

Exploration of Tick-Borne Pathogens and Microbiota of Dog Ticks Collected at Potchefstroom Animal Welfare Society
Exploration of tick-borne pathogens and microbiota of dog ticks collected at Potchefstroom Animal Welfare Society C Van Wyk orcid.org 0000-0002-5971-4396 Dissertation submitted in fulfilment of the requirements for the degree Master of Science in Environmental Sciences at the North-West University Supervisor: Prof MMO Thekisoe Co-supervisor: Ms K Mtshali Graduation May 2019 24263524 DEDICATION This thesis is dedicated to the late Nettie Coetzee. For her inspiration and lessons to overcome any obstacle that life may present. God called home another angel we all love and miss you. “We are the scientists, trying to make sense of the stars inside us.” -Christopher Poindexter i ACKNOWLEDGEMENTS My sincerest appreciation goes out to my supervisor, Prof. Oriel M.M. Thekisoe, for his support, motivation, guidance, and insightfulness during the duration of this project and been there every step of the way. I would also like to thank my co-supervisor, Ms. Khethiwe Mtshali, for her patience and insightfulness towards the corrections of this thesis. I would like to thank Dr. Stalone Terera and the staff members at PAWS for their aid towards the collection of tick specimens. For the sequencing on the Illumina MiSeq platform and metagenomic data analysis I would like to thank Dr. Moeti O. Taioe, Dr. Charlotte M.S. Mienie, Dr. Danie C. La Grange, and Dr. Marlin J. Mert. I would like to thank the National Research Foundation (NRF) for their financial support by awarding me the S&F- Innovation Masters Scholarship and the North-West University (NWU) for the use of their laboratories.