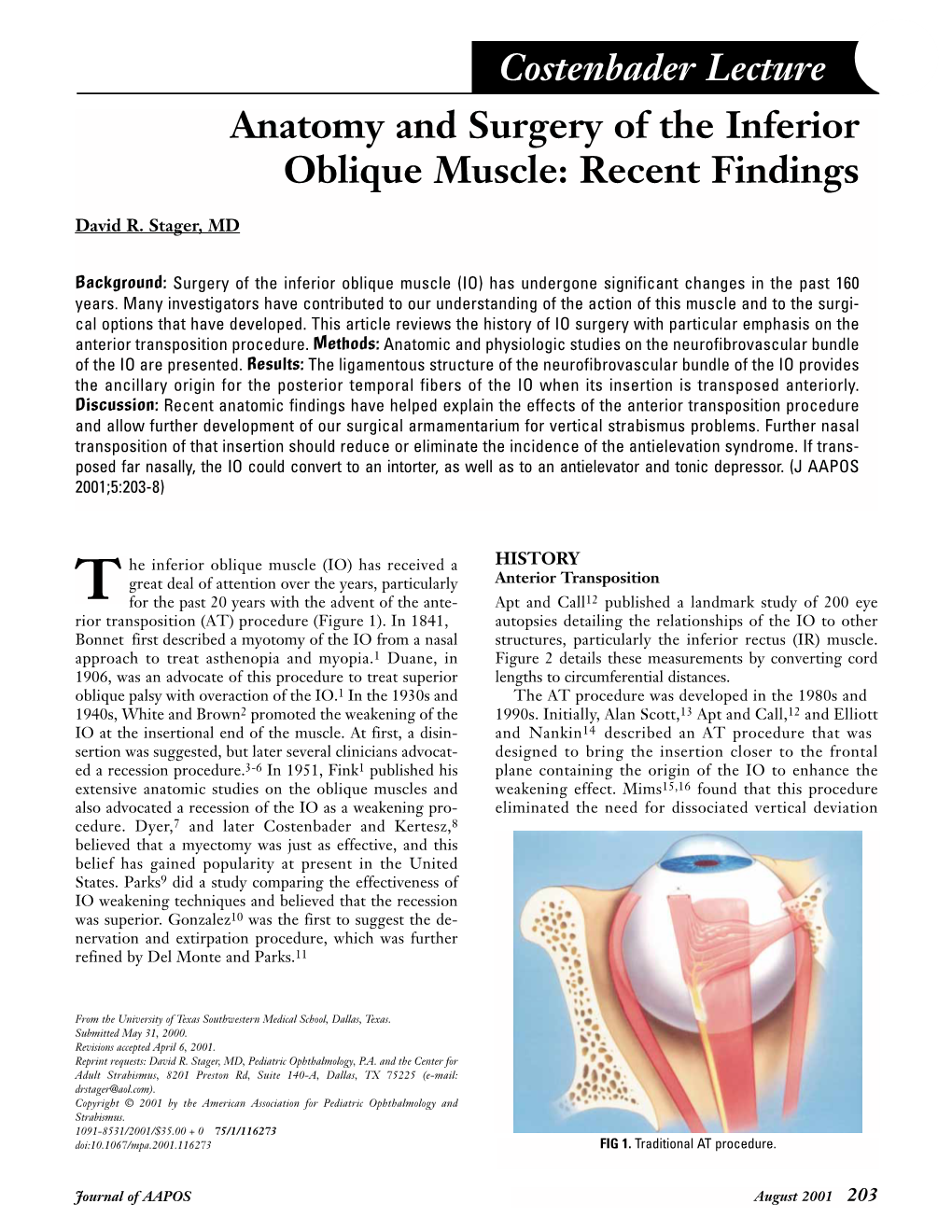
Costenbader Lecture Anatomy and Surgery of the Inferior Oblique Muscle: Recent Findings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Questions on Human Anatomy
Standard Medical Text-books. ROBERTS’ PRACTICE OF MEDICINE. The Theory and Practice of Medicine. By Frederick T. Roberts, m.d. Third edi- tion. Octavo. Price, cloth, $6.00; leather, $7.00 Recommended at University of Pennsylvania. Long Island College Hospital, Yale and Harvard Colleges, Bishop’s College, Montreal; Uni- versity of Michigan, and over twenty other medical schools. MEIGS & PEPPER ON CHILDREN. A Practical Treatise on Diseases of Children. By J. Forsyth Meigs, m.d., and William Pepper, m.d. 7th edition. 8vo. Price, cloth, $6.00; leather, $7.00 Recommended at thirty-five of the principal medical colleges in the United States, including Bellevue Hospital, New York, University of Pennsylvania, and Long Island College Hospital. BIDDLE’S MATERIA MEDICA. Materia Medica, for the Use of Students and Physicians. By the late Prof. John B Biddle, m.d., Professor of Materia Medica in Jefferson Medical College, Phila- delphia. The Eighth edition. Octavo. Price, cloth, $4.00 Recommended in colleges in all parts of the UnitedStates. BYFORD ON WOMEN. The Diseases and Accidents Incident to Women. By Wm. H. Byford, m.d., Professor of Obstetrics and Diseases of Women and Children in the Chicago Medical College. Third edition, revised. 164 illus. Price, cloth, $5.00; leather, $6.00 “ Being particularly of use where questions of etiology and general treatment are concerned.”—American Journal of Obstetrics. CAZEAUX’S GREAT WORK ON OBSTETRICS. A practical Text-book on Midwifery. The most complete book now before the profession. Sixth edition, illus. Price, cloth, $6.00 ; leather, $7.00 Recommended at nearly fifty medical schools in the United States. -

Relation of Macular and Other Holes to the Insertion of the Inferior Oblique
Br J Ophthalmol: first published as 10.1136/bjo.47.2.90 on 1 February 1963. Downloaded from Brit. J. Ophthal. (1963) 47, 90. RELATION OF MACULAR AND OTHER HOLES TO THE INSERTION OF THE INFERIOR OBLIQUE* WITH A NOTE ON THE TOPOGRAPHY OF THE POSTERIOR SURFACE OF THE GLOBE BY ANWAR EL MASSRI Faculty ofMedicine, Ein-Shams University, Cairo THE macular region, like the peripheral retina, is liable to cystic degeneration, especially in high myopes and in old people. This gives a honeycomb appearance and on rupture of the cyst or cysts by slight or severe trauma a depression is produced which may be confined to the inner layers of the retina or form a macular hole. A hole may occur in a normal macula immediately after trauma or after an interval during which probably cystic degeneration has developed. A macular hole may also be formed in the process of retrac- tion of the vitreous if the macula is previously diseased or affected. These holes are always round or oval with a punched appearance. Multiple holes are rare. They may or may not be accompanied by retinal detachment. copyright. It seems that relationship exists between the formation of a macular hole and the contraction of the inferior oblique muscle (el Massri, 1958). In about five out of nine cases, the hole is accompanied by a peripheral tear or an area of degeneration at about 7 to 8 o'clock in the right eye or 4 to 5 o'clock in the left. At operation the peripheral tears were seen to be situated of the insertion of over the lateral end the inferior oblique. -

Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2
Open Access Review Article DOI: 10.7759/cureus.5679 Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2 Bruno Bordoni 1 , Marta Simonelli 2 , Maria Marcella Lagana 3 1. Cardiology, Foundation Don Carlo Gnocchi, Milan, ITA 2. Osteopathy, French-Italian School of Osteopathy, Pisa, ITA 3. Radiology, IRCCS Fondazione Don Carlo Gnocchi Onlus, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract The tentorium cerebelli is a meningeal portion in relation to the skull, the nervous system, and the cervical tract. In this second part, the article discusses the systematic tentorial relationships, such as the central and cervical neurological connections, the venous circulation and highlights possible clinical alterations that could cause pain. To understand the function of anatomy, we should always remember that every area of the human body is never a segment, but a functional continuum. Categories: Physical Medicine & Rehabilitation, Anatomy, Osteopathic Medicine Keywords: tentorium cerebelli, fascia, pain, venous circulation, neurological connections, cranio Introduction And Background Cervical neurological connections The ansa cervicalis characterizes the first cervical roots and connects all anterior cervical nerve exits with the inferior floor of the oral cavity, the trigeminal system, the respiratory control system, and the sympathetic system. The descending branch of the hypoglossal nerve anastomoses with C1, forming the ansa hypoglossi or ansa cervicalis superior [1]. The inferior root of the ansa cervicalis, also known as descendens cervicalis, is formed by ascendant fibers from spinal nerves C2-C3 and occasionally fibers C4, lying anteriorly to the common carotid artery (it passes laterally or medially to the internal jugular vein upon anatomical variations) [1]. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

Anatomy of the Periorbital Region Review Article Anatomia Da Região Periorbital
RevSurgicalV5N3Inglês_RevistaSurgical&CosmeticDermatol 21/01/14 17:54 Página 245 245 Anatomy of the periorbital region Review article Anatomia da região periorbital Authors: Eliandre Costa Palermo1 ABSTRACT A careful study of the anatomy of the orbit is very important for dermatologists, even for those who do not perform major surgical procedures. This is due to the high complexity of the structures involved in the dermatological procedures performed in this region. A 1 Dermatologist Physician, Lato sensu post- detailed knowledge of facial anatomy is what differentiates a qualified professional— graduate diploma in Dermatologic Surgery from the Faculdade de Medician whether in performing minimally invasive procedures (such as botulinum toxin and der- do ABC - Santo André (SP), Brazil mal fillings) or in conducting excisions of skin lesions—thereby avoiding complications and ensuring the best results, both aesthetically and correctively. The present review article focuses on the anatomy of the orbit and palpebral region and on the important structures related to the execution of dermatological procedures. Keywords: eyelids; anatomy; skin. RESU MO Um estudo cuidadoso da anatomia da órbita é muito importante para os dermatologistas, mesmo para os que não realizam grandes procedimentos cirúrgicos, devido à elevada complexidade de estruturas envolvidas nos procedimentos dermatológicos realizados nesta região. O conhecimento detalhado da anatomia facial é o que diferencia o profissional qualificado, seja na realização de procedimentos mini- mamente invasivos, como toxina botulínica e preenchimentos, seja nas exéreses de lesões dermatoló- Correspondence: Dr. Eliandre Costa Palermo gicas, evitando complicações e assegurando os melhores resultados, tanto estéticos quanto corretivos. Av. São Gualter, 615 Trataremos neste artigo da revisão da anatomia da região órbito-palpebral e das estruturas importan- Cep: 05455 000 Alto de Pinheiros—São tes correlacionadas à realização dos procedimentos dermatológicos. -

Illustrations from the Wellcome Institute Library
Medical History, 1984, 28: 432437 ILLUSTRATIONS FROM THE WELLCOME INSTITUTE LIBRARY THE ORIGIN OF THE WELLCOME ANATOMICAL WAXES ALBINUS AND THE FLORENTINE COLLECTION AT LA SPECOLA* RECENT research has indicated a possible link between the wax models in the Wellcome Museum in London and the exquisite life-sized figures at La Specola in Florence.' This study offers further evidence that the Wellcome figures are, indeed, initial sketch models for not one, but two, sets of models at La Specola: the life-sized series already mentioned, and a smaller set about 75 cms. high; and that the source for all three sets of models is the German anatomist, Bernard Siegfried Albinus (1697-1770), and his artist/engraver, Jan Wandelaer (1690-1759). The seven standing male figures of the Wellcome Collection, hereinafter identified as the "'W" models, measuring only 85 cms. high, depict the human body in various stages of dissection. This study concentrates only on the four "W" models which show bones, muscles, and tendons, and on the similar Florentine models (Table I). The other three "W" models, showing arteries and veins, are omitted from this study as the normal variability of these structures does not lend itself to a valid comparative study. TABLE I Albinus Wellcome La Specola Models Group Tablesa Models Largeb Small A I 4557 444/000 956 B II, VI 4551 442/557 000c C III, VII 4555 443/558 959 D IV 4556 441/000 957 -aAlbinus Tables I-IV show the frontal (ventral) view of the body; VI and VIII show the posterior (dorsal) view. -

Double-Bellied Superior Rectus Muscle
Surgical and Radiologic Anatomy (2019) 41:713–715 https://doi.org/10.1007/s00276-019-02211-0 ANATOMIC VARIATIONS Double-bellied superior rectus muscle Satheesha B. Nayak1 · Surekha D. Shetty1 · Naveen Kumar1 · Ashwini P. Aithal1 Received: 3 September 2018 / Accepted: 23 February 2019 / Published online: 7 March 2019 © Springer-Verlag France SAS, part of Springer Nature 2019 Abstract Congenital variations of extraocular muscles are rare. We report a double-bellied superior rectus muscle, observed in an adult male cadaver aged 70 years. The superior rectus muscle had two equal-sized bellies, which took separate origins from the common tendinous ring and united to form a common belly 1 cm before the insertion. Due to the duplication, the muscle extended laterally beyond the levator palpebrae superioris. Both its bellies were supplied by oculomotor nerve. To the best of our knowledge, this is the first report on doubling of the belly of the superior rectus muscle. Keywords Extraocular · Orbit · Superior rectus muscle · Eye movement · Strabismus Introduction Case report Voluntary movements of the eyeball are performed by six During dissection classes for the first-year medical students, extraocular muscles, namely superior rectus muscle, the we observed a unique variation in the right orbit of an adult inferior rectus muscle, medial rectus muscle, lateral rectus male cadaver aged 70 years. The cadaver was donated to the muscle, superior oblique muscle, and inferior oblique mus- department for teaching and research purpose. No history of cles. Variations of these muscles can result in restrictions of strabismus or visual defects is available. The variation was movements of eyeball, causing strabismus. -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

A- and V-Patterns and Oblique Muscle Overaction A- and V-Patterns
18 A- and V-Patterns and Oblique Muscle Overaction A- and V-Patterns Clinical Features Etiology Management with Horizontal Rectus Muscle Offsets Inferior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Oblique Weakening Procedures Complications A- and V-patterns of strabismus are changes in the horizontal deviation as the patient looks up and down. They are usually associated with oblique dysfunction, either overaction or paresis. Primary oblique muscle overaction is when an oblique muscle is too strong for its antagonist and there is no known cause. Secondary oblique overaction is caused by a paresis of the antagonist muscle. A superior oblique paresis results in inferior oblique overaction, and inferior oblique paresis results in superior oblique overaction. This chapter covers the management of A- and V- patterns and primary oblique muscle overaction. A- and V-Patterns CLINICAL FEATURES A-patterns are defined as increasing divergence in down gaze (>10 prism diopters [PD]), whereas Vpatterns are increased divergence (>15 prism diopters) in up gaze. The type of A- or V-pattern helps identify the cause. Superior oblique paresis produces a V-pattern, arrow subtype, with convergence in down gaze. The arrow pattern subtype indicates a lack of abduction in down gaze, the field of action of the superior oblique muscles. Inferior oblique overaction, on the other hand, has a V-pattern, Y subtype, with increased abduction in up gaze. The Y-pattern occurs because the field of action of the inferior oblique muscles is up gaze and they are abductors. Lambda subtype is typically associated with superior oblique overaction, with increased abduction in down gaze, because the field of action is in down gaze. -

Kinesiology of the Head and Spine
Oatis_CH20_389-411.qxd 4/18/07 3:10 PM Page 389 PART Kinesiology of the Head III and Spine Vertebral body Inferior articular process of superior vertebra Superior articular process of inferior vertebra Spinous process UNIT 4: MUSCULOSKELETAL FUNCTIONS WITHIN THE HEAD Chapter 20: Mechanics and Pathomechanics of the Muscles of the Face and Eyes Chapter 21: Mechanics and Pathomechanics of Vocalization Chapter 22: Mechanics and Pathomechanics of Swallowing Chapter 23: Structure and Function of the Articular Structures of the TMJ Chapter 24: Mechanics and Pathomechanics of the Muscles of the TMJ Chapter 25: Analysis of the Forces on the TMJ during Activity UNIT 5: SPINE UNIT Chapter 26: Structure and Function of the Bones and Joints of the Cervical Spine Chapter 27: Mechanics and Pathomechanics of the Cervical Musculature Chapter 28: Analysis of the Forces on the Cervical Spine during Activity Chapter 29: Structure and Function of the Bones and Joints of the Thoracic Spine Chapter 30: Mechanics and Pathomechanics of the Muscles of the Thoracic Spine Chapter 31: Loads Sustained by the Thoracic Spine Chapter 32: Structure and Function of the Bones and Joints of the Lumbar Spine Chapter 33: Mechanics and Pathomechanics of Muscles Acting on the Lumbar Spine Chapter 34: Analysis of the Forces on the Lumbar Spine during Activity Chapter 35: Structure and Function of the Bones and Joints of the Pelvis Chapter 36: Mechanics and Pathomechanics of Muscle Activity in the Pelvis Chapter 37: Analysis of the Forces on the Pelvis during Activity 389 Oatis_CH20_389-411.qxd 4/18/07 3:10 PM Page 390 PARTUNIT 4V MUSCULOSKELETAL FUNCTIONS WITHIN THE HEAD he preceding three units examine the structure, function, and dysfunction of the upper extremity, which is part of the appendicular skeleton. -

Muscles of the Head, Neck, and Torso
MusclesMuscles ofof thethe Head,Head, Neck,Neck, andand TorsoTorso DanilDanil HHammoudi.MDammoudi.MD MuscleMuscle myofibril Fiber/NerveFiber/Nerve motor end plate TerminalTerminal sarcomere I-band A-band Z-line sarcolemma motor neuron endomysium SomeSome definitiondefinition •• aponeurosisaponeurosis -- AA sheetlikesheetlike fibrousfibrous membrane,membrane, resemblingresembling aa flattenedflattened tendon,tendon, thatthat servesserves asas aa fasciafascia toto bindbind musclesmuscles togethertogether oror asas aa meansmeans ofof connectingconnecting musclemuscle toto bobone.ne. anyany ofof thethe deeperdeeper andand thickerthicker fasciafascia thatthat attachattach musclesmuscles toto bobones;nes; resembleresemble flattenedflattened tendons,tendons, •• ffasciaascia -- aa sheetsheet oror bandband ofof fibroufibrouss connectiveconnective tissuetissue separatingseparating oror bindingbinding togethertogether musclesmuscles andand organsorgans etcetc •• Ligament:Ligament: AA ligaligamentment isis aa toughtough bandband ofof connectiveconnective tisstissueue thatthat connectsconnects variousvarious structuresstructures suchsuch asas twotwo bones.bones. "Ligament""Ligament" isis aa fittingfitting term;term; itit comescomes fromfrom thethe LatinLatin "ligare""ligare" meaningmeaning "to"to bindbind oror tie.tie. •Tendon: The tissue by which a muscle attaches to bone. A tendon is somewhat flexible, but fibrous and tough. MusclesMuscles ofof thethe headhead •• EEpicranius.:picranius.: OccipitofrontalisOccipitofrontalis TheThe epicraniusepicranius -

The Anatomy of the Head of Ctenosaura Pectinata (Iguanidae)
MISCELLANEOUS PUBLICATIONS MUSEUM OF ZOOLOGY, UNIVERSITY OF MICHIGAN, NO. 94 The Anatomy of the Head of Ctenosaura pectinata (Iguanidae) BY THOMAS M. OELRICH ANN ARBOR MUSEUM OF ZOOLOGY, UNIVERSITY OF MICHIGAN March 21, 1956 LIST OF THE MISCELLANEOUS PUBLICATIONS OF THE MUSEUM OF ZOOLOGY, UNIVERSITY OF MICHIGAN Address inquiries to the Director of the Museum of Zoology, Ann Arbor, Michigan *On sale from the University Press, 311 Maynard St., Ann Arbor, Michigan. Bound in Paper No. 1. Directions for Collecting and Preserving Specimens of Dragonflies for Museum Purposes. By E. B. Williamson. (1916) Pp. 15, 3 figures . No. 2. An Annotated List of the Odonata of Indiana. By E. B. Williamson. (1917) Pp. 12, 1 map . No. 3. A Collecting Trip to Colombia, South America. By E. B. Williamson. (1918) Pp. 24 (Out of print) No. 4. Contributions to the Botany of Michigan. By C. K. Dodge. (1918) Pp. 14 No. 5. Contributions to the Botany of Michigan, 11. By C. K. Dodge. (1918) Pp. 44, 1 map No. 6. A Synopsis of the Classification of the Fresh-water Mollusca of North America, North of Mexico, and a Catalogue of the More Recently Described Species, with Notes. By Bryant Walker. (1918) Pp. 213, 1 plate, 233 figures No. 7. The Anculosae of the Alabama River Drainage. By Calvin Goodrich. (1922) Pp. 57, 3 plates . No. 8. The Amphibians and Reptiles of the Sierra Nevada de Santa Marta, Colombia. By Alexander G. Ruthven. (1922) Pp. 69, 13 plates, 2 figures, 1 map No. 9. Notes on American Species of Triacanthagyna and Gynacantha.