Anatomy of Small Intestine Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Introduction to Anatomy of the Abdomen the Region Between: Diaphragm and Pelvis
Introduction to Anatomy of the Abdomen The region between: Diaphragm and pelvis. Boundaries: • Roof: Diaphragm • Posterior: Lumbar vertebrae, muscles of the posterior abdominal wall • Infrerior: Continuous with the pelvic cavity, superior pelvic aperture • Anterior and lateral: Muscles of the anterior abdominal wall Topography of the Abdomen (PLANES)..1/2 TRANSVERSE PLANES • Transpyloric plane : tip of 9th costal cartilages; pylorus of stomach, L1 vertebra level. • Subcostal plane: tip of 10th costal cartilages, L2-L3 vertebra. • Transtubercular plane: L5 tubercles if iliac crests; L5 vertebra level. • Interspinous plane: anterior superior iliac spines; promontory of sacrum Topography of the Abdomen (PLANES)..2/2 VERTICAL PLANES • Mid-clavicular plane: midpoint of clavicle- mid-point of inguinal ligament. • Semilunar line: lateral border of rectus abdominis muscle. Regions of the Abdomen..1/2 4 2 5 9 regions: • Umbilical (1) 8 1 9 • Epigastric (2) • Hypogastric (Suprapubic) (3) • Right hypochondriacum (4) 6 3 7 • Left hypochondrium (5) • Right Iliac (Inguinal) (6) • Left Iliac (Inguinal) (7) • Right lumbar (8) • Left lumbar (9) Regions of the Abdomen..2/2 1 2 4 Quadrants: • Upper right quadrant (1) 3 4 • Upper left quadrant (2) • Lower right quadrant (3) • Lower left quadrant (4) Dermatomes Skin innervation: • lower 5 intercostal nerves • Subcostal nerve • L1 spinal nerve (ilioinguinal+iliohypogastric nerves). Umbilical region skin = T10 Layers of Anterior Abdominal Wall Skin Fascia: • Superficial fascia: • Superficial fatty layer(CAMPER’S -

Short Bowel Syndrome with Intestinal Failure Were Randomized to Teduglutide (0.05 Mg/Kg/Day) Or Placebo for 24 Weeks
Short Bowel (Gut) Syndrome LaTasha Henry February 25th, 2016 Learning Objectives • Define SBS • Normal function of small bowel • Clinical Manifestation and Diagnosis • Management • Updates Basic Definition • A malabsorption disorder caused by the surgical removal of the small intestine, or rarely it is due to the complete dysfunction of a large segment of bowel. • Most cases are acquired, although some children are born with a congenital short bowel. Intestinal Failure • SBS is the most common cause of intestinal failure, the state in which an individual’s GI function is inadequate to maintain his/her nutrient and hydration status w/o intravenous or enteral supplementation. • In addition to SBS, diseases or congenital defects that cause severe malabsorption, bowel obstruction, and dysmotility (eg, pseudo- obstruction) are causes of intestinal failure. Causes of SBS • surgical resection for Crohn’s disease • Malignancy • Radiation • vascular insufficiency • necrotizing enterocolitis (pediatric) • congenital intestinal anomalies such as atresias or gastroschisis (pediatric) Length as a Determinant of Intestinal Function • The length of the small intestine is an important determinant of intestinal function • Infant normal length is approximately 125 cm at the start of the third trimester of gestation and 250 cm at term • <75 cm are at risk for SBS • Adult normal length is approximately 400 cm • Adults with residual small intestine of less than 180 cm are at risk for developing SBS; those with less than 60 cm of small intestine (but with a -
5- Small Intestines Edited.Pdf
Small Intestines Lecture (5) . Important . Doctors Notes Please check our Editing File . Notes/Extra explanation هذا العمل مبني بشكل أساسي على عمل دفعة 436 مع المراجعة {ومنْْيتو َ ّكْْع َلْْا ِّْللْفَهُوْْحس بهْ} َ َ َ َ َ َ َ َ َ ُ ُ والتدقيق وإضافة المﻻحظات وﻻ يغني عن المصدر اﻷساسي للمذاكرة . Objectives At the end of the lecture, students should be able to: List the different parts of small intestine. Describe the anatomy of duodenum, jejunum & ileum regarding: the shape, length, site of beginning & termination, peritoneal covering, arterial supply & lymphatic drainage. Differentiate between each part of duodenum regarding the length, level & relations. Differentiate between the jejunum & ileum regarding the characteristic anatomical features of each of them. Abdomen o What is Mesentery? o It is a double layer attach the intestine to abdominal wall. If it has mesentery it is freely moveable. o The small intestines consist of two parts: • Fixed part (without mesentery) (retroperitoneal): duodenum • Free (movable) part (with mesentery): jejunum & ileum Jejunum & ileum Mesentery of SI L= liver, S=Spleen, SI=Small Intestine, AC=Ascending Colon, TC=Transverse Colon To see the second layer you should Abdomen (this slide is not important) remove the parietal peritoneum of posterior abdominal wall. The second layer consists of: Dr.ahmed fathalla’s notes: We you remove the anterior 1- ascending colon - any structure invaginates the abdominal wall, you will find 2- cecum peritoneum has a certain the most superficial 3- descending colon degree of mobility 4- duodenum structures are: 5- pancreas - we have three levels related to 1- liver abdominal structures: 2- stomach 6- spleen 1- (Part of the GIT) it is mobile and 3- transvers colon And behind the 2nd layer, there are completely covered by the 4- small intestine) the other non-GIT structures like peritoneum, because it has kidney, Aorta and IVC invaginated the peritoneum. -

Esophageal Reconstruction Using a Pedicled Jejunum with Microvascular Augmentation
Ann Thorac Cardiovasc Surg 2011; 17: 103–109 Review Esophageal Reconstruction Using a Pedicled Jejunum with Microvascular Augmentation Takushi Yasuda, MD and Hitoshi Shiozaki, MD The pedicled colon segment is widely accepted as a substitute to the gastric tube in esopha- geal reconstruction of cases where the stomach is not available. The usefulness of reconstruc- tion with a pedicled jejunum has also been reported in recent years. In order to make a long jejunal graft, at least the second and third jejunal vessels have to be severed. However, this leads to a decrease of circulation in the pedicled jejunum. This poor circulation was primar- ily responsible for the high rates of gangrene and mortality (22.2% and 46.5%, respectively) in the beginnings of jejunal reconstruction. Advances in microsurgery have now enabled surgeons to overcome these disadvantages, as a result, both the rates of gangrene and mor- tality have decreased to almost zero since the addition of microvascular anastomosis with the jejunal vessels and the internal thoracic vessels. At present, the reconstruction using a pedi- cled jejunum is a safe operation that provides such advantages as a low incidence of intrinsic disease, more active transport of food, and a lower rate of regurgitation by peristalsis, com- pared with the reconstruction using the pedicled colon. The disadvantage of the procedure is the relatively high rate of anastomotic leakage (11.1% to 19.2%). Improvements in the surgi- cal procedures to overcome this disadvantage are, therefore, needed before it can be recom- mended without any reservations. Key words: esophageal reconstruction, jejunum, microvascular anastomosis, complication Introduction stomach is necessary. -

Molecular Embryology of the Foregut
Author manuscript, published in "Journal of Pediatric Gastroenterology & Nutrition 2011;52 Suppl 1:S2-3" DOI : 10.1097/MPG.0b013e3182105a1a Molecular embryology of the foregut. Sandrine Faure, Ph.D. and Pascal de Santa Barbara, Ph.D. INSERM ERI 25, EA4202, Muscle and Pathologies Address correspondence and reprint requests to Pascal de Santa Barbara, Ph.D., 371 Avenue Doyen Giraud, 34295 Montpellier, FRANCE (e-mail: [email protected]). Supported by grants from Agence Nationale pour la Recherche (ANR-07-JCJC-0112), Association Française contre les Myopathies, Région Languedoc-Roussillon (Chercheur d’Avenir) and Ligue Contre le Cancer (Comité de l’Aude). Key words: foregut; Shh; Bmp; adriomycin; endodermal-mesenchymal interaction inserm-00595617, version 1 - 25 May 2011 The digestive and respiratory systems have different physiological functions (nutrition, food transit and evacuation for the first; breathing and oxygen supply to the blood for the second) and are generally considered and studied as two independent structures. Nevertheless, although at birth they are separated, they both derive from a common and transient developmental structure, the foregut, which is the anterior part of the gastrointestinal (GI) tract (1). The GI tract is a remarkably complex, three-dimensional, specialized and vital system that is derived from a simple tube-like structure. The vertebrate GI tract includes the luminal digestive system (i.e., esophagus, stomach, intestine and colon, which we will designate on the whole as "gut") and the GI-tract derivatives (i.e., thyroid, lungs, liver and pancreas). The gut is composed of three germ layers: mesoderm (which forms the smooth muscle layer), endoderm (which forms the epithelial lining) and ectoderm (which includes the enteric nervous system). -

Small & Large Intestine
Small & Large Intestine Gastrointestinal block-Anatomy-Lecture 6,7 Editing file Objectives Color guide : Only in boys slides in Green Only in girls slides in Purple important in Red At the end of the lecture, students should be able to: Notes in Grey ● List the different parts of small intestine. ● Describe the anatomy of duodenum, jejunum & ileum regarding: (the shape, length, site of beginning & termination, peritoneal covering, arterial supply & lymphatic drainage) ● Differentiate between each part of duodenum regarding the length, level & relations. ● Differentiate between the jejunum & ileum regarding the characteristic anatomical features of each of them. ● List the different parts of large intestine. ● List the characteristic features of colon. ● Describe the anatomy of different parts of large intestine regarding: (the surface anatomy, peritoneal covering, relations, arterial & nerve supply) Small intestine The small intestine divided into : Fixed Part (No Mesentery): Free (Movable) Part (With Parts Duodenum* Mesentery): Jejunum & Ileum Shape C-shaped loop coiled tube Length 10 inches 6 meters (20 feet) Transverse Colon separates the Beginning At pyloro-duodenal junction at duodeno-jejunal flexure stomach/liver from the jejunum/ileum Termination At duodeno-jejunal flexure at ileo-ceacal flexure Peritoneal Covering Retroperitoneal mesentery of small intestine Divisions 4 parts --------- Foregut (above bile duct opening in 2nd part )& Midgut Embryological origin Midgut (below bile duct opening in 2nd part) So 2nd part has double -

Digestive System
Naziha Sultan Ahmed, BVMS, MSc Scientific degree (Assis. Prof.), Department of Anatomy College of Veterinary Medicine, University of Mosul, Mosul, Iraq https://orcid.org/0000-0002-2856-8277 https://www.researchgate.net/profile/Naziha_Ahmed Anatomy | Part 18| 2nd year 2019 Digestive System Fixation of the liver (Ligaments of the liver): 1-Lesser omentum: consist of two parts: a/Hepatogastric ligament: connect between hepatic porta and lesser curvature of the stomach . b/Hepatoduodenal ligament: connect between hepatic porta and the cranial part of the duodenum. 2-Coronary ligament: connect between the parietal (diaphragmatic ) surface of liver, with the diaphragm and the caudal vena cava. 3-Falciform ligament: connect between the notch of round ligament in the liver and the sternal part of the diaphragm. 4-Round ligament: the residue (remnants) of the umbilical vein of the fetus. 5-Hepatorenal ligament: connect between the right lobe of liver and the right kidney. 6-Right & left triangular ligaments: connect between the dorsal border of right and left lobes of the liver and the diaphragm . Both ligaments continue medially with the coronary ligament. CouAnatomy | Digestive system | Assis. Prof. Naziha Sultan Ahmed Page | 1 The pancreas: Pancreas has V-shape. It consists of base and two limbs (right & left limbs). *In horse: large pancreas body perforated by portal vein and long left limb, with short right limb (because of large size of cecum in horse ). The horse pancreas has two ducts: 1-Chief pancreatic duct: opens with bile duct at the major duodenal papilla. 2-Accessory pancreatic duct: opens at the minor duodenal papilla. *In dog: pancreas notched by the portal vein. -

Anatomy of the Digestive System
The Digestive System Anatomy of the Digestive System We need food for cellular utilization: organs of digestive system form essentially a long !nutrients as building blocks for synthesis continuous tube open at both ends !sugars, etc to break down for energy ! alimentary canal (gastrointestinal tract) most food that we eat cannot be directly used by the mouth!pharynx!esophagus!stomach! body small intestine!large intestine !too large and complex to be absorbed attached to this tube are assorted accessory organs and structures that aid in the digestive processes !chemical composition must be modified to be useable by cells salivary glands teeth digestive system functions to altered the chemical and liver physical composition of food so that it can be gall bladder absorbed and used by the body; ie pancreas mesenteries Functions of Digestive System: The GI tract (digestive system) is located mainly in 1. physical and chemical digestion abdominopelvic cavity 2. absorption surrounded by serous membrane = visceral peritoneum 3. collect & eliminate nonuseable components of food this serous membrane is continuous with parietal peritoneum and extends between digestive organs as mesenteries ! hold organs in place, prevent tangling Human Anatomy & Physiology: Digestive System; Ziser Lecture Notes, 2014.4 1 Human Anatomy & Physiology: Digestive System; Ziser Lecture Notes, 2014.4 2 is suspended from rear of soft palate The wall of the alimentary canal consists of 4 layers: blocks nasal passages when swallowing outer serosa: tongue visceral peritoneum, -

Anatomy of the Small Intestine
Anatomy of the small intestine Make sure you check this Correction File before going through the content Small intestine Fixed Free (Retro peritoneal part) (Movable part) (No mesentery) (With mesentery) Duodenum Jejunum & ileum Duodenum Shape C-shaped loop Duodenal parts Length 10 inches Length Level Beginning At pyloro-duodenal Part junction FIRST PART 2 INCHES L1 (Superior) (Transpyloric Termination At duodeno-jejunal flexure Plane) SECOND PART 3 INCHES DESCENDS Peritoneal Retroperitoneal (Descending FROM L1 TO covering L3 Divisions 4 parts THIRD PART 4 INCHES L3 (SUBCOTAL (Horizontal) PLANE) Embryologic Foregut & midgut al origin FOURTH PART 1 INCHES ASCENDS Lymphatic Celiac & superior (Ascending) FROM L3 TO drainage mesenteric L2 Arterial Celiac & superior supply mesenteric Venous Superior mesenteric& Drainage Portal veins Duodenal relations part Anterior Posterior Medial Lateral First part Liver Bile duct - - Gastroduodenal artery Portal vein Second Part Liver Transverse Right kidney Pancreas Right colic flexure Colon Small intestine Third Part Small intestine Right psoas major - - Superior Inferior vena cava mesenteric vessels Abdominal aorta Inferior mesenteric vessels Fourth Part Small intestine Left psoas major - - Openings in second part of the duodenum Opening of accessory Common opening of bile duct pancreatic duct (one inch & main pancreatic duct: higher): on summit of major duodenal on summit of minor duodenal papilla. papilla. Jejunum & ileum Shape Coiled tube Length 6 meters (20 feet) Beginning At duodeno-jejunal flexur -
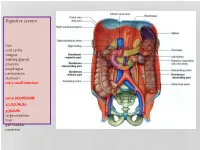
Digestive System
Digestive system Lips oral cavity tongue salivary glands pharynx esophagus peritoneum stomach m6-7 small intestine: cm25 DEODENUM: 2/5JEJUNUM: 3/5ILIUM: large intestine liver gall bladder pancreas :Duodenum Sup. Part Descending part Horizontal part Ascending part Major duodenal papilla Minor duodenal papilla : JEJUNUM / ILIUM From duodenojejunal curvature To Iliocecal Different jejunum & ilium 3Tenia coli: sigmoid 2 / rectum 0 Houstra / saccule Appendices epiploicae : No in Appendix / cecum / rectum Many in sigmoid DIFFERENT BETWEEN SMALL AND LARGE INTESTINE large intestine 1.5m Cecum appendix ascending colon transverse colon descending colon sigmoid colon rectum anal canal McBurneys point ascending colon transverse colon descending colon sigmoid colon :Rectum cm 12 Sacral flexure Puborectalis muscle Perineal flexure Rectum Ampulla : Anal canal cm 4 sup. = anal column / anal valve / anal sinus / pectinate line 2/3 Hiltons white line .inf 1/3 :Anal sphincter Internal sphincter External sphincter: deep / superficial / subcutaneous Liver: 1.5 kgr Located in Rt. & lf. Hypochondriac & epigastric region Surfaces: Sup. Anterior Surface: falciform ligament Inf. Surface: H shape fissure / porta hepatis / quadrate lobe / qudate lobe Post. Surface: bare area Rt. Surface: ribs 7-11 / Rt. lung Liver viewed from posterior Liver viewed from inferior Liver viewed from inferior Liver viewed from posterior :Liver vasculature 20%Hepatic artery 80%Portal vein Supra hepatic vein IVC :Nerve Sympathetic Parasympathetic From Vagus+ Phernic + celiac :Gall bladder Located in inf. Surface of liver cm7-10 Length: cm3-4 Wide: :Structure Fundus Body Infundibulum Neck Systic duct :Pancreas 2–L1 L cm15-20 Length: cm3Wide: cm2 Thickness: gram 90 :Structure Head :Uncinate process / sup. Mesenteric artery Neck: portal vein / sup. -

Unit #2 - Abdomen, Pelvis and Perineum
UNIT #2 - ABDOMEN, PELVIS AND PERINEUM 1 UNIT #2 - ABDOMEN, PELVIS AND PERINEUM Reading Gray’s Anatomy for Students (GAFS), Chapters 4-5 Gray’s Dissection Guide for Human Anatomy (GDGHA), Labs 10-17 Unit #2- Abdomen, Pelvis, and Perineum G08- Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) G09A- Peritoneum, GI System Overview and Foregut (Dr. Albertine) G09B- Arteries, Veins, and Lymphatics of the GI System (Dr. Albertine) G10A- Midgut and Hindgut (Dr. Albertine) G10B- Innervation of the GI Tract and Osteology of the Pelvis (Dr. Albertine) G11- Posterior Abdominal Wall (Dr. Albertine) G12- Gluteal Region, Perineum Related to the Ischioanal Fossa (Dr. Albertine) G13- Urogenital Triangle (Dr. Albertine) G14A- Female Reproductive System (Dr. Albertine) G14B- Male Reproductive System (Dr. Albertine) 2 G08: Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) At the end of this lecture, students should be able to master the following: 1) Overview a) Identify the functions of the anterior abdominal wall b) Describe the boundaries of the anterior abdominal wall 2) Surface Anatomy a) Locate and describe the following surface landmarks: xiphoid process, costal margin, 9th costal cartilage, iliac crest, pubic tubercle, umbilicus 3 3) Planes and Divisions a) Identify and describe the following planes of the abdomen: transpyloric, transumbilical, subcostal, transtu- bercular, and midclavicular b) Describe the 9 zones created by the subcostal, transtubercular, and midclavicular planes c) Describe the 4 quadrants created -

Carcinoid Tumor of the Minor Papilla in Complete Pancreas Divisum Presenting As Recurrent Abdominal Pain Yong Gil Kim, Tae Nyeun Kim*, Kyeong Ok Kim
Kim et al. BMC Gastroenterology 2010, 10:17 http://www.biomedcentral.com/1471-230X/10/17 CASE REPORT Open Access Carcinoid tumor of the minor papilla in complete pancreas divisum presenting as recurrent abdominal pain Yong Gil Kim, Tae Nyeun Kim*, Kyeong Ok Kim Abstract Background: Tumors of the minor papilla of the duodenum are extremely rare, and they are mostly neuroendocrine tumors, such as somatostatinomas and carcinoid tumors. However, true incidence of carcinoid tumors in minor papilla might be much higher, because patients with minor papillary tumors usually remain asymptomatic. We report a very unusual case of carcinoid tumor in a patient with complete pancreas divisum with a review of the literature. Case presentation: A 56-year-old female patient was referred for evaluation of pancreatic duct dilatation noted on abdominal ultrasonography and computerized tomography. She complained of intermittent epigastric pain for 6 months. A MRCP and ERCP revealed complete pancreas divisum with dilatation of the main pancreatic duct. On duodenoscopy, a small, yellows, subepithelial nodule was visualized at the minor papilla; biopsy of this lesion revealed a carcinoid tumor. She underwent a pylorus-preserving pancreaticoduodenectomy. The histologic evaluation showed a single nodule, 1 cm in diameter, in the submucosa with duodenal and vascular invasion and metastasis to the regional lymph nodes. Conclusion: Although the size of the carcinoid tumor was small and the tumor was hormonally inactive, the concomitant pancreas divisum led to an early diagnosis, the tumor had aggressive behavior. Carcinoid tumors of the minor papilla should be included in the differential diagnosis of recurrent abdominal pain or pancreatitis of unknown cause.