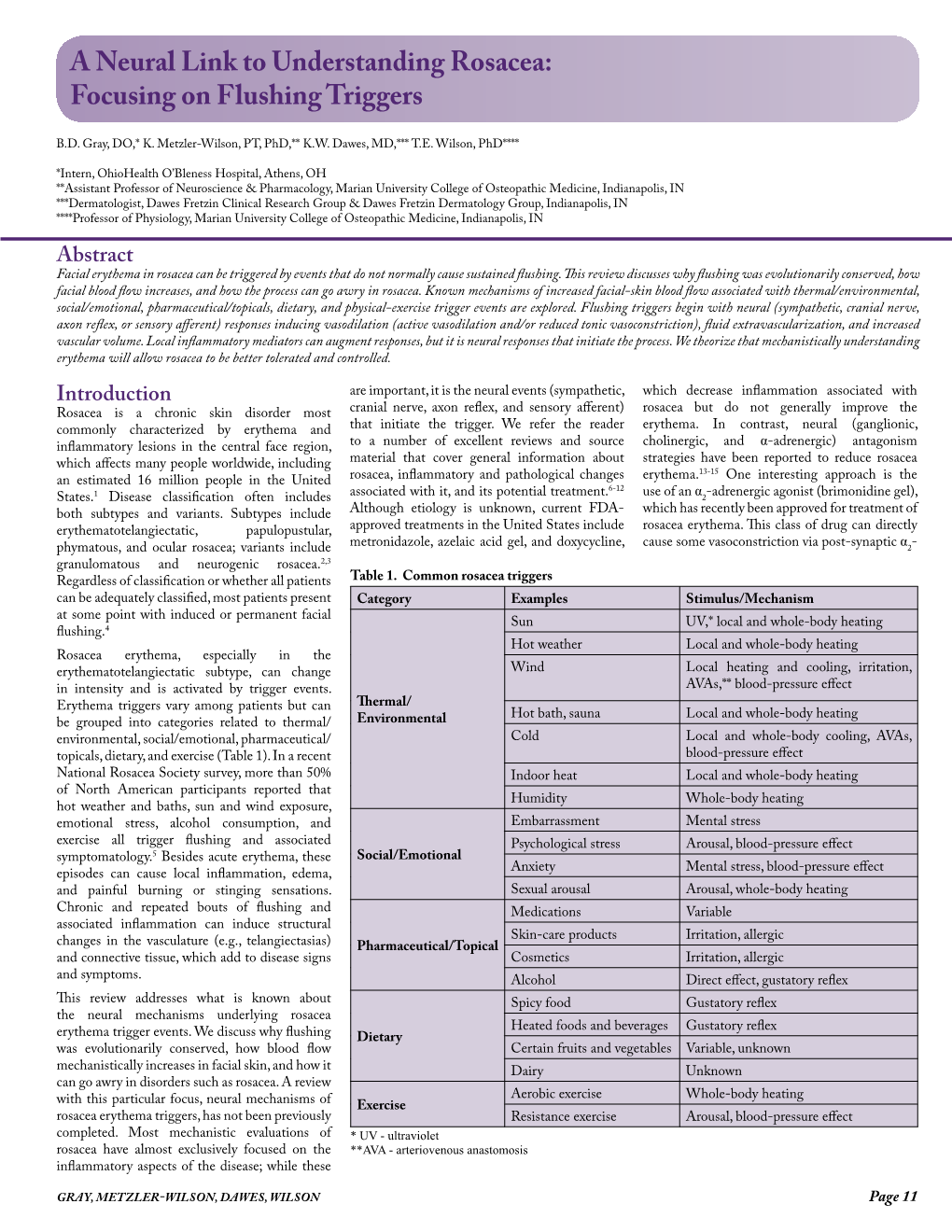
A Neural Link to Understanding Rosacea: Focusing on Flushing Triggers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiating Between Anxiety, Syncope & Anaphylaxis
Differentiating between anxiety, syncope & anaphylaxis Dr. Réka Gustafson Medical Health Officer Vancouver Coastal Health Introduction Anaphylaxis is a rare but much feared side-effect of vaccination. Most vaccine providers will never see a case of true anaphylaxis due to vaccination, but need to be prepared to diagnose and respond to this medical emergency. Since anaphylaxis is so rare, most of us rely on guidelines to assist us in assessment and response. Due to the highly variable presentation, and absence of clinical trials, guidelines are by necessity often vague and very conservative. Guidelines are no substitute for good clinical judgment. Anaphylaxis Guidelines • “Anaphylaxis is a potentially life-threatening IgE mediated allergic reaction” – How many people die or have died from anaphylaxis after immunization? Can we predict who is likely to die from anaphylaxis? • “Anaphylaxis is one of the rarer events reported in the post-marketing surveillance” – How rare? Will I or my colleagues ever see a case? • “Changes develop over several minutes” – What is “several”? 1, 2, 10, 20 minutes? • “Even when there are mild symptoms initially, there is a potential for progression to a severe and even irreversible outcome” – Do I park my clinical judgment at the door? What do I look for in my clinical assessment? • “Fatalities during anaphylaxis usually result from delayed administration of epinephrine and from severe cardiac and respiratory complications. “ – What is delayed? How much time do I have? What is anaphylaxis? •an acute, potentially -

Generalized Edema Resulting from Mixed Intestinal Infection by Entamoebia Histolytica and E
Case Report JOJ Case Stud Volume 12 Issue 2 -April 2021 Copyright © All rights are reserved by Ajite Adebukola DOI: 10.19080/JOJCS.2021.12.555833 Generalized Edema Resulting from Mixed Intestinal Infection by Entamoebia Histolytica and E. Coli in a Nigerian Female Adolescent: A Case Report Ajite Adebukola1,2*, Oluwayemi Oludare1,2 and Fatunla Odunayo2 1Department of Paediatrics, Ekiti State University, Nigeria 2Department of Paediatrics, Ekiti State University Teaching Hospital, Nigeria Submission: March 15, 2021; Published: April 08, 2021 *Corresponding author: Ajite Adebukola, Consultant Paediatrician, Department of Paediatrics, Ekiti State University, Ado Ekiti, Nigeria Abstract Amoebiasis, a clinical condition caused by Entamoeba histolytica does not usually present with generalized oedema known as anarsarca. We present a case of an adolescent female Nigerian who was admitted on account of chronic diarrhea and anarsarca in a tertiary hospital, Southwest Nigeria. There was no proteinuria. She however had cyst of E. histolytica and growth of E. coli in her stool; she also had E. coli isolated in her urine. She had hypoproteinaemia (35.2g/L) and hypoalbuminaemia (21.3g/L) as well as hypokalemia (2.97mmol/L). Symptoms resolved Entamoeba histolytica and Escherichia coli bacteria may be responsible for the worse clinical manifestations of Amoebiasis and biochemical parameters normalized following treatment with Nitrofurantoin, Tinidazole and Ciprofloxacin. A mixed infection of Keywords: Amoebiasis; Chronic diarrhea; Hypoproteinaemia; Anasarca Introduction Amoebiasis, caused by the protozoan Entamoeba histolytica of amenorrhoea. is an infection that frequently manifests clinically with symptoms recurrent generalized body swelling, and a seven-month history of abdominal pain, diarrhoea, dysentery and weight loss [1,2]. -

Ehrlichiosis and Anaplasmosis Are Tick-Borne Diseases Caused by Obligate Anaplasmosis: Intracellular Bacteria in the Genera Ehrlichia and Anaplasma
Ehrlichiosis and Importance Ehrlichiosis and anaplasmosis are tick-borne diseases caused by obligate Anaplasmosis: intracellular bacteria in the genera Ehrlichia and Anaplasma. These organisms are widespread in nature; the reservoir hosts include numerous wild animals, as well as Zoonotic Species some domesticated species. For many years, Ehrlichia and Anaplasma species have been known to cause illness in pets and livestock. The consequences of exposure vary Canine Monocytic Ehrlichiosis, from asymptomatic infections to severe, potentially fatal illness. Some organisms Canine Hemorrhagic Fever, have also been recognized as human pathogens since the 1980s and 1990s. Tropical Canine Pancytopenia, Etiology Tracker Dog Disease, Ehrlichiosis and anaplasmosis are caused by members of the genera Ehrlichia Canine Tick Typhus, and Anaplasma, respectively. Both genera contain small, pleomorphic, Gram negative, Nairobi Bleeding Disorder, obligate intracellular organisms, and belong to the family Anaplasmataceae, order Canine Granulocytic Ehrlichiosis, Rickettsiales. They are classified as α-proteobacteria. A number of Ehrlichia and Canine Granulocytic Anaplasmosis, Anaplasma species affect animals. A limited number of these organisms have also Equine Granulocytic Ehrlichiosis, been identified in people. Equine Granulocytic Anaplasmosis, Recent changes in taxonomy can make the nomenclature of the Anaplasmataceae Tick-borne Fever, and their diseases somewhat confusing. At one time, ehrlichiosis was a group of Pasture Fever, diseases caused by organisms that mostly replicated in membrane-bound cytoplasmic Human Monocytic Ehrlichiosis, vacuoles of leukocytes, and belonged to the genus Ehrlichia, tribe Ehrlichieae and Human Granulocytic Anaplasmosis, family Rickettsiaceae. The names of the diseases were often based on the host Human Granulocytic Ehrlichiosis, species, together with type of leukocyte most often infected. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -
How to Recognize a Suspected Cardiac Defect in the Neonate
Neonatal Nursing Education Brief: How to Recognize a Suspected Cardiac Defect in the Neonate https://www.seattlechildrens.org/healthcare- professionals/education/continuing-medical-nursing-education/neonatal- nursing-education-briefs/ Cardiac defects are commonly seen and are the leading cause of death in the neonate. Prompt suspicion and recognition of congenital heart defects can improve outcomes. An ECHO is not needed to make a diagnosis. Cardiac defects, congenital heart defects, NICU, cardiac assessment How to Recognize a Suspected Cardiac Defect in the Neonate Purpose and Goal: CNEP # 2092 • Understand the signs of congenital heart defects in the neonate. • Learn to recognize and detect heart defects in the neonate. None of the planners, faculty or content specialists has any conflict of interest or will be presenting any off-label product use. This presentation has no commercial support or sponsorship, nor is it co-sponsored. Requirements for successful completion: • Successfully complete the post-test • Complete the evaluation form Date • December 2018 – December 2020 Learning Objectives • Describe the risk factors for congenital heart defects. • Describe the clinical features of suspected heart defects. • Identify 2 approaches for recognizing congenital heart defects. Introduction • Congenital heart defects may be seen at birth • They are the most common congenital defect • They are the leading cause of neonatal death • Many neonates present with symptoms at birth • Some may present after discharge • Early recognition of CHD -

Cutaneous Manifestations of Abdominal Arteriovenous Fistulas
Cutaneous Manifestations of Abdominal Arteriovenous Fistulas Jessica Scruggs, MD; Daniel D. Bennett, MD Abdominal arteriovenous (A-V) fistulas may be edema.1-3 We report a case of abdominal aortocaval spontaneous or secondary to trauma. The clini- fistula presenting with lower extremity edema, ery- cal manifestations of abdominal A-V fistulas are thema, and cyanosis that had been previously diag- variable, but cutaneous findings are common and nosed as venous stasis dermatitis. may be suggestive of the diagnosis. Cutaneous physical examination findings consistent with Case Report abdominal A-V fistula include lower extremity A 51-year-old woman presented to the emergency edema with cyanosis, pulsatile varicose veins, department with worsening lower extremity swelling, and scrotal edema. redness, and pain. Her medical history included a We present a patient admitted to the hospital diagnosis of congestive heart failure, chronic obstruc- with lower extremity swelling, discoloration, and tive pulmonary disease, hepatitis C virus, tobacco pain, as well as renal insufficiency. During a prior abuse, and polysubstance dependence. Swelling, red- hospitalization she was diagnosed with venous ness, and pain of her legs developed several years stasis dermatitis; however, CUTISher physical examina- prior, and during a prior hospitalization she had been tion findings were not consistent with that diagno- diagnosed with chronic venous stasis dermatitis as sis. Imaging studies identified and characterized well as neurodermatitis. an abdominal aortocaval fistula. We propose that On admission, the patient had cool lower extremi- dermatologists add abdominal A-V fistula to the ties associated with discoloration and many crusted differential diagnosis of patients presenting with ulcerations. Aside from obesity, her abdominal exam- lower extremity edema with cyanosis, and we ination was unremarkable and no bruits were noted. -

Skin Manifestations of Illicit Drug Use Manifestações Cutâneas
RevABDV81N4.qxd 12.08.06 13:10 Page 307 307 Educação Médica Continuada Manifestações cutâneas decorrentes do uso de drogas ilícitas Skin manifestations of illicit drug use Bernardo Gontijo 1 Flávia Vasques Bittencourt 2 Lívia Flávia Sebe Lourenço 3 Resumo: O uso e abuso de drogas ilícitas é um problema significativo e de abrangência mun- dial. A Organização das Nações Unidas estima que 5% da população mundial entre os 15 e 64 anos fazem uso de drogas pelo menos uma vez por ano (prevalência anual), sendo que meta- de destes usam regularmente, isto é, pelo menos uma vez por mês. Muitos dos eventos adver- sos das drogas ilícitas surgem na pele, o que torna fundamental que o dermatologista esteja familiarizado com essas alterações. Palavras-chave: Drogas ilícitas; Drogas ilícitas/história; Drogas ilícitas/efeitos adversos; Pele; Revisão Abstract: Illicit drug use and abuse is a major problem all over the world. The United Nations estimates that 5% of world population (aged 15-64 years) use illicit drugs at least once a year (annual prevalence) and half of them use drugs regularly, that is, at least once a month. Many adverse events of illicit drugs arise on the skin and therefore dermatologists should be aware of these changes. Keywords: Street drugs; Street drugs/history; Street drugs/adverse effects; Skin; Review HISTÓRICO Há mais de cinco mil anos na Mesopotâmia, minorar o sofrimento dos condenados. região onde hoje se situa o Iraque, os poderes cal- Provavelmente seja o ópio a droga nephente à qual mantes, soníferos e anestésicos do ópio (do latim Homero se referia como “o mais poderoso destrui- opium, através do grego opion, ‘seiva, suco’) já eram dor de mágoas”.1,2 conhecidos pelos sumérios. -
Quick Tips on Recognizing Cutaneous Manifestations of Systemic Disease
FEATURE ARTICLE 2.0 Quick Tips on Recognizing Contact Hours Cutaneous Manifestations of Systemic Disease Jennifer Cittadino ABSTRACT: Although many skin manifestations are isolated This article will concentrate on nonmalignant cutaneous to a dermatological disorder, some skin manifestations can manifestations of systemic disease. The body systems will berelatedtoadeeper,moresystemicissue.Theskinis be reviewed, and their associated skin manifestations will be related to other body systems and functions. The impor- discussed. Some of the skin manifestations can be seen in tance of being able to recognize these dermatological multiple systemic disorders, such as erythema nodosum, manifestations and associate them with potential systemic which can be seen in pulmonary disorders, collagen and disease can be a critical diagnostic tool for the practitioner. vascular disorders, and gastrointestinal disorders. Pictures Sometimes, these skin manifestations can be the first sign will be provided when possible. of an internal disease. Although challenging, recognition, prompt diagnosis, and treatment can alter the course of a CARDIOVASCULAR AND PULMONARY SYSTEM life-threatening illness. There are several general cutaneous signs of cardiovascular Key words: Cutaneous, Dermatology, Systemic, Skin disease that may commonly be seen. These findings may include edema, cyanosis, clubbing of the nails, and corneal he skin is the largest organ in the body and one arcus. The corneal arcus appears as a gray-white ring around of the most visible body systems. The skin has the cornea and correlates with age and cholesterol levels. a reciprocal relationship between what is visu- A diagonal earlobe crease is also reported to be a marker for alized on the surface and what is occurring coronary artery disease (Uliasz & Lebwohl, 2008). -

(MPN) Symptoms
RECOGNIZING SYMPTOMS RECOGNIZING YOUR MPN SYMPTOMS The MPN LANDMARK SURVEY* is a large-scale analysis of patients with myeloproliferative neoplasms (MPNs) and Healthcare Professionals (HCPs) who treat these rare, chronic blood cancers (813 patients; 457 hematologists/oncologists). The results from LANDMARK provide new information that validates previous findings about the effect of MPN symptoms and their impact on the lives of patients, even those with low-risk MPNs. Fatigue is a symptom of particular note. Across diseases it was reported as the most common and severe symptom, and the one that patients most wanted to resolve. Symptoms such as fatigue can be vague and challenging to quantify. It is difficult to measure tiredness and its impact on daily life. In addition to physical symptoms, patients in the survey reported emotional difficulties—feeling irritable, angry or depressed. Many patients surveyed suffered with their MPN symptoms for a year or more before diagnosis. LANDMARK helps to confirm that MPN symptoms have a significant, negative impact on daily activities and quality of life, often resulting in limited or canceled family and/or social activities. For some, it means having to miss days from work, reduce hours, or even leave their job. These issues create stress, anxiety, and financial hardship for MPN patients. This information is intended to help patients validate the impact of MPN symptoms and know that they are not alone. SYMPTOM RECOGNITION Patients in the survey often did not recognize the connection between certain symptoms they were experiencing and their MPN. For example, patients with MPNs often have difficulty sleeping; however, some patients who reported this symptom did not realize it was related to their MPN. -

Pedal Edema in Older Adults Jennifer M
www.aging.arizona.edu July 2013 (updated May2015) ELDER CARE A Resource for Interprofessional Providers Pedal Edema in Older Adults Jennifer M. Vesely, MD, Teresa Quinn, MD, and Donald Pine, MD, Family Medicine Residency, University of Minnesota Pedal edema is the accumulation of fluid in the feet and pedal edema, which is more common in older adults, is lower legs. It is typically caused by one of two mechanisms. often multifactorial and may reflect a systemic process. The first is venous edema, caused by increased capillary Treating the underlying cause can often lessen the edema. filtration and retention of protein-poor fluid from the Table 1 lists common and less common causes of bilateral venous system into the interstitial space. The other pedal edema. mechanism is lymphatic edema, caused by obstruction or In addition to seeking evidence for the conditions listed in dysfunction of lymphatic outflow from the legs resulting in Table 1, certain clues in the patient’s presentation might accumulation of protein-rich interstitial fluid. These two point to a particular cause of edema. In particular, the mechanisms can operate independently or together. duration of edema and presence of pain should be noted. Regardless of the mechanism, chronic bilateral pedal Acute onset and presence of edema for less than 72 hours edema is detrimental to the health and quality of life of suggests the possibility of venous thrombosis and steps older adults. Besides alterations in cosmetic appearance or should be taken to exclude that diagnosis. Edema due to the discomfort it may cause, older adults with pedal edema chronic venous insufficiency is often associated with a dull often experience gait disturbance with decreased mobility aching pain. -

Review of Systems Health History Sheet Patient: ______DOB: ______Age: ______Gender: M / F
603 28 1/4 Road Grand Junction, CO 81506 (970) 263-2600 Review of Systems Health History Sheet Patient: _________________ DOB: ____________ Age: ______ Gender: M / F Please mark any symptoms you are experiencing that are related to your complaint today: Allergic/ Immunologic Ears/Nose/Mouth/Throat Genitourinary Men Only Frequent Sneezing Bleeding Gums Pain with Urinating Pain/Lump in Testicle Hives Difficulty Hearing Blood in Urine Penile Itching, Itching Dizziness Difficulty Urinating Burning or Discharge Runny Nose Dry Mouth Incomplete Emptying Problems Stopping or Sinus Pressure Ear Pain Urinary Frequency Starting Urine Stream Cardiovascular Frequent Infections Loss of Urinary Control Waking to Urinate at Chest Pressure/Pain Frequent Nosebleeds Hematologic / Lymphatic Night Chest Pain on Exertion Hoarseness Easy Bruising / Bleeding Sexual Problems / Irregular Heart Beats Mouth Breathing Swollen Glands Concerns Lightheaded Mouth Ulcers Integumentary (Skin) History of Sexually Swelling (Edema) Nose/Sinus Problems Changes in Moles Transmitted Diseases Shortness of Breath Ringing in Ears Dry Skin Women Only When Lying Down Endocrine Eczema Bleeding Between Shortness of Breath Increased Thirst / Growth / Lesions Periods When Walking Urination Itching Heavy Periods Constitutional Heat/Cold Intolerance Jaundice (Yellow Extreme Menstrual Pain Exercise Intolerance Gastrointestinal Skin or Eyes) Vaginal Itching, Fatigue Abdominal Pain Rash Burning or Discharge Fever Black / Tarry Stool Respiratory Waking to Urinate at Weight Gain (___lbs) Blood -

Drug Eruptions- When to Worry
3/17/2017 Drug reactions: Drug Eruptions‐ When to Worry 3 things you need to know 1. Type of drug reaction 2. Statistics: – Which drugs are most likely to cause that type of Lindy P. Fox, MD reaction? Associate Professor 3. Timing: Director, Hospital Consultation Service – How long after the drug started did the reaction Department of Dermatology University of California, San Francisco begin? [email protected] I have no conflicts of interest to disclose 1 Drug Eruptions: Common Causes of Cutaneous Drug Degrees of Severity Eruptions • Antibiotics Simple Complex • NSAIDs Morbilliform drug eruption Drug hypersensitivity reaction Stevens-Johnson syndrome •Sulfa (SJS) Toxic epidermal necrolysis (TEN) • Allopurinol Minimal systemic symptoms Systemic involvement • Anticonvulsants Potentially life threatening 1 3/17/2017 Morbilliform (Simple) Drug Eruption Morbilliform (Simple) Drug Eruption Per the drug chart, the most likely culprit is: Per the drug chart, the most likely culprit is: Day Day Day ‐> ‐8 ‐7 ‐6 ‐5 ‐4 ‐3 ‐2 ‐1 0 1 Day ‐> ‐8 ‐7 ‐6 ‐5 ‐4 ‐3 ‐2 ‐1 0 1 A vancomycin x x x x A vancomycin x x x x B metronidazole x x B metronidazole x x C ceftriaxone x x x C ceftriaxone x x x D norepinephrine x x x D norepinephrine x x x E omeprazole x x x x E omeprazole x x x x F SQ heparin x x x x F SQ heparin x x x x trimethoprim/ trimethoprim/ G xxxxxxx G xxxxxxx sulfamethoxazole sulfamethoxazole Admit day Rash onset Admit day Rash onset Morbilliform (Simple) Drug Eruption Drug Induced Hypersensitivity Syndrome • Begins 5‐10 days after drug started