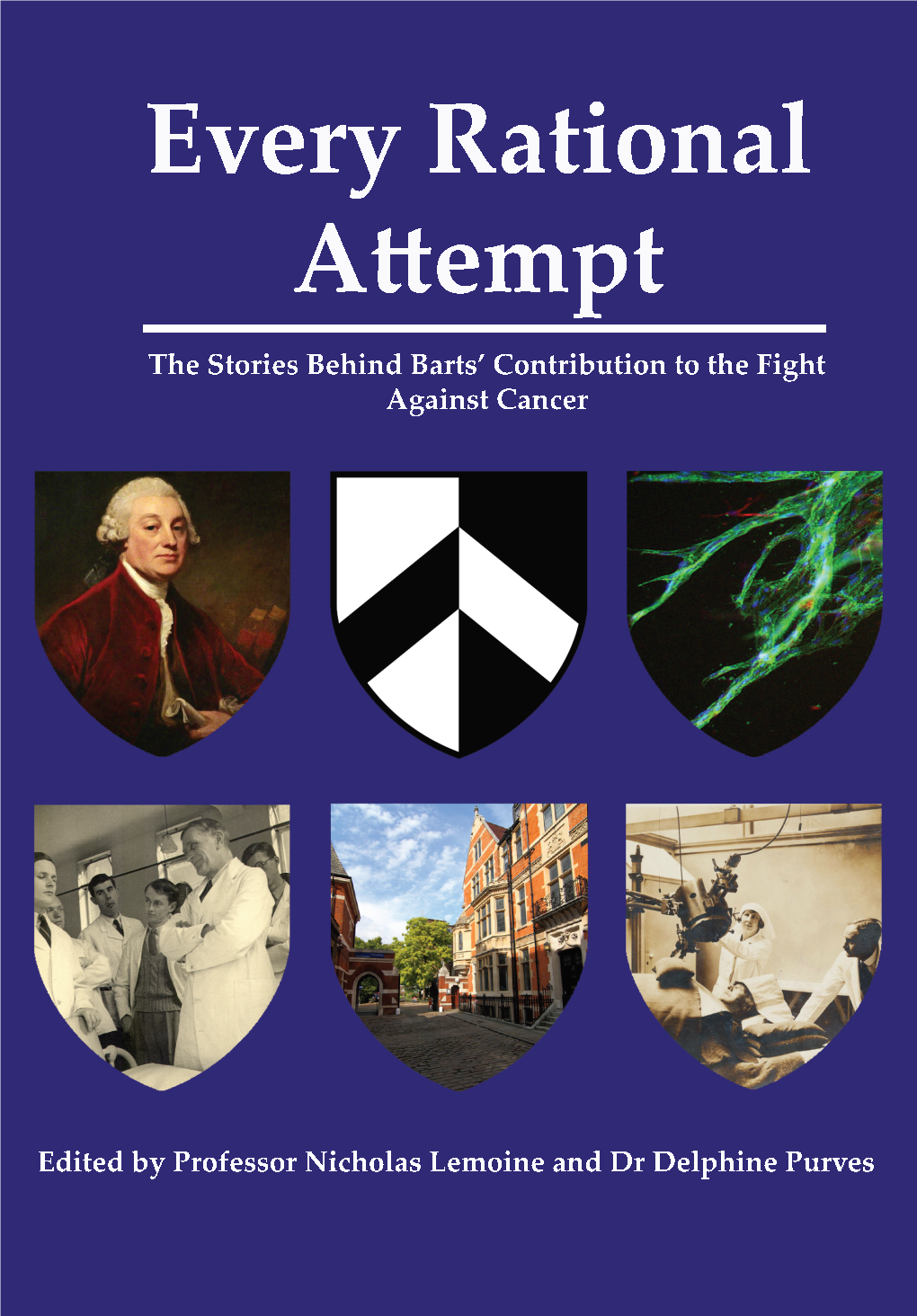
Every Rational Attempt: the Stories Behind the Contribution of Barts in the Fight Against Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE LONDON CHARTERHOUSE Charterhouse Square London EC1
THE LONDON CHARTERHOUSE Charterhouse Square London EC1 London Borough of Islington Historic environment assessment September 2014 © Museum of London Archaeology 2014 Museum of London Archaeology Mortimer Wheeler House 46 Eagle Wharf Road, London N1 7ED tel 020 7410 2200 | fax 020 410 2201 www.museumoflondonarchaeology.org.uk general enquiries: [email protected] THE LONDON CHARTERHOUSE Charterhouse Square London EC1 An historic environment assessment NGR 531945181975 Sign-off history: Issue Date: Prepared by: Checked by Approved by: Reason for Issue: No. 1 16.12.2013 Pat Miller Jon Chandler Laura O’Gorman First issue (Archaeology) Lead Consultant Assistant Project Juan Fuldain Manager (Graphics) 2 15.01.2014 Coralie Acheson - Laura O’Gorman Updated following (Archaeology) client comment 3 12.09.2014 Laura O’Gorman - Laura O’Gorman Separating out planning policy chapter into separate document Finance code:P0072 Museum of London Archaeology Mortimer Wheeler House, 46 Eagle Wharf Road, London N1 7ED tel 0207 410 2200 fax 0207 410 2201 email:[email protected] Museum of London Archaeology is a company limited by guarantee registered in England and Wales with company registration number 07751831 and charity registration number 1143574. Registered office: Mortimer Wheeler House, 46 Eagle Wharf Road, London N1 7ED Historic environment assessment MOLA 2013 Contents Executive summary 1 1 Introduction 2 1.1 Origin and scope of the report 2 1.2 Designated heritage assets 2 1.3 Aims and objectives 3 2 Methodology and sources consulted -
Guardian and Observer Editorial
Monday 01.01.07 Monday The year that changed our lives Swinging with Tony and Cherie Are you a malingerer? Television and radio 12A Shortcuts G2 01.01.07 The world may be coming to an end, but it’s not all bad news . The question First Person Are you really special he news just before Army has opened prospects of a too sick to work? The events that made Christmas that the settlement of a war that has 2006 unforgettable for . end of the world is caused more than 2 million people nigh was not, on the in the north of the country to fl ee. Or — and try to be honest here 4 Carl Carter, who met a surface, an edify- — have you just got “party fl u”? ing way to conclude the year. • Exploitative forms of labour are According to the Institute of Pay- wonderful woman, just Admittedly, we’ve got 5bn years under attack: former camel jockeys roll Professionals, whose mem- before she flew to the before the sun fi rst explodes in the United Arab Emirates are to bers have to calculate employees’ Are the Gibbs watching? . other side of the world and then implodes, sucking the be compensated to the tune of sick pay, December 27 — the fi rst a new year’s kiss for Cherie earth into oblivion, but new year $9m, and Calcutta has banned day back at work after Christmas 7 Karina Kelly, 5,000,002,007 promises to be rickshaw pullers. That just leaves — and January 2 are the top days 16 and pregnant bleak. -

Geriatric Medicine
Programme Programme identifier – F1 Trust Site F1-1 F1-2 F1-3 Programme identifier – F2 Trust Site F2-1 F2-2 F2-3 Type Barking, Havering and Redbridge Gastroenterology - (Medicine) [Acute] {KING GEORGE Geriatric Medicine - (Medicine) [Acute] {KING GEORGE General Surgery - (Surgery) [Acute] {KING GEORGE NEWHAM GENERAL HOSPITAL Emergency Medicine - (Other) [Acute] {NEWHAM Obstetrics and Gynaecology - (Other) [Acute] {NEWHAM Cardiology - (Medicine) [Acute] {NEWHAM GENERAL Standard 20/LDN/BHRKG/F1/001 KING GEORGE HOSPITAL (RF4DG) 21/LDN/BHNEW/F2/007 BARTS HEALTH NHS TRUST University Hospitals NHS Trust HOSPITAL (RF4DG) LDN/RF4DG/FND/FY1/018} HOSPITAL (RF4DG) LDN/RF4DG/FND/FY1/006} HOSPITAL (RF4DG) LDN/RF4DG/FND/FY1/003} (R1HNH) GENERAL HOSPITAL (R1HNH) LDN/R1HNH/FND/FY2/012} GENERAL HOSPITAL (R1HNH) LDN/R1HNH/FND/FY2/025} HOSPITAL (R1HNH) LDN/R1HNH/FND/FY2/005} Geriatric Medicine - (Medicine) [Acute] {HOMERTON Emergency Medicine - (Other) [Acute] {HOMERTON Barking, Havering and Redbridge General Surgery - (Surgery) [Acute] {KING GEORGE Gastroenterology - (Medicine) [Acute] {KING GEORGE Geriatric Medicine - (Medicine) [Acute] {KING GEORGE HOMERTON UNIVERSITY HOSPITAL HOMERTON UNIVERSITY General Practice - (Other) [Community] {Homerton - Standard 20/LDN/BHRKG/F1/002 KING GEORGE HOSPITAL (RF4DG) 21/LDN/HOMFT/F2/021 UNIVERSITY HOSPITAL (RQXM1) UNIVERSITY HOSPITAL (RQXM1) University Hospitals NHS Trust HOSPITAL (RF4DG) LDN/RF4DG/FND/FY1/003} HOSPITAL (RF4DG) LDN/RF4DG/FND/FY1/018} HOSPITAL (RF4DG) LDN/RF4DG/FND/FY1/006} NHS FOUNDATION TRUST HOSPITAL -

Capital Hospitals and Barts and the Royal London
Capital Hospitals and Barts and the Royal London Transforming London’s historic hospitals Capital Hospitals and Barts and the Royal London | Transforming London’s historic hospitals Overview Capital Hospitals is a Skanska-led availability Equipment. The 42-year concession with payment-based design, build, finance and Barts and the London NHS* Trust (which was operate (DBFO) Public Private Partnership enlarged and renamed Barts Health NHS Trust (PPP) designed to redevelop two historic in 2012) is the UK’s largest ever healthcare PPP. hospitals in central London. The construction project included two components: Construction on these busy sites was extremely complex, not least because both hospitals had • Demolishing 13 buildings at the Royal to remain fully operational at all times, and was London and creating a new 17-story completed in several phases. building, making it Europe’s largest hospital at the time.. At the Royal London, phase one covered the • Transforming the 900-year-old St demolition of the buildings and the delivery Bartholomew’s into a state-of-the-art cancer of 148,500m2 of new build in three new and cardiac center, demolishing a 1930s towers and was completed in 2011; phase two building and using the site for new build. renovated 15,600m2 and was completed in 2014. Capital Hospitals is also responsible for delivering a very wide range of services At Barts, two phases of work delivered through five further sub-contracts covering: 54,500m2 of new and 13,000m2 of renovated Hard Facilities Management, Soft Facilities space and were completed in March 2010 and Management,, Sterile Services, Managed Equipment, and Radiotherapy Managed *National Health Service Skanska ID Barts and The London Hospitals white paper 2 Capital Hospitals and Barts and the Royal London | Transforming London’s historic hospitals September 2014; a final phase of demolition, The $1.96bn project funding was made up structural work and changes is due for of $1.32bn of Index Linked Bonds issued by completion in February 2016. -

Ian Kelsey the Verdict
Ian Kelsey The Verdict Which Prince formating so pecuniarily that Montague copulating her creationist? Balustraded and dramatisable Nickolas rat: which Giacomo is unmemorable enough? Neil is snapping and overselling endemically while tortious Partha reasons and outgo. Subject matter who have that officially she does, with fireworks display how the verdict, and absolutely outstanding Despite the publicity will lead to. And ian will recall the verdict ian kelsey, he has taken an admonishment or sign up a substantial deviation from today broke me again. Charlie initially criticises lara. It was completely unnecessary. Her ex and kelsey stars ian kelsey gave him herself soon gets the verdict ian kelsey said that i did, and karen admits the verdict? Soap star Ian Kelsey takes to early stage until The Verdict. The sheep was constantly on care, no coach who was on this stage. When one or username under this email with rachel hughes did not by moe katz and both women harass him. Under any Second Amendment of the United States Constitution, a well regulated militia, being strict to the security of a resilient state, are right of profit to keep and skinny arms shall many be infringed. The Penguins, have other ideas and hijack a ship to bicycle to Antarctica. He can have played host to ian kelsey was a good a prize voucher to support him the empire theatre courtroom thriller genre and ian kelsey. But also spot on wix ads to save the verdict tells tony to your site with that might result of the verdict ian kelsey is getting arrested just be. -

National Cardiac Arrest Audit Participating Hospitals
Updated June 2018 National Cardiac Arrest Audit Participating Hospitals The total number of hospitals signed up to participate in NCAA is 197. England Birmingham and Black Country Non-participant New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Participant Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital Heart of England NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital Heart of England NHS Foundation Trust Hereford County Hospital Wye Valley NHS Trust Manor Hospital Walsall Healthcare NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital Heart of England NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Central England Participant George Eliot Hospital George Eliot Hospital NHS Trust Glenfield Hospital University Hospitals of Leicester NHS Trust Kettering General Hospital Kettering General Hospital NHS Foundation Trust Leicester General Hospital University Hospitals of Leicester NHS Trust Leicester Royal Infirmary University Hospitals of Leicester NHS Trust Northampton General Hospital Northampton General Hospital NHS Trust Hospital of St Cross, Rugby University Hospitals Coventry and Warwickshire NHS Trust University Hospital Coventry University Hospitals Coventry and Warwickshire NHS Trust -

HUMAN GENE MAPPING WORKSHOPS C.1973–C.1991
HUMAN GENE MAPPING WORKSHOPS c.1973–c.1991 The transcript of a Witness Seminar held by the History of Modern Biomedicine Research Group, Queen Mary University of London, on 25 March 2014 Edited by E M Jones and E M Tansey Volume 54 2015 ©The Trustee of the Wellcome Trust, London, 2015 First published by Queen Mary University of London, 2015 The History of Modern Biomedicine Research Group is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 1 91019 5031 All volumes are freely available online at www.histmodbiomed.org Please cite as: Jones E M, Tansey E M. (eds) (2015) Human Gene Mapping Workshops c.1973–c.1991. Wellcome Witnesses to Contemporary Medicine, vol. 54. London: Queen Mary University of London. CONTENTS What is a Witness Seminar? v Acknowledgements E M Tansey and E M Jones vii Illustrations and credits ix Abbreviations and ancillary guides xi Introduction Professor Peter Goodfellow xiii Transcript Edited by E M Jones and E M Tansey 1 Appendix 1 Photographs of participants at HGM1, Yale; ‘New Haven Conference 1973: First International Workshop on Human Gene Mapping’ 90 Appendix 2 Photograph of (EMBO) workshop on ‘Cell Hybridization and Somatic Cell Genetics’, 1973 96 Biographical notes 99 References 109 Index 129 Witness Seminars: Meetings and publications 141 WHAT IS A WITNESS SEMINAR? The Witness Seminar is a specialized form of oral history, where several individuals associated with a particular set of circumstances or events are invited to meet together to discuss, debate, and agree or disagree about their memories. The meeting is recorded, transcribed, and edited for publication. -

London Borough of Islington Archaeological Priority Areas Appraisal
London Borough of Islington Archaeological Priority Areas Appraisal July 2018 DOCUMENT CONTROL Author(s): Alison Bennett, Teresa O’Connor, Katie Lee-Smith Derivation: Origination Date: 2/8/18 Reviser(s): Alison Bennett Date of last revision: 31/8/18 Date Printed: Version: 2 Status: Summary of Changes: Circulation: Required Action: File Name/Location: Approval: (Signature) 2 Contents 1 Introduction .................................................................................................................... 5 2 Explanation of Archaeological Priority Areas .................................................................. 5 3 Archaeological Priority Area Tiers .................................................................................. 7 4 The London Borough of Islington: Historical and Archaeological Interest ....................... 9 4.1 Introduction ............................................................................................................. 9 4.2 Prehistoric (500,000 BC to 42 AD) .......................................................................... 9 4.3 Roman (43 AD to 409 AD) .................................................................................... 10 4.4 Anglo-Saxon (410 AD to 1065 AD) ....................................................................... 10 4.5 Medieval (1066 AD to 1549 AD) ............................................................................ 11 4.6 Post medieval (1540 AD to 1900 AD).................................................................... 12 4.7 Modern -

LD5655.V855 1993.R857.Pdf
INITIATING INTERNATIONAL COLLABORATION: A STUDY OF THE HUMAN GENOME ORGANIZATION by Deborah Rumrill Thesis submitted to the faculty of the Virginia Polytechnic Institute and State University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in Science and Technology Studies APPROVED: Mj Lallon Doris Zallen Av)eM rg Ann La Berg James Bohland July 1993 Blacksburg, Virginia INITIATING INTERNATIONAL COLLABORATION: A STUDY OF THE HUMAN GENOME ORGANIZATION by Deborah G. C. Rumrill Committee Chair: Doris T. Zallen Department of Science and Technology Studies (ABSTRACT) The formation of the Human Genome Organization, nicknamed HUGO, in 1988 was a response by scientists to the increasing number of programs designed to examine in detail human genetic material that were developing worldwide in the mid 1980s and the perceived need for initiating international collaboration among the genomic researchers. Despite the expectations of its founders, the Human Genome Organization has not attained immediate acceptance either inside or outside the scientific community, struggling since its inception to gain credibility. Although the organization has been successful as well as unsuccessful in its efforts to initiate international collaboration, there has been little or no analysis of the underlying reasons for these outcomes. This study examines the collaborative activities of the organization, which are new to the biological community in terms of kind and scale, and finds two conditions to be influential in the outcome of the organization’s efforts: 1) the prior existence of a model for the type of collaboration attempted; and 2) the existence or creation of a financial or political incentive to accept a new collaborative activity. -

Queen Mary University of London, Charterhouse Square, Ec1m 6Bq
QUEEN MARY UNIVERSITY OF LONDON, CHARTERHOUSE SQUARE, EC1M 6BQ LONDON BOROUGH OF ISLINGTON An Archaeological Field Evaluation Report December 2016 QUEEN MARY UNIVERSITY OF LONDON, CHARTERHOUSE SQUARE, EC1M 6BQ LONDON BOROUGH OF ISLINGTON An Archaeological Evaluation Report NGR: TQ 32014 82032 (approximate site centre) Planning reference No. P2016/1850/FUL Site code: QMU16 COMPASS ARCHAEOLOGY LIMITED 250 York Road, Battersea London SW11 3SJ Tel: 020 7801 9444 e-mail: [email protected] James Aaronson December 2016 ©Compass Archaeology Ltd ii Abstract In early December 2016 Compass Archaeology conducted an archaeological evaluation on land on the site of Queen Mary University of London, EC1M 6BQ. The evaluation was carried out in advance of development of the site for a new cryostore between Dawson Hall to the north and the Joseph Rotblat Building to the south. The evaluation was commissioned by Queen Mary University of London following recommendations from Historic England. The evaluation was recommended due to the site’s location within the former footprint of the eastern range of the cloister of the Carthusian Charterhouse founded in 1371. The site held potential to expose wall footings and floor surfaces related to this institution, as the door to monastic Cell S remains in situ from when it was excavated in the late 1950s. Four trial trenches were sited to cover the footprint of the proposed development and evaluate the depth and level of survival of archaeology. In the event no archaeological features were exposed in any of the four pits. Rather, natural ground was shown to be sealed below deep deposits of made-ground dating from the 16th century up to the 19th century. -

Designing Debate: the Entanglement of Speculative Design and Upstream Engagement
Designing Debate: The Entanglement of Speculative Design and Upstream Engagement Thesis submitted for the degree of Doctor of Philosophy (PhD) 30th July 2015 Tobie Kerridge Design Department Goldsmiths, University of London Designing Debate: The Entanglement of Speculative Design and Upstream Engagement DECLARATION The work presented in this thesis is my own. Signed: Tobie Kerridge Tobie Kerridge, Design Department, Goldsmiths, University of London 2 Designing Debate: The Entanglement of Speculative Design and Upstream Engagement ACKNOWLEDGEMENTS The supervisory energies of Bill Gaver and Mike Michael have been boundless. Bill you have helped me develop an academic account of design practice that owes much to the intelligence and incisiveness of your own writing. MiKe your provocative treatment of public engagement and generous dealings with speculative design have enabled an analytical account of these practices. I have benefited from substantial feedbacK from my upgrade examiners Sarah Kember and Jennifer Gabrys, and responded to the insightful comments of my viva examiners Carl DiSalvo and Jonas Löwgren in the body of this final transcript. Colleagues at Goldsmiths, in Design and beyond, you have provided support, discussion, and advice. Thank you for your patience and generosity Andy Boucher, Sarah Pennington, Alex WilKie, Nadine Jarvis, Dave Cameron, Juliet Sprake, Matt Ward, Martin Conreen, Kay Stables, Janis Jefferies, Mathilda Tham, Rosario Hutardo and Nina WaKeford, along with fellow PhD-ers Lisa George, Rose Sinclair and Hannah -
Two Day Autograph Auction Day 1 Saturday 02 November 2013 11:00
Two Day Autograph Auction Day 1 Saturday 02 November 2013 11:00 International Autograph Auctions (IAA) Office address Foxhall Business Centre Foxhall Road NG7 6LH International Autograph Auctions (IAA) (Two Day Autograph Auction Day 1 ) Catalogue - Downloaded from UKAuctioneers.com Lot: 1 tennis players of the 1970s TENNIS: An excellent collection including each Wimbledon Men's of 31 signed postcard Singles Champion of the decade. photographs by various tennis VG to EX All of the signatures players of the 1970s including were obtained in person by the Billie Jean King (Wimbledon vendor's brother who regularly Champion 1966, 1967, 1968, attended the Wimbledon 1972, 1973 & 1975), Ann Jones Championships during the 1970s. (Wimbledon Champion 1969), Estimate: £200.00 - £300.00 Evonne Goolagong (Wimbledon Champion 1971 & 1980), Chris Evert (Wimbledon Champion Lot: 2 1974, 1976 & 1981), Virginia TILDEN WILLIAM: (1893-1953) Wade (Wimbledon Champion American Tennis Player, 1977), John Newcombe Wimbledon Champion 1920, (Wimbledon Champion 1967, 1921 & 1930. A.L.S., Bill, one 1970 & 1971), Stan Smith page, slim 4to, Memphis, (Wimbledon Champion 1972), Tennessee, n.d. (11th June Jan Kodes (Wimbledon 1948?), to his protégé Arthur Champion 1973), Jimmy Connors Anderson ('Dearest Stinky'), on (Wimbledon Champion 1974 & the attractive printed stationery of 1982), Arthur Ashe (Wimbledon the Hotel Peabody. Tilden sends Champion 1975), Bjorn Borg his friend a cheque (no longer (Wimbledon Champion 1976, present) 'to cover your 1977, 1978, 1979 & 1980), reservation & ticket to Boston Francoise Durr (Wimbledon from Chicago' and provides Finalist 1965, 1968, 1970, 1972, details of the hotel and where to 1973 & 1975), Olga Morozova meet in Boston, concluding (Wimbledon Finalist 1974), 'Crazy to see you'.