Cardiopulmonary Resuscitation: Update, Controversies and New Advances
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Commotio Cordis
Commotio Cordis Background Sudden unexpected cardiac death that occurs in young people during sports participation is usually associated with previously diagnosed or undiagnosed structural or primary electrical cardiac abnormalities. Examples of such abnormalities include hypertrophic cardiomyopathy, anomalous origin of a coronary artery, arrhythmogenic right ventricular cardiomyopathy, and primary electrical disorders, such as congenital prolongation of the QTc interval and catecholaminergic, polymorphic ventricular tachycardia (CPVT). Sudden death due to ventricular fibrillation may also occur following a blunt, nonpenetrating blow to the chest, specifically the precordial area, in an individual with no underlying cardiac disease. This is termed commotio cordis. Much of our understanding of the clinical and pathophysiologic aspects of commotio cordis is the result of work by N.A. Mark Estes III, MD, and Mark S. Link, MD, from the New England Cardiac Arrhythmia Center at the Tufts University and School of Medicine in Boston, Massachusetts and data derived from the US Commotio Cordis Registry (Minneapolis, Minnesota). Relatively recent data from the registry of the Minneapolis Heart Institute Foundation show that commotio cordis is one of the leading cause of sudden cardiac death in young athletes, exceeded only by hypertrophic cardiomyopathy and congenital cornoary artery abnormalities.[1] Commotio cordis typically involves young, predominantly male, athletes in whom a sudden, blunt, nonpenetrating and innocuous-appearing trauma to the anterior chest results in cardiac arrest and sudden death from ventricular fibrillation. The rate of successful resuscitation remains relatively low but is improving slowly. Although commotio cordis usually involves impact from a baseball, it has also been reported during hockey, softball, lacrosse, karate, and other sports activities in which a relatively hard and compact projectile or bodily contact caused impact to the person's precordium. -

Emergency Medical Services Program Policies – Procedures – Protocols
Emergency Medical Services Program Policies – Procedures – Protocols Protocols Table of Contents GENERAL PROVISIONS ................................................................................................ 3 DESTINATION DECISION SUMMARY-METRO BAKERSFIELD AREA ........................ 5 DETERMINATION OF DEATH ..................................................................................... 12 101 AIRWAY OBSTRUCTION ...................................................................................... 16 102 ALTERED LEVEL OF CONSCIOUSNESS ............................................................ 18 103 ALLERGIC REACTION/ANAPHYLAXIS ................................................................ 20 104 ASYSTOLE/ PULSELESS ELECTRICAL ACTIVITY ............................................. 22 105 BITES STINGS ENVENOMATION ......................................................................... 24 106 BRADYCARDIA ..................................................................................................... 26 107 BRIEF RESOLVED UNEXPLAINED EVENT ......................................................... 29 108 BURNS ................................................................................................................... 32 109 CHEMPACK ........................................................................................................... 35 110 CHEST PAIN OR ACUTE CORONARY SYNDROME ........................................... 37 111 CHEST TRAUMA .................................................................................................. -

Medical Memoranda MEDICAJHRNA Haemodynamic Effects of Balloon
27 January 1968 Medical Memoranda MEDICAJHRNA 225 he had been after the myocardial infarction in March 1967. There- He was readmitted on 6 September again in supraventricular after he was maintained on lignocaine infusion 1 mg./min. to a tachycardia and with evidence of congestive failure. On three maximum of 500 mg. in 24 hours and remained in sinus rhythm for occasions over the next 48 hours a precordial thump converted this Br Med J: first published as 10.1136/bmj.1.5586.225 on 27 January 1968. Downloaded from 48 hours with only occasional extrasystoles. By this time the rhythm to sinus rhythm. On each occasion the procedure was infusion had been discontinued and he felt well, was in sinus performed with the patient monitored on the cardioverter, and with rhythm 80/min., and the blood pressure was 120/70. the shock paddles prepared and an intravenous drip available for At this time he suddenly relapsed to the original dysrhythmia- giving sodium bicarbonate or other drugs in the event of more supraventricular tachycardia with right bundle-branch block. On serious arrhythmia developing. In view of the continuing cardiac this occasion, as an alternative to further electrical cardioversion irritability with multifocal extrasystoles he was then put on a but while being monitored on the " cardioverter," he was given a procainamide continuous infusion, 4 g. in 24 hours, which had the sharp blow on the sternum with no effect. A similar heavy thump effect of almost clearing the ventricular ectopic beats. with the ulnar side of the clenched fist on the precordium at the cardiac apex immediately induced sinus rhythm with left bundle- COMMENT branch block (see Fig.). -
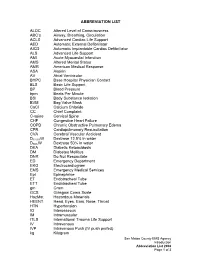
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Precordial Thump
practical procedures resuscitation skills – part five Precordial thump phil Jevon, pGce, Bsc, rN, is tachycardia, asystole and resuscitation officer/clinical skills complete heart block where a lead, Manor Hospital, Walsall. precordial thump was delivered. The results were as follows: The precordial thump is a blow to l Ninety-one (49%) reverted to the lower half of the patient’s normal sinus rhythm; sternum using the lateral aspect l Seventy-seven (41%) had no of a closed fist. It can successfully change in rhythm; resuscitate the patient when l Nineteen (10%) were worse; given promptly following a l Overall, 90% of patients were cardiac arrest caused by either better or no change and Fig 1. check carotic pulse ventricular fibrillation (VF) or 10% were worse. ventricular tachycardia (VT) (Resuscitation Council (UK), 2006). Procedure This article describes the On discovering a collapsed procedure for delivering a unconscious patient: precordial thump. l Call out for help and activate the emergency buzzer; Mechanism of action l Lie the patient flat; The rationale for delivering a l Look, listen and feel for no precordial thump is that it longer than 10 seconds to generates a mechanical energy, determine if the patient is which is converted to electrical breathing normally (an occasional energy, which then may be gasp, slow, laboured or noisy sufficient to achieve successful breathing is abnormal) or has other cardioversion (Kohl et al, 2005). signs of life (Resuscitation Council Following the onset of VF, the (UK), 2006). If trained and threshold for successful experienced in assessing ill defibrillation rises steeply after a patients, a simultaneous Fig 2. -

FIRST AID QUICK SHEET- Airway and Breathing
FIRST AID QUICK SHEET Airway and Breathing After you have checked to make sure the scene is safe and put on gloves to protect yourself (Danger) and checked if the patient is responsive (Response), if you find the patient is not responding, you should think: ABC. First check for an Airway and Breathing. Instructions for the A and B steps of the DR. ABC acronym for first aid priorities are below: How to Adjust Someone’s Airway (A): 1. Gently swipe the mouth with one finger to ensure that no objects are blocking the airway. 2. Place two fingers under the casualties chin and one hand on the forehead. 3. Gently lift the chin with two fingers, removing the tongue from the back of the throat. 4. If transport is delayed, roll the casualty onto their side in the recovery position to allow fluids to drain from the mouth Note: If someone is able to speak, their airway is open. Breathing (B): 1. Always remember to look, listen, and feel when checking for breathing. 2. LOOK to see the chest rise and fall. 3. LISTEN to hear breath sounds. 4. Place one hand on the stomach and FEEL for breathing movement and FEEL beneath the nose for air movement. After you have secured an airway and checked for breathing, you may move on to check for bleeding in the C (circulation) step of DR. ABC. *Please be safe and practice first aid at your own risk. LFR International is not liable for injuries resulting from any first aid attempts. . -
Basic Trauma Overview - ABC
Basic Trauma Overview - ABC Dale Dangleben, MD, FACS 1 2 Team 3 Extended Team 4 Team Leader Decrease chaos / optimize care. – Remains calm – Maintains control and provides direction – Stays decisive – Sees the big picture (situational awareness) – Is open to other team members input – Directs resuscitation – Makes early decision to transfer the patients that exceed the local capabilities 5 Team Members − Know your roles in the trauma team − Remain calm − Be responsive to team leader −Voice suggestions or concerns 6 Responsibilities – Perform the Primary and secondary survey – Verbalize patient care – Report completed tasks 7 Responsibilities – Monitors the patient – Manual BP – Obtains IV access – Administers medications – Dresses wounds – Performs or assists in resuscitative procedures 8 Responsibilities Records data Ensures documentation accompanies patient upon transfer Assists team members as needed 9 Responsibilities – Obtains needed supplies – Coordinates communication with local and external resources – Assists team members as needed 10 Responsibilities • Place Oxygen on patient • Manage airway • Hold C spine • Manage ventilator if • Manage rapid infuser line patient intubated where indicated • Assists team members as needed 11 Organization of trauma resuscitation area – Basic adult and pediatric equipment for: • Airway management (cart) • IV access with warm fluids • Chest tube insertion • Hemorrhage control (tourniquets, pelvic binders) • Immobilization • Medications • Pediatric length/weight based tape (Broselow Tape) – Warming -

Abdominal Pain 02/02/2021
Medical Control Board Approved Protocols ABDOMINAL PAIN 02/02/2021 Follow Assessment, General Procedures Protocol EMR • Assess and support ABCs • Position of comfort • Supine if: • Trauma • Hypotension • Syncope • NPO • Monitor vital signs • Oxygen indicated for: • Unstable vitals • Severity of pain • Suspected GI bleed EMT • 12-lead – See CARDIAC-ECG/12 Lead Procedure A-EMT • IV – NS with standard tubing • Titrate fluid to patient’s needs – See Shock Protocol EMT-I/ • Cardiac monitoring PARAMEDIC • Pain management – See Acute Pain Management Protocol 199 March, 2021 Medical Control Board Approved Protocols This page intentionally left blank 200 March, 2021 Medical Control Board Approved Protocols ACUTE ADRENAL INSUFFICIENCY PROTOCOL 02/02/2021 Follow Assessment, General Procedures Protocol • Acute adrenal insufficiency (crisis) can occur in the following settings: - During neonatal period (undiagnosed adrenal insufficiency) - In patients with known, pre-existing adrenal insufficiency (e.g., Addison’s disease) - In patients who are chronically steroid dependent (i.e., taking steroids daily, long- term, for any number of medical conditions) - Adrenal crisis can be triggered by any acute stressor (e.g., trauma or illness), as well as by abrupt cessation of steroid use (for any reason). • Signs/symptoms of adrenal crisis: Altered mental status, seizures; generalized weakness, hypotension, hypoglycemia, hyperkalemia. • Notify hospital you are transporting known/suspected adrenal crisis patient • Emergency transport for: ALOC, hypotension, hypoglycemia, suspected hyperkalemia. Acute adrenal crisis is an immediately life-threatening emergency, and must be treated aggressively EMR • PMH, Take thorough history of patient’s steroid use/dependence. Determine if the patient is on oral hydrocortisone. • Assess and support ABC’s • Oxygen therapy, as needed • Monitor vitals EMT • Check blood glucose • If blood glucose is <60: administer glucose solution orally if the patient is awake and able to protect own airway • Obtain 12 lead ECG; if time permitted. -

Triage and Scenario
Triage and Scenario By Bryan Lewis Triage Triage: Is a rapid approach to prioritizing a large number of patients Incident Casualty Collection Triage Site Point Officer/Treatment/Transport S imple T riage A nd R apid T reatment Triage ● Triage should be performed RAPIDLY ● Utilize START Triage to determine priority ● 30–60 seconds per patient ● Affix tag on left upper arm or leg – Triage 1. Scene Safety BSI and Identify number of patients, and types of injuries, communicate to EMS 2. Clear the “walking wounded” with verbal instruction: If you can hear me and you can move, walk to… (Use a PA System if Possible) 3. Direct patients to the casualty collection point (CCP) or treatment area for detailed assessment and medical care Green Minor Manager/Triage Officer will be the area to control patients and manage area 4. Green tag will be issued at the CCP These patients may be classified as MINOR START Triage Now use START to assess and categorize the remaining patients… USE Color System START-Triage Now categorize the patients by assessing each patient’s RPMs… ✓Respirations ✓Pulse ✓Mental Status START—RPM RESPIRATIONS Is the patient breathing? Yes Adult – respirations > 30 = Red/Immediate Pediatric – respirations < 15 or > 45 = Red/Immediate Adult – respirations < 30 = check pulse Pediatric – respirations > 15 and < 45 = check pulse START—RPM RESPIRATIONS Is the Patient Breathing? No Reposition the airway… Respirations begin = IMMEDIATE/RED If patient doesn’t breath . ▪ Adult – deceased = BLACK ▪ Pediatric: Pulse Present – give 5 rescue breaths -

Paramedic Update
PARAMEDIC UPDATE 2020 AGENDA Protocol format New medications Base contact requirements Against Medical Advice Pediatric King Airway Protocol changes New Policies Determination of death Online Certifications- Image trend NEW PROTOCOL FORMAT Public safety, EMT, and Public safety personal can Adults and Pediatric are on Paramedic protocols are in only perform skills in the top the same page. one document. canary yellow section Anything listed in the yellow EMT’s can perform any skills Paramedics will start with ALS section is a standing in the green BLS section the BLS section (BLS before order. Base contact must be located below the public ALS!) and move down into attempted for anything in the safety area. the ALS section as needed. red “base hospital contact required” section. NEW PROTOCOL FORMAT Adults Pediatrics (13 years and under) Public Safety First Aid Procedures: Only Public Safety First Aid Procedures: Only • Remove nearby objects to prevent injury to Patient. Place • Remove nearby objects to prevent injury to Patient. Place patient in recovery position on left side patient in recovery position on left side • Give Oxygen if available • Give Oxygen if available • Request Fire/EMS • Request Fire/EMS • Public safety will start here BLS Procedures: EMT’s and Paramedics start here BLS Procedures: EMT’s and Paramedics start here • Support ABC’s • Support ABC’s • Give Oxygen only if Spo2 < 94% or if in Respiratory Distress • Give Oxygen only if Spo2 <94% or if in Respiratory Distress • Blood Glucose Check, if hypoglycemic enter appropriate • Blood Glucose check, if hypoglycemic enter appropriate protocol protocol • EMT and Paramedic start here • If Focal seizure, place patient in position of comfort, rapid • If Focal seizure, place patient in position of comfort, rapid transport or ALS Rendezvous transport or ALS Rendezvous • If full body tonic/clonic seizure, prepare to support • If full body tonic/clonic seizure, prepare to support respirations, provide cooling measures if febrile respirations. -

First Aid & CPR Training Inc. “At a Glance”
First Aid & CPR Training Inc. REFERENCE MANUAL “At A Glance” 2 Introduction 3 Emergency Scene Management 13 Life Threatening Priorities 15 Levels of Consciousness and Shock 20 Heart Attacks, Strokes, and Heart-Smart Awareness 26 CPR 30 Automated External Defibrillation (AED) 32 Health Care Providers (HCP) 35 Choking 40 Wounds and Bleeding 46 Medical Conditions (Asthma, Allergies, Diabetes and Seizures) 54 Bone and Joint Injuries 58 Head and Spinal Injuries 62 Eye, Ear and Nose Injuries 65 Burns 68 Poisons 70 Opioid Overdoses 71 Cold and Heat Injuries 76 Rescue Carries 77 In Closing 78 Quiz ATTENTION Please pay extra attention when you see this symbol. Introduction Hello from all of us at Lifesaver 101 First Aid & CPR Training Inc. Thank you for selecting Lifesaver 101 to provide you with educational, enjoyable and effective First Aid and CPR training. This reference manual is to be used with the “hands- on” approach to our interactive training. Please enjoy your program. Learning objectives include clearly determining when to call 9-1-1 and what to do while waiting for help to arrive. Being confident in FIRST AID & CPR includes your ability to assess quickly and competently the components of an emergency situation. As a First Aider you will always follow the steps of Emergency Scene Management (ESM) by completing the Lifesaver 101 Rules of 123 & ABC and providing ongoing care. Any scene of a medical emergency can be overwhelming for a first aider. By taking a first aid course you are equipping yourself with the knowledge you will need to become and effective and confident first aider. -

Part 3: Defibrillation
Resuscitation (2005) 67, 203—211 Part 3: Defibrillation International Liaison Committee on Resuscitation The 2005 Consensus Conference considered ques- sic devices achieve higher first-shock success rates tions related to the sequence of shock delivery than monophasic defibrillators. This fact, combined and the use and effectiveness of various waveforms with the knowledge that interruptions to chest and energies. These questions have been grouped compressions are harmful, suggests that a one- into the following categories: (1) strategies before shock strategy (one shock followed immediately by defibrillation; (2) use of automated external defib- CPR) may be preferable to the traditional three- rillators (AEDs); (3) electrode-patient interface; (4) shock sequence for VF and pulseless ventricular use of the electrocardiographic (ECG) waveform to tachycardia (VT). alter management; (5) waveform and energy lev- els for the initial shock; (6) sequence after failure of the initial shock (i.e. second and subsequent Strategies before defibrillation shocks; and (7) other related topics. The International Guidelines 20001 state that Precordial thump defibrillation should be attempted as soon as ven- W59,W166B tricular fibrillation (VF) is detected, regardless of the response interval (i.e. time between collapse Consensus on science. No prospective studies and arrival of the AED). If the response interval have evaluated the use of the precordial (chest) is >4—5 min, however, there is evidence that thump. In three case series (LOE 5)2—4 VF or pulse- 1.5—3 min of CPR before attempted defibrillation less VT was converted to a perfusing rhythm by a may improve the victim’s chance of survival.