Clinicopathological Evaluations of Cervical Polyps
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Cervical Polypectomy
Cervical Polypectomy Author: Consultant Department: Gynaecology/ Colposcopy Document Number: STHK1225 Version: 4 Review date: 01/10/2022 What is a polyp? Your doctor/nurse has advised you to have a polypectomy, which is the removal of a polyp. A polyp is a flesh-like structure (often described as looking like a cherry on a stalk or a skin tag), which can develop in many places in the body, including the cervix and uterus. It may have blood vessels running through it, which can often be the cause of bleeding. If it is thought the polyp is in your uterus, you will need to have a hysteroscopy (a procedure that uses a narrow camera to look inside the cavity of the uterus). This procedure is carried out as a gynaecology outpatient appointment at the Women’s Centre, and is performed in a special clinic in the Diagnostic Suite. You will receive a further appointment for this treatment and be given a different leaflet to explain the hysteroscopy procedure. If for any reason the polyp cannot be removed or fully removed during either of these treatments, the doctor will advise you of other options. Reasons for the procedure As you know you have been referred to the Colposcopy Clinic because you have a polyp on the cervix. Sometimes the cervical polyp is broad based, where it does not have a stalk but sits on the cervix. Often they cause no symptoms and are found as a result of other examinations. Polyps are usually benign (non-cancerous). Less than 1 % (1 in 100) may have pre-cancerous or cancerous changes within them; it is therefore advisable to have them removed. -

ICD-9-CM and ICD-10-CM Codes for Gynecology and Obstetrics
Diagnostic Services ICD-9-CM and ICD-10-CM Codes for Gynecology and Obstetrics ICD-9 ICD-10 ICD-9 ICD-10 Diagnoses Diagnoses Code Code Code Code Menstral Abnormalities 622.12 Moderate Dysplasia Of Cervix (CIN II) N87.2 625.3 Dysmenorrhea N94.6 Menopause 625.4 Premenstrual Syndrome N94.3 627.1 Postmenopausal Bleeding N95.0 626.0 Amenorrhea N91.2 627.2 Menopausal Symptoms N95.1 626.1 Oligomenorrhea N91.5 627.3 Senile Atrophic Vaginitis N95.2 626.2 Menorrhagia N92.0 627.4 Postsurgical Menopause N95.8 626.4 Irregular Menses N92.6 627.8 Perimenopausal Bleeding N95.8 626.6 Metrorrhagia N92.1 Abnormal Pap Smear Results 626.8 Dysfunctional Uterine Bleeding N93.8 795.00 Abnormal Pap Smear Result, Cervix R87.619 Disorders Of Genital Area 795.01 ASC-US, Cervix R87.610 614.9 Pelvic Inflammatory Disease (PID) N73.9 795.02 ASC-H, Cervix R87.611 616.1 Vaginitis, Unspecified N76.0 795.03 LGSIL, Cervix R87.612 616.2 Bartholin’s Cyst N75.0 795.04 HGSIL, Cervix R87.613 Cervical High-Risk HPV DNA 616.4 Vulvar Abscess N76.4 795.05 R87.810 Test Positive 616.5 Ulcer Of Vulva N76.6 Unsatisfactory Cervical 795.08 R87.615 616.89 Vaginal Ulcer N76.5 Cytology Sample 623.1 Leukoplakia Of Vagina N89.4 795.10 Abnormal Pap Smear Result, Vagina R87.628 Vaginal High-Risk HPV DNA 623.5 Vaginal Discharge N89.8 795.15 R87.811 Test Positive 623.8 Vaginal Bleeding N93.9 Disorders Of Uterus And Ovary 623.8 Vaginal Cyst N89.8 218.9 Uterine Fibroid/Leiomyoma D25.9 Noninflammatory Disorder 623.9 N89.9 Of Vagina 256.39 Ovarian Failure E28.39 624.8 Vulvar Lesion N90.89 256.9 Ovarian -

Having a Cervical Polypectomy
Gynaecology information Having a cervical polypectomy Introduction This leaflet gives you advice and information about having a cervical polypectomy (removal of polyps from the neck of the womb). Please read it before you go home so that you can have your questions answered before you leave. Feel free to discuss any questions or concerns with your nurse or telephone the Colposcopy Clinic on 0118 322 7197 or Sonning Ward on: 0118 322 7181. What is a cervical polypectomy and why do I need one? A cervical polyp is a small piece of tissue, usually on a stalk, that grows on the cervix (neck of the womb). Sometimes the cervical polyp is broad-based, where it does not have a stalk but sits on the cervix. Often they cause no symptoms and are found as a result of other examinations. Polyps are usually benign (non-cancerous). Less than 1% may have pre- cancerous or cancerous changes within them; it is therefore advisable to have them removed. A polypectomy is the removal of polyps. What are the risks of a cervical polypectomy? The procedure is very low risk, but may cause an infection or heavier bleeding. Before being sent for a polypectomy your doctor will have carried out a full pelvic examination, including an examination of your cervix using a speculum and you may have had an ultrasound or scan. What happens during a cervical polypectomy? This is normally done in the outpatient clinic. You will be asked to undress from the waist down and lie down on an examination couch. A speculum (the instrument used to open up the vagina) is passed into the vagina to expose the cervix. -

Menstrual Disorder
Menstrual Disorder N.SmidtN.Smidt--AfekAfek MD MHPE Lake Placid January 2011 The Menstrual Cycle two phases: follicular and luteal Normal Menstruation Regular menstruation 28+/28+/--7days;7days; Flow 4 --7d. 40ml loss Menstrual Disorders Abnormal Beleding –– Menorrhagia ,Metrorrhagia, Polymenorrhagia, Oligomenorrhea, Amenorrhea -- Dysmenorrhea –– Primary Dysmenorrhea, secondary Dysmenorrhea Pre Menstrual Tension –– PMD, PMDD Abnormal Uterine Beleeding Abnormal Bleeding Patterns Menorrhagia --bleedingbleeding more than 80ml or lasting >7days Metrorrhagia --bleedingbleeding between periods Polymenorrhagia -- menses less than 21d apart Oligomenorrhea --mensesmenses greater than 35 dasy apart. (in majority is anovulatory) Amenorrhea --NoNo menses for at least 6months Dysfunctional Uterine Bleeding Clinical term referring to abnormal bleeding that is not caused by identifiable gynecological pathology "Anovulatory Uterine Bleeding“ is usually the cause Diagnosis of exclusion Anovulatory Bleeding Most common at either end of reproductive life Chronic spotting Intermittent heavy bleeding Post Coital Bleeding Cervical ectropion ( most common in pregnancy) Cervicitis Vaginal or cervical malignancy Polyp Common Causes by age Neonatal Premenarchal ––EstrogenEstrogen withdrawal ––ForeignForeign body ––Trauma,Trauma, including sexual abuse Infection ––UrethralUrethral prolapse ––Sarcoma botryoides ––Ovarian tumor ––PrecociousPrecocious puberty Common Causes by age Early postmenarche Anovulation (hypothalamic immaturity) Bleeding -

A Giant, Deceptive Cervical Polyp
Interventions in Gynaecology & Women’s Healthcare DOI: 10.32474/IGWHC.2020.04.000183 ISSN: 2637-4544 Case Report A Giant, Deceptive Cervical Polyp Mounia Bennani*, Hanane Baybay, Jihane Ziani, Sara Elloudi, Zakia Douhi and Fatima Zahra Mernissi Department of dermatology and venerology, Hassan II hospital university, Morocco *Corresponding author: Mounia Bennani Department of dermatology and venerology, Hassan II Hospital University, FES Received: February 29,2020 Published: March 05, 2020 Case Report This is the case of a 48-year-old patient, no Medical or pink-reddish, with a smooth surface (Figure 2), the vaginal touch pharmacological history referred in Our dermatology consultation protruding through the vagina (Figure1). The mass was firm, the tumor was in continuity with the cervix, while the vulva was for management of a lesion evolving for 6 years, increasing in intact. A dermoscopic examination was carried out objectifying size, becoming bleeding on contact, the patient did not complain the presence of a polymorphic vascularization made of vessels in of pain, but rather an unpleasant feeling of heaviness. On local points, irregular linear, and hairpins in place, associated with the examination, a multi-lobed tumor of approximately 10 cm was presence of bright white areas without structures (Figure 3). Figure 1: Image showing a 10cm Multilobed tumor protruding through the vagina. Copyright © All rights are reserved by Mounia Bennani. 384 Int Gyn & Women’s Health Volume 4 - Issue 2 Copyrights @ Mounia Bennani. Figure 2: Image showing a firm, pinkish-reddish, multiloped mass with a smooth surface. Figure 3: Dermoscopic image showing polymorphic vascularity and bright white structures. -

The Woman with Postmenopausal Bleeding
THEME Gynaecological malignancies The woman with postmenopausal bleeding Alison H Brand MD, FRCS(C), FRANZCOG, CGO, BACKGROUND is a certified gynaecological Postmenopausal bleeding is a common complaint from women seen in general practice. oncologist, Westmead Hospital, New South Wales. OBJECTIVE [email protected]. This article outlines a general approach to such patients and discusses the diagnostic possibilities and their edu.au management. DISCUSSION The most common cause of postmenopausal bleeding is atrophic vaginitis or endometritis. However, as 10% of women with postmenopausal bleeding will be found to have endometrial cancer, all patients must be properly assessed to rule out the diagnosis of malignancy. Most women with endometrial cancer will be diagnosed with early stage disease when the prognosis is excellent as postmenopausal bleeding is an early warning sign that leads women to seek medical advice. Postmenopausal bleeding (PMB) is defined as bleeding • cancer of the uterus, cervix, or vagina (Table 1). that occurs after 1 year of amenorrhea in a woman Endometrial or vaginal atrophy is the most common cause who is not receiving hormone therapy (HT). Women of PMB but more sinister causes of the bleeding such on continuous progesterone and oestrogen hormone as carcinoma must first be ruled out. Patients at risk for therapy can expect to have irregular vaginal bleeding, endometrial cancer are those who are obese, diabetic and/ especially for the first 6 months. This bleeding should or hypertensive, nulliparous, on exogenous oestrogens cease after 1 year. Women on oestrogen and cyclical (including tamoxifen) or those who experience late progesterone should have a regular withdrawal bleeding menopause1 (Table 2). -

Pregnancy Complicated with a Giant Endocervical Polyp
Pregnancy complicated with a giant endocervical polyp Kirbas A, Biberoglu E, Timur H, Uygur D, Danisman N Zekai Tahir Burak Women's Health Education and Research Hospital, Ankara, Turkey Objective We report the case of a giant cervical polyp in a primigravid young women that was associated cervical funneling. Methods Case report. Results A 21 year old primigravid woman admitted to our clinic with suspicion of cervical incompetence at 22 weeks of gestation. She complained of light vaginal bleeding and a vaginal mass. She did not have any pain. Her past medical history was uneventful. A detailed abdominal 2D ultrasound scan was performed to verify the presence of the pregnancy and research for associated anomalies. The US scan showed a 22 week viable fetus. Additionally, there was funneling of the cervical canal and the cervical length was 22 mm (Figure 1). On vaginal examination, there was light bleeding and a large fragile mass protruding from the vagina (Figure 2). We detected that the mass originated from the anterior lip of the cervix and it was extending into the cervical canal (Figure 3). We performed simple polypectomy. The funneling of the cervical canal disappeared after the operation and cervical canal length was 31 mm. The final histopathological findings confirmed a benign giant cervical polyp. The pregnancy is progressing well with a normal cervical length and she is currently 34 weeks of gestation. There has been no recurrence. We have planned endometrial and cervical canal evaluation after delivery. Conclusion Cervical polyps less than 2cm are quite common in the female adult population. -

The Uterus and the Endometrium Common and Unusual Pathologies
The uterus and the endometrium Common and unusual pathologies Dr Anne Marie Coady Consultant Radiologist Head of Obstetric and Gynaecological Ultrasound HEY WACH Lecture outline Normal • Unusual Pathologies • Definitions – Asherman’s – Flexion – Osseous metaplasia – Version – Post ablation syndrome • Normal appearances – Uterus • Not covering congenital uterine – Cervix malformations • Dimensions Pathologies • Uterine – Adenomyosis – Fibroids • Endometrial – Polyps – Hyperplasia – Cancer To be avoided at all costs • Do not describe every uterus with two endometrial cavities as a bicornuate uterus • Do not use “malignancy cannot be excluded” as a blanket term to describe a mass that you cannot categorize • Do not use “ectopic cannot be excluded” just because you cannot determine the site of the pregnancy 2 Endometrial cavities Lecture outline • Definitions • Unusual Pathologies – Flexion – Asherman’s – Version – Osseous metaplasia • Normal appearances – Post ablation syndrome – Uterus – Cervix • Not covering congenital uterine • Dimensions malformations • Pathologies • Uterine – Adenomyosis – Fibroids • Endometrial – Polyps – Hyperplasia – Cancer Anteflexed Definitions 2 terms are described to the orientation of the uterus in the pelvis Flexion Version Flexion is the bending of the uterus on itself and the angle that the uterus makes in the mid sagittal plane with the cervix i.e. the angle between the isthmus: cervix/lower segment and the fundus Anteflexed < 180 degrees Retroflexed > 180 degrees Retroflexed Definitions 2 terms are described -
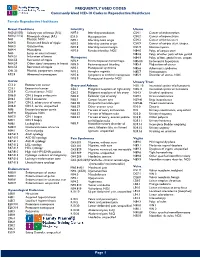
Commonly Used ICD-10 Codes in Reproductive Healthcare
FREQUENTLY USED CODES Commonly Used ICD-10 Codes in Reproductive Healthcare Female Reproductive Healthcare Breast Conditions Infertility Uterus N60.(01/02) Solitary cyst of breast (R/L) N97.0 Infertility-anovulation C54.1 Cancer of endometrium N60.(11/12) Fibrocystic change (R/L) E23.0 Hypopituarism C54.2 Cancer of myometrium N61 Mastitis, NOS N97.1 Infertility-tubal origin C54.3 Cancer of fundus uteri N64.0 Fissure and fistula of nipple N97.2 Infertility-uterine origin C54.9 Cancer of corpus uteri, unspec. N64.3 Galactorrhea N97.8 Infertility-cervical origin D25.9 Uterine myoma N64.4 Mastodynia N97.9 Female infertility, NOS N84.0 Polyp of corpus uteri N63 Lump or mass in breast N84.8 Polyp of other parts of fem genital N64.51 Induration of breast Menopause N84.9 Polyptract of fem. genital tract, unspec. N64.53 Retraction of nipple N92.4 Perimenopausal menorrhagia N85.00 Endometrial hyperplasia N64.59 Other signs/ symptoms in breast N95.0 Postmenopausal bleeding N85.4 Malposition of uterus N64.53 Retraction of nipple N95.1 Menopausal syndrome N85.6 Asherman’s syndrome O91.23 Mastitis, postpartum, unspec. N95.2 Atrophic vaginitis N85.7 Hematometra R92.8 Abnormal mammogram N95.8 Symptoms w artificial menopause N85.9 Disorder of uterus, NOS N95.9 Menopausal disorder NOS Cervix Urinary Tract C53.0 Endocervical cancer Ovary and Adnexa N30. 10 Interstitial cystitis w/o hematuria C53.1 Exocervical cancer C56.1 Malignant neoplasm of right ovary N30.11 Interstitial cystitis w/ hematuria C53.9 Cervical cancer, NOS C56.2 Malignant neoplasm of left -

Removal of Cervical Polyp in the Outpatient Department
Removal of cervical polyp in the outpatient department. This leaflet aims to answer your questions about having a cervical polyp removed. It explains the benefits, risks and what you can expect when you come to hospital. If you have any further questions, please speak to a Doctor or Nurse caring for you. What is a cervical polyp? A polyp is a growth of tissue from either the outside of the cervix (neck of the womb) or inside the cervical canal (the passage between the vagina and the womb). Polyp are usually benign (not cancerous) and can be removed quite easily. There are often no symptoms and the polyp will only be noticed when a woman has had a smear test. However, some polyps can cause bleeding after sexual intercourse, bleeding between periods, bleeding after the menopause or discharge. What are the benefits of removing a polyp? A small percentage of polyps are abnormal and may develop into a cancer if left untreated. Removing the polyp should make symptoms such as bleeding after sexual intercourse or in between periods return to normal. A polyp sometimes makes it difficult to take an adequate smear test. If left a polyp may continue to grow. What happens during the procedure to remove the polyp? Cervical polyps are removed with an instrument called polyp forceps. The instrument is used to grasp the base for the polyp and the polyp is removed with a gentle twisting motion. Occasionally, if the polyp is large or broad based this will be removed under local anesthetic. The polyp is then sent to the laboratory for examination. -

Giant Cervical Polyps: Report of Two Cases and Literature Review
■ SHORT COMMUNICATION ■ GIANT CERVICAL POLYPS: REPORT OF TWO CASES AND LITERATURE REVIEW Wen-Yih Wu, Bor-Ching Sheu, Ho-Hsiung Lin* Department of Obstetrics and Gynecology, National Taiwan University College of Medicine and National Taiwan University Hospital, Taipei, Taiwan. SUMMARY Objective: We report two patients with benign giant cervical polyps. Case Reports: A 47-year-old multiparous woman complained of a protruding mass from her vagina for 6 months. On pelvic examination, there was a large cervical polyp measuring 7 = 2.5 cm arising from the endocervix. The polyp was excised by electrocauterization at the base. The pathological report revealed no evidence of malignancy in the polyp. A 45-year-old nulligravid woman suffered from menorrhagia for 2 months and a mass protruding from the vagina was noted for 10 days. On pelvic examination, there were two cervical polyps. One was 5 = 2 cm and arose from the posterior lip of the cervix and the other was 1 = 1 cm and arose from the right lateral lip. The polyps were excised by electrocauterization. The pathological report revealed benign cervical polyps. Conclusion: Giant cervical polyp is uncommon and malignancy has not been reported in the 11 cases in the literature. Excision was adequate for these lesions. [Taiwanese J Obstet Gynecol 2005;44(1):65–68] Key Words: cervical disease, cervical polyp Introduction are usually found at gynecologic pelvic examination. They are also found in women who present for evalua- Cervical polyps are relatively common lesions and most tion of intermenstrual or postcoital bleeding and for commonly present in perimenopausal and multigravid profuse vaginal discharge. -

Cervical Polypectomy During Pregnancy: Is There Any Management Advances on the Last Decades? C Panayotidis, a Alhuwalia
The Internet Journal of Gynecology and Obstetrics ISPUB.COM Volume 5 Number 1 Cervical Polypectomy During Pregnancy: Is There Any Management Advances On The Last Decades? C Panayotidis, A Alhuwalia Citation C Panayotidis, A Alhuwalia. Cervical Polypectomy During Pregnancy: Is There Any Management Advances On The Last Decades?. The Internet Journal of Gynecology and Obstetrics. 2004 Volume 5 Number 1. Abstract The diagnosis of a cervical polyp during pregnancy is not an uncommon condition. These polyps can give concern to the pregnant woman despite their benign nature in the majority of cases. The management depends on the symptoms. Most of the time, conservative approach is preferred. This article summarises the essential points of the current management and gives a recent review of literature of cervical polypectomy during pregnancy. INTRODUCTION NATURE OF POLYPS The diagnosis of a cervical polyp during pregnancy is not an When a polyp is found during pregnancy the examination uncommon condition. These polyps can give concern to the must be thorough in order to exclude malignancy. Most pregnant woman despite their benign nature in the majority polyps are small, less than 2 centimetres long. Because rare of cases. Protruded cervical polyps out of the vulva are rare types of cancerous conditions can look like polyps, all and their management depends on the symptoms. Most of polyps should be removed and examined to exclude the time, conservative approach is preferred only for small malignancy. The polyps are usually cherry-red to reddish- polyps. purple or greyish-white. They vary in size and often look like bulbs on thin stems.