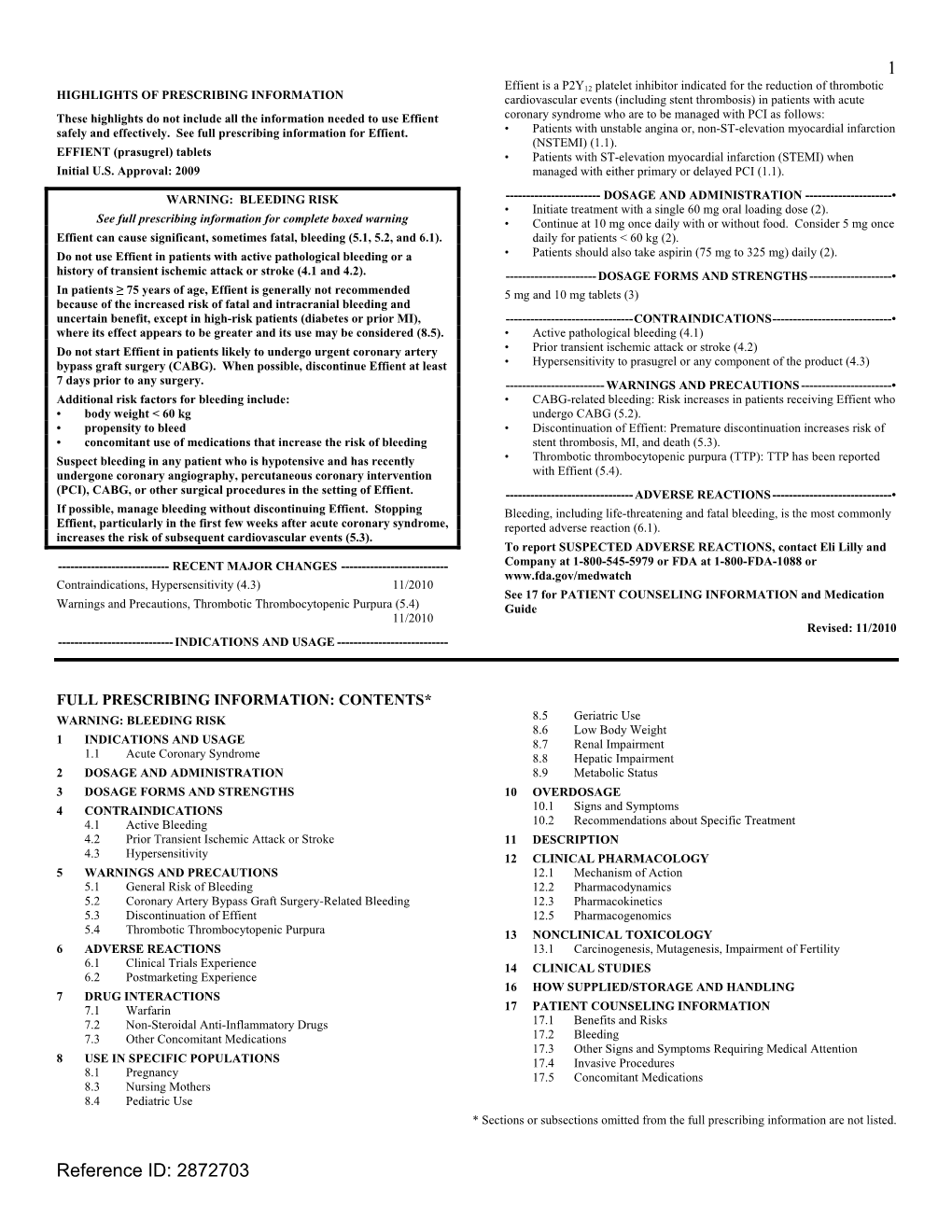
EFFIENT (Prasugrel) Tablets • Patients with ST-Elevation Myocardial Infarction (STEMI) When Initial U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Additions and Deletions to the Drug Product List
Prescription and Over-the-Counter Drug Product List 40TH EDITION Cumulative Supplement Number 09 : September 2020 ADDITIONS/DELETIONS FOR PRESCRIPTION DRUG PRODUCT LIST ACETAMINOPHEN; BUTALBITAL; CAFFEINE TABLET;ORAL BUTALBITAL, ACETAMINOPHEN AND CAFFEINE >A> AA STRIDES PHARMA 325MG;50MG;40MG A 203647 001 Sep 21, 2020 Sep NEWA ACETAMINOPHEN; CODEINE PHOSPHATE SOLUTION;ORAL ACETAMINOPHEN AND CODEINE PHOSPHATE >D> AA WOCKHARDT BIO AG 120MG/5ML;12MG/5ML A 087006 001 Jul 22, 1981 Sep DISC >A> @ 120MG/5ML;12MG/5ML A 087006 001 Jul 22, 1981 Sep DISC TABLET;ORAL ACETAMINOPHEN AND CODEINE PHOSPHATE >A> AA NOSTRUM LABS INC 300MG;15MG A 088627 001 Mar 06, 1985 Sep CAHN >A> AA 300MG;30MG A 088628 001 Mar 06, 1985 Sep CAHN >A> AA ! 300MG;60MG A 088629 001 Mar 06, 1985 Sep CAHN >D> AA TEVA 300MG;15MG A 088627 001 Mar 06, 1985 Sep CAHN >D> AA 300MG;30MG A 088628 001 Mar 06, 1985 Sep CAHN >D> AA ! 300MG;60MG A 088629 001 Mar 06, 1985 Sep CAHN ACETAMINOPHEN; HYDROCODONE BITARTRATE TABLET;ORAL HYDROCODONE BITARTRATE AND ACETAMINOPHEN >A> @ CEROVENE INC 325MG;5MG A 211690 001 Feb 07, 2020 Sep CAHN >A> @ 325MG;7.5MG A 211690 002 Feb 07, 2020 Sep CAHN >A> @ 325MG;10MG A 211690 003 Feb 07, 2020 Sep CAHN >D> AA VINTAGE PHARMS 300MG;5MG A 090415 001 Jan 24, 2011 Sep DISC >A> @ 300MG;5MG A 090415 001 Jan 24, 2011 Sep DISC >D> AA 300MG;7.5MG A 090415 002 Jan 24, 2011 Sep DISC >A> @ 300MG;7.5MG A 090415 002 Jan 24, 2011 Sep DISC >D> AA 300MG;10MG A 090415 003 Jan 24, 2011 Sep DISC >A> @ 300MG;10MG A 090415 003 Jan 24, 2011 Sep DISC >D> @ XIROMED 325MG;5MG A 211690 -

P2 Receptors in Cardiovascular Regulation and Disease
Purinergic Signalling (2008) 4:1–20 DOI 10.1007/s11302-007-9078-7 REVIEW P2 receptors in cardiovascular regulation and disease David Erlinge & Geoffrey Burnstock Received: 3 May 2007 /Accepted: 22 August 2007 /Published online: 21 September 2007 # Springer Science + Business Media B.V. 2007 Abstract The role of ATP as an extracellular signalling Introduction molecule is now well established and evidence is accumulating that ATP and other nucleotides (ADP, UTP and UDP) play Ever since the first proposition of cell surface receptors for important roles in cardiovascular physiology and pathophysi- nucleotides [1, 2], it has become increasingly clear that, in ology, acting via P2X (ion channel) and P2Y (G protein- addition to functioning as an intracellular energy source, the coupled) receptors. In this article we consider the dual role of purines and pyrimidines ATP, adenosine diphosphate ATP in regulation of vascular tone, released as a cotransmitter (ADP), uridine triphosphate (UTP) and uridine diphosphate from sympathetic nerves or released in the vascular lumen in (UDP) can serve as important extracellular signalling response to changes in blood flow and hypoxia. Further, molecules [3, 4] acting on 13 P2X homo- and heteromul- purinergic long-term trophic and inflammatory signalling is timer ionotropic and 8 P2Y metabotropic receptor subtypes described in cell proliferation, differentiation, migration and [5, 6] (Table 1). To terminate signalling, ectonucleotidases death in angiogenesis, vascular remodelling, restenosis and are present in the circulation and on cell surfaces, rapidly atherosclerosis. The effects on haemostasis and cardiac degrading extracellular ATP into ADP, AMP and adenosine regulation is reviewed. The involvement of ATP in vascular [7, 8]. -

Prasugrel Mylan 10 Mg Film-Coated Tablets Prasugrel
Package leaflet: Information for the user Prasugrel Mylan 5 mg film-coated tablets Prasugrel Mylan 10 mg film-coated tablets prasugrel Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. – Keep this leaflet. You may need to read it again. – If you have any further questions, ask your doctor or pharmacist. – This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. – If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Prasugrel Mylan is and what it is used for 2. What you need to know before you take Prasugrel Mylan 3. How to take Prasugrel Mylan 4. Possible side effects 5. How to store Prasugrel Mylan 6. Contents of the pack and other information 1. What Prasugrel Mylan is and what it is used for Prasugrel Mylan, which contains the active substance prasugrel, belongs to a group of medicines called antiplatelet agents. Platelets are very small cell particles that circulate in the blood. When a blood vessel is damaged, for example if it is cut, platelets clump together to help form a blood clot (thrombus). Therefore, platelets are essential to help stop bleeding. If clots form within a hardened blood vessel such as an artery they can be very dangerous as they can cut off the blood supply, causing a heart attack (myocardial infarction), stroke or death. -

Salts of Therapeutic Agents: Chemical, Physicochemical, and Biological Considerations
molecules Review Salts of Therapeutic Agents: Chemical, Physicochemical, and Biological Considerations Deepak Gupta 1, Deepak Bhatia 2 ID , Vivek Dave 3 ID , Vijaykumar Sutariya 4 and Sheeba Varghese Gupta 4,* 1 Department of Pharmaceutical Sciences, School of Pharmacy, Lake Erie College of Osteopathic Medicine, Bradenton, FL 34211, USA; [email protected] 2 ICPH Fairfax Bernard J. Dunn School of Pharmacy, Shenandoah University, Fairfax, VA 22031, USA; [email protected] 3 Wegmans School of Pharmacy, St. John Fisher College, Rochester, NY 14618, USA; [email protected] 4 Department of Pharmaceutical Sciences, USF College of Pharmacy, Tampa, FL 33612, USA; [email protected] * Correspondence: [email protected]; Tel.: +01-813-974-2635 Academic Editor: Peter Wipf Received: 7 June 2018; Accepted: 13 July 2018; Published: 14 July 2018 Abstract: The physicochemical and biological properties of active pharmaceutical ingredients (APIs) are greatly affected by their salt forms. The choice of a particular salt formulation is based on numerous factors such as API chemistry, intended dosage form, pharmacokinetics, and pharmacodynamics. The appropriate salt can improve the overall therapeutic and pharmaceutical effects of an API. However, the incorrect salt form can have the opposite effect, and can be quite detrimental for overall drug development. This review summarizes several criteria for choosing the appropriate salt forms, along with the effects of salt forms on the pharmaceutical properties of APIs. In addition to a comprehensive review of the selection criteria, this review also gives a brief historic perspective of the salt selection processes. Keywords: chemistry; salt; water solubility; routes of administration; physicochemical; stability; degradation 1. -

A Comparative Study of Molecular Structure, Pka, Lipophilicity, Solubility, Absorption and Polar Surface Area of Some Antiplatelet Drugs
International Journal of Molecular Sciences Article A Comparative Study of Molecular Structure, pKa, Lipophilicity, Solubility, Absorption and Polar Surface Area of Some Antiplatelet Drugs Milan Remko 1,*, Anna Remková 2 and Ria Broer 3 1 Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Comenius University in Bratislava, Odbojarov 10, SK-832 32 Bratislava, Slovakia 2 Department of Internal Medicine, Faculty of Medicine, Slovak Medical University, Limbová 12, SK–833 03 Bratislava, Slovakia; [email protected] 3 Department of Theoretical Chemistry, Zernike Institute for Advanced Materials, University of Groningen, Nijenborgh 4, 9747 AG Groningen, The Netherlands; [email protected] * Correspondence: [email protected]; Tel.: +421-2-5011-7291 Academic Editor: Michael Henein Received: 18 February 2016; Accepted: 11 March 2016; Published: 19 March 2016 Abstract: Theoretical chemistry methods have been used to study the molecular properties of antiplatelet agents (ticlopidine, clopidogrel, prasugrel, elinogrel, ticagrelor and cangrelor) and several thiol-containing active metabolites. The geometries and energies of most stable conformers of these drugs have been computed at the Becke3LYP/6-311++G(d,p) level of density functional theory. Computed dissociation constants show that the active metabolites of prodrugs (ticlopidine, clopidogrel and prasugrel) and drugs elinogrel and cangrelor are completely ionized at pH 7.4. Both ticagrelor and its active metabolite are present at pH = 7.4 in neutral undissociated form. The thienopyridine prodrugs ticlopidine, clopidogrel and prasugrel are lipophilic and insoluble in water. Their lipophilicity is very high (about 2.5–3.5 logP values). The polar surface area, with regard to the structurally-heterogeneous character of these antiplatelet drugs, is from very large interval of values of 3–255 Å2. -
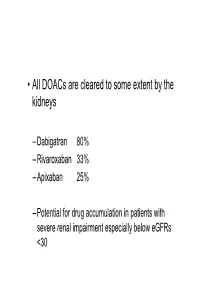
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Anticoagulation Reversal Guideline for Adults
Anticoagulation Reversal Guideline for Adults Antithrombotic reversal strategies should be limited to clinical situations (i.e. life-threatening bleeding) where the immediate need for anticoagulant reversal outweighs the risk of thrombosis (either from the reversal agent itself or normalization of coagulation in a patient with underlying thromboembolic risk). These recommendations are meant to serve as general guidelines and should not replace clinical judgment. Always seek input from the appropriate specialists when indicated and include the patient and/or family in shared decision making when possible. This document is not meant to guide selection of patients for reversal therapies. Please refer to appropriate national guidelines to aide decision- making regarding need for reversal, if warranted. 1. ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants 2. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine All indications for anticoagulation are considered, including atrial fibrillation, venous thromboembolism, prosthetic cardiac valves, and intracardiac thrombus. Mechanical circulatory support devices, including temporary or permanent ventricular assist devices (i.e. LVADs), are excluded from this document. Whenever possible, anticoagulation should be resumed in a timely manner to avoid thromboembolic complications related to the underlying indication for anticoagulation. This guideline does not provide recommendations on resuming anticoagulation. References: • Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Experts Consensus Decisions Pathways. J Am Coll Cardiol. -

Dissertation.Pdf
UNIVERSITÄTSKLINIKUM HAMBURG-EPPENDORF Zentrum für Experimentelle Medizin, Institut für Experimentelle Pharmakologie und Toxikologie Direktor: Professor T. Eschenhagen Thrombus-Targeted Theranostic Microbubbles for Simultaneous Ultrasound Diagnosis and Therapy of Thrombosis. Title page Dissertation zur Erlangung des Grades eines Doktors der Medizin an der Medizinischen Fakultät der Universität Hamburg. vorgelegt von: Yannik Andreas Gkanatsas aus Bremen Hamburg 2017 Angenommen von der Medizinischen Fakultät der Universität Hamburg am: 13.12.2017 Veröffentlicht mit Genehmigung der Medizinischen Fakultät der Universität Hamburg. Prüfungsausschuss, der Vorsitzende: Prof. Dr. Thomas Eschenhagen Prüfungsausschuss, zweite Gutachterin: Prof. Dr. Renate Bonin-Schnabel Prüfungsausschuss, dritter Gutachter: PD Dr. Florian Langer 2 Table of contents Title page ..................................................................................................................... 1 Table of contents ......................................................................................................... 3 List of Figures: ............................................................................................................. 6 List of Tables: .............................................................................................................. 7 Chapter 1. Introduction ............................................................................................. 8 1.1 Cardiovascular Disease (CVD) ......................................................................................... -

Salts of Therapeutic Agents: Chemical, Physicochemical and Biological
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 16 April 2018 doi:10.20944/preprints201804.0187.v1 1 Review 2 Salts of Therapeutic Agents: Chemical, 3 Physicochemical and Biological Considerations 4 Deepak Gupta 1, Deepak Bhatia 2, Vivek Dave3, Vijaykumar Sutariya 4 and Sheeba Varghese 5 Gupta4* 6 1 Lake Eerie College of Osteopathic Medicine , School of Pharmacy, Pharmaceutical Sciences , Bradenton , FL , USA; 7 email: [email protected] 8 2 Shenandoah University - ICPH Fairfax Bernard J. Dunn School of Pharmacy, Fairfax, VA 22031USA; email: 9 [email protected] 10 3 Wegmans School of Pharmacy, St. John Fisher College, Rochester, NY, USA; email: [email protected] 11 4 Department of Pharmaceutical Sciences, USF College of Pharmacy, Tampa, FL, USA; email: 12 [email protected] 13 * Correspondence: [email protected]; Tel.: +01-813-974-2635 14 15 Abstract: Choice of the salts of therapeutic agents or active pharmaceutical ingredients (API) is 16 based on the physicochemical properties of API and the dosage form considerations. The 17 appropriate salt can have positive effect on overall therapeutic and pharmaceutical effects of API. 18 However, the incorrect salt form can negatively affect the overall pharmaceutical outcomes of the 19 API. This review addresses various criteria for choosing appropriate salt form along with the effect 20 of salt forms on API’s pharmaceutical properties. In addition to comprehensive review of the 21 criteria, this review also gives a brief historic perspective of the salt selection process. 22 23 Keywords: Chemistry, salt, water solubility, routes of administration, physicochemical, stability, 24 degradation 25 1. Introduction 26 Salt of an Active Pharmaceutical Ingredient (API) often formed to achieve desirable formulation 27 properties. -

New Drugs: T-Score for Transparency
New drugs: T-score for transparency Access to information about drugs is essential for the quality For 2011, the T-score has been revised to include the AusPAR. use of medicines. Pharmaceutical companies and regulatory agencies, such as the Therapeutic Goods Administration The revised T-scores will be as follows: (TGA), hold large quantities of information about individual drugs, but do not always share this information. To encourage T T T manufacturer provided complete clinical evaluation transparency, Australian Prescriber rates companies' willingness to provide clinical information about new drugs. T T manufacturer provided additional useful Table 1 shows how the companies have performed between information January 2009 and December 2010. The TGA is now publishing Australian Public Assessment T manufacturer provided the AusPAR and/or the Reports (AusPARs) for prescription medicines. While the product information Editorial Executive Committee welcomes this move to greater transparency, it will still ask companies to provide the clinical T manufacturer declined to supply data evaluations for their new products. While there are similarities, the AusPAR may not include all the details found in the X manufacturer did not respond to request for data regulator's clinical evaluation. Table 1 Pharmaceutical company responses to requests for clinical evaluation data for drugs marketed Jan 2009 – Dec 2010 Company Drug T T T manufacturer provided clinical evaluation Amgen denosumab Ferring degarelix Pfizer anidulafungin eletriptan PharmaLink cilostazol Phebra caffeine citrate Roche methoxy polyethylene glycol-epoetin beta tocilizumab Sanofi Pasteur H5N1 influenza vaccine Shire icatibant Wyeth methylnaltrexone T T manufacturer provided additional useful information Abbott omega-3-acid ethyl esters Celgene azacitidine Commercial Eyes melatonin CSL H1N1 influenza vaccine Japanese encephalitis vaccine Eli Lilly prasugrel Table continued.. -

Cardioprotection by Very Mild Hypothermia in Mice
67 Brief Report Cardioprotection by very mild hypothermia in mice Betül Knoop1,2#, David Naguib1,2#, Lisa Dannenberg1,2, Carolin Helten1,2, Saif Zako1,2, Christian Jung1,2, Bodo Levkau3, Maria Grandoch4, Malte Kelm1,2, Tobias Zeus1,2, Amin Polzin1,2 1Department of Cardiology, Pulmonology, and Vascular Medicine, Medical Faculty of the Heinrich Heine University Düsseldorf, Düsseldorf, Germany; 2Cardiovascular Research Institute Düsseldorf (CARID), Düsseldorf, Germany; 3Institute of Pathophysiology, West German Heart and Vascular Center, University Hospital Essen, University of Duisburg-Essen, Essen, Germany; 4Institute for Pharmacology and Clinical Pharmacology, Heinrich Heine University Düsseldorf, Düsseldorf, Germany #These authors contributed equally to this work. Correspondence to: Dr. med. Amin Polzin, PD. Klinik für Kardiologie, Pneumologie und Angiologie, Moorenstrasse 5, 40225 Düsseldorf, Germany. Email: [email protected]. Abstract: Target temperature management is recommended in post-resuscitation care. Additionally, hypothermia is a promising option in adjunctive therapy of acute myocardial infarction (MI). However, first in men data are contradicting. There are still many open questions to identify the optimal regimen and target temperature. In this study, we aimed to investigate the effect of very mild hypothermia on infarct size (IS) in mice. Mice underwent cardiac ischemia by temporary occlusion of the left anterior descending (LAD) artery under conditions of very mild hypothermia (34–36 ). Hypothermia was reached within the first 5 minutes of ischemia (temperature: 34.6±0.5 vs. 36.8±1.1 , P=0.035). Very mild hypothermia reduced IS ℃ in mice undergoing 30 minutes ischemia [IS/area at risk (AAR): 45±12% vs. 22±4%, P=0.018] as well as mice ℃ undergoing 60 minutes ischemia [IS/AAR: 67±7% vs.