Meeting Agenda (Public Session) Primary Care Commissioning
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nottinghamshire Local Flood Risk Management Strategy 2016 - 2021
Nottinghamshire Local Flood Risk Management Strategy 2016 - 2021 Final June 2016 Nottinghamshire Local Flood Risk Management Strategy Review Local Flood Risk Management Strategy Rev Date Details Prepared by Checked by Approved by 1 August 2013 Outline Local Flood Risk Hannah Andy Wallace, Gary Wood, Group Management Strategy for O’Callaghan, Flood Risk Manager Highways Consultation Flood Risk Manager Planning, Access Management and Officer (Project Commissioning Manager) (Project Executive) 2 December Local Flood Risk Management Amy Ruocco, Sarah Kelly, Carl Pelling 2014 Strategy – Draft for Client Water and Principal Associate Comment Flood Risk Consultant Consultant (URS) (URS) (URS) 3 June 2015 Local Flood Risk Management Amy Ruocco, Sarah Kelly, Carl Pelling Strategy – Second Draft for Water and Principal Associate Client Comment Flood Risk Consultant Consultant AECOM AECOM AECOM (formerly URS) (Formerly URS) (Formerly URS) 4 July 2015 Local Flood Risk Management Amy Ruocco, Sarah Kelly, Carl Pelling Strategy – Final Draft for Water and Principal Associate Consultation Flood Risk Consultant Consultant AECOM AECOM AECOM 5 October Local Flood Risk Management Derek Hair Andy Wallace Transport and 2015 Strategy – Final Draft for Highways Principal Project Flood Risk Consultation Committee Engineer Manager AECOM 6 December Local Flood Risk Management Derek Hair Clive Wood Transport and 2015 Strategy – Final Draft for Highways Principal Project Flood Risk Consultation Committee Engineer Manager 7 June 2016 Local Flood Risk Management Derek -

Statement of Persons Nominated, Notice of Poll and Situation of Polling Stations
STATEMENT OF PERSONS NOMINATED, NOTICE OF POLL AND SITUATION OF POLLING STATIONS Nottinghamshire County Council Election of a County Councillor for Kirkby South Division Notice is hereby given that: 1. A poll for the election of a County Councillor for Kirkby South Division will be held on Thursday 6 May 2021, between the hours of 7:00 am and 10:00 pm. 2. One County Councillor is to be elected. 3. The names, home addresses and descriptions of the Candidates remaining validly nominated for election and the names of all persons signing the Candidates nomination paper are as follows: Name of Home Address Description (if Names of Signatories Candidate any) Proposers(+), Seconders(++) & Assentors FLOWERS (Address in The Conservative Hancock Kelly(+) Sellens Adam P(++) Carol Anne Ashfield District) Party Candidate GILBERT 30 Lime Tree Labour Party Butler Duncan(+) Gilbert Jill V(++) Donna Samantha Avenue, Kirkby In Jane Ashfield, Nottinghamshire, NG17 8BJ WILLIAMSON 11 Church Hill, Ashfield Madden Rachel E(+) Grounds Dale A(++) Daniel Frederick Kirkby In Ashfield, Independents Nottinghamshire, Working All Year NG17 8LN Round 4. The situation of Polling Stations and the description of persons entitled to vote thereat are as follows: Situation of Polling Station Station Number Ranges of electoral register numbers of persons entitled to vote thereat Nuncar Court, Nuncargate Road, Kirkby In Ashfield, Nottingham 29 AKW1-1 to AKW1-2186 Acacia Centre, Acacia Avenue, Annesley Woodhouse, Nottingham 30 AKW2-1 to AKW2-1257 Acacia Centre, Acacia Avenue, -

Adopted Local Plan Still Remain Essential to the Local Plan Review
ASHFIELD LOCAL PLAN REVIEW ADOPTED NOVEMBER 2002 FOREWORD The previous Ashfield Local Plan was adopted in December 1995 with a plan period to 2001. Following adoption of the Nottinghamshire Structure Plan Review in November 1996 work commenced on the Ashfield Local Plan Review with a plan period to 2011. In July 1997 consultation took place on the Main Issues and Site Allocations Report. The Council's response to comments made on the report were subsequently published on 4th March 1999 together with the Ashfield Local Plan Review Deposit Draft. Following detailed consideration of responses to the Deposit Draft Plan and revised Government guidance, a Second Deposit Local Plan was prepared to include proposed changes to the Deposit Draft Local Plan. The Second Deposit Local Plan was subsequently approved on 11th May 2000 for public consultation. An Inquiry into unresolved objections to the Ashfield Local Plan Review was held between 13th February and 22nd May 2001. The Inspector considered all of the outstanding objections to the Plan together with a number of informal 'Inquiry Changes’ (IC’s) that the Council proposed at the time of the Inquiry. The Inspector’s Report on the Local Plan Inquiry was released for public consideration on 16th January 2002. The Council considered all of the Inspector’s recommendations, and subsequently the 'Statement of Decisions on the Inspector's Report & Proposed Modifications to the Ashfield Local Plan Review' was published for consultation on 9th May 2002. A report of consultation was published in July 2002 indicating that no further material changes were required to the plan. -
DRAFT Greater Nottingham Blue-Green Infrastructure Strategy
DRAFT Greater Nottingham Blue-Green Infrastructure Strategy July 2021 Contents 1. Introduction 3 2. Methodology 8 3. Blue-Green Infrastructure Priorities and Principles 18 4. National and Local Planning Policies 23 5. Regional and Local Green Infrastructure Strategies 28 6. Existing Blue-Green Infrastructure Assets 38 7. Blue-Green Infrastructure Strategic Networks 62 8. Ecological Networks 71 9. Synergies between Ecological and the Blue-Green Infrastructure Network 89 Appendix A: BGI Corridor Summaries 92 Appendix B: Biodiversity Connectivity Maps 132 Appendix C: Biodiversity Opportunity Areas 136 Appendix D: Natural Environment Assets 140 Appendix D1: Sites of Special Scientific Interest 141 Appendix D2: Local Nature Reserves 142 Appendix D3: Local Wildlife Sites 145 Appendix D4: Non-Designated 159 1 Appendix E: Recreational Assets 169 Appendix E1: Children’s and Young People’s Play Space 170 Appendix E2: Outdoor Sports Pitches 178 Appendix E3: Parks and Gardens 192 Appendix E4: Allotments 199 Appendix F: Blue Infrastructure 203 Appendix F1: Watercourses 204 2 1. Introduction Objectives of the Strategy 1.1 The Greater Nottingham authorities have determined that a Blue-Green Infrastructure (BGI) Strategy is required to inform both the Greater Nottingham Strategic Plan (Local Plan Part 1) and the development of policies and allocations within it. This strategic plan is being prepared by Broxtowe Borough Council, Gedling Borough Council, Nottingham City Council and Rushcliffe Borough Council. It will also inform the Erewash Local Plan which is being progressed separately. For the purposes of this BGI Strategy the area comprises the administrative areas of: Broxtowe Borough Council; Erewash Borough Council; Gedling Borough Council; Nottingham City Council; and Rushcliffe Borough Council. -

NOTICE of POLL Election of Parish Councillors
NOTICE OF POLL Annesley & Felley Parish Council Election of Parish Councillors for Annesley Notice is hereby given that: 1. A poll for the election of Parish Councillors for Annesley will be held on Thursday 2 May 2019, between the hours of 7:00 am and 10:00 pm. 2. The number of Parish Councillors to be elected is ten. 3. The names, home addresses and descriptions of the Candidates remaining validly nominated for election and the names of all persons signing the Candidates nomination paper are as follows: Names of Signatories Name of Candidate Home Address Description (if any) Proposers(+), Seconders(++) & Assentors BLAZEWICZ-BELL (Address in Ashfield Independent Donald Roberts-Davis Melanie E J Sherlock Adam Antoni District) (+) (++) BLAZEWICZ-BELL (Address in Ashfield Independent Donald Roberts-Davis Derek A Sherlock (++) Rachael Elizabeth District) (+) BROWN 1 Glover Close, Ashfield Independents Terence J Sills (+) Ross A Cope (++) Ciaran Richard Annesley, Working All Year Nottinghamshire, Round NG15 0DH BUTLER Brunts House, 6 Crees Labour Party Carol A Evans (+) Cameron J Evans (++) Cheryl Yard, Kirkby-in- Ashfield, Nottingham, NG17 8LF COLLIER 53 Forest Road, Labour Party Carol A Evans (+) Cameron J Evans (++) Bob Annesley Woodhouse, Nottingham, NG17 9HA COPE 70 Byron Road, Ashfield Independents Terence J Sills (+) Ross A Cope (++) Ann Mary Annesley, Working All Year Nottinghamshire, Round NG15 0AG DAVIS (Address in Ashfield Labour Party Cathy Robinson (+) Craig R Spray (++) Don District) GIBBONS (Address in Ashfield Labour Party -

Publicise the Boating Association (TBA) Charts
Danny Brennan Chair East Midlands Waterway Partnership Welcome and introductions Presentations • River Witham • Canoe trails • Waterside fun days • Shared use of towpaths • Working in partnership • Encouraging use of the tidal Trent Summary; Q & A Networking • We’re 3 years old! Custodianship of 2000 miles of canals, rivers, heritage, environmental and property assets • 2014/15 spend – over £130m on charitable activities: • most applied to annual programme of planned maintenance and repair • £18m on larger infrastructure projects • nearly £11m on clearing and maintaining towpaths • nearly £7m on dredging - 130,000 tonnes of silt. • Exceptional volunteer input: • equivalent to nearly 60,000 days last year • East Midlands leading the way • worth £6.5m nationally – but also priceless. • Significant grant and development funding secured e.g. £830,000 for improvements on the Grantham Canal, working with Grantham Canal Society – now live! • We’re now full participants in 21st century – strong digital presence What’s all that for? • to maintain and improve the asset; • to widen access to and enjoyment of it and, in turn, • create that sense of common ownership of, and care for, the waterways we need for a sustainable future. Some ways to do so? • Increasing participation and activity – on and alongside the water; focus on young people • Re-connecting waterside communities • Developing partnerships with stakeholders • Improvements − Lincoln visitor mooring extension − New visitor moorings – Chesterfield Canal − Trent Lock welcome station / education base • Volunteering − New partnership members − East Midlands: over 35,600 hours in 2014/15 with 11 active adoptions • Events − Worksop Water Day − Radcliffe on Trent Bio-blitz − Nottingham event planning • Research, project testing/development − Nottingham Trent University partnership • Improvements − Tidal Trent − Visitor welcome at key destinations − Towpath harmony • Building partnerships − Existing (e.g. -
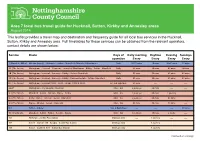
Area 7 Local Bus Travel Guide for Hucknall, Sutton, Kirkby And
Area 7 local bus travel guide for Hucknall, Sutton, Kirkby and Annesley areas August 2014 This leaflet provides a travel map and destination and frequency guide for all local bus services in the Hucknall, Sutton, Kirkby and Annesley area. Full timetables for these services can be obtained from the relevant operators, contact details are shown below. Service Route Days of Early morning Daytime Evening Sundays operation Every Every Every Every 1 (Mansfield Miller) Alfreton (hourly) - Huthwaite - Sutton - Mansfield - Mansfield Woodhouse Daily 10-20 mins 10 mins 30-60 mins 30 mins 3A (The threes) Nottingham - Hucknall - Newstead - Annesley Woodhouse - Kirkby - Sutton - Mansfield Daily 30 mins 30 mins 60 mins 60mins 3B (The threes) Nottingham - Hucknall - Annesley - Kirkby - Sutton - Mansfield Daily 30 mins 30 mins 60 mins 60 mins 3C (The threes) Nottingham - Hucknall - Annesley - Kirkby - Coxmoor Estate - Sutton - Mansfield Daily 30 mins 30 mins 60 mins 60 mins N3 (The threes) Nottingham - Hucknall (0030 - 0230) - Kirkby (0300 & 0330) Fri, Sat night bus 30 mins ---- ---- ---- 8AOT Nottingham - City Hospital - Hucknall Mon - Sat 3 journeys 60 mins ---- ---- 9.1 (The Nines) Mansfield - Sutton - Alfreton - Ripley - Derby Mon - Sat 2 journeys 60 mins 1 journey ---- 9.2 (The Nines) Derby - Ripley - Alfreton - Sutton - Mansfield Mon - Sat 2 journeys 60 mins 60 mins ---- 9.3 (The Nines) Ripley - Alfreton - Sutton - Mansfield Mon - Sat 30 mins 30 mins 30 mins ---- 9.3 Sutton - Alfreton Sun & Bank Hols ---- ---- ---- 60 mins 90 (The Ninety) Mansfield -

Strategic Plan for Greenwood Guiding the Creation of Nottinghamshire’S Community Forest Greenwood Strategic Plan for Greenwood
Strategic Plan for Greenwood guiding the creation of Nottinghamshire’s Community Forest Greenwood Strategic Plan for Greenwood September 2000 Key Partners The Countryside Agency Forestry Commission Ashfield District Council Broxtowe Borough Council Gedling Borough Council Mansfield District Council Newark & Sherwood District Council Nottingham City Council Nottinghamshire County Council This document has been kindly supported by: East Midlands Development Agency Environment Agency Greenwood foreword In 1991 a partnership of Local Authorities and National Bodies embarked on possibly the biggest and most ambitious undertaking in the history of Nottinghamshire. The idea was to transform almost one-fifth of the county for the benefit of all who live in or near it. Although many things have changed since then, CHAIR'S MESSAGE Greenwood - Nottinghamshire's Community Forest, has grown from just a vision to tangible results. May The Strategic Plan is a document that tries to bring be its because the concept, like all good ideas is to life the Community Forest concept. A strength of simple, a countryside on our doorstep; may be its the Plan is that it is all about working in because people can see the beneficial effects from "partnership" with various organisations and local creating extensive well-wooded areas around built-up communities, and it is essential that this approach areas; may be its because opportunities for economic continues over the forthcoming years. prosperity, biodiversity, education, health, social enrichment and improved quality of life can be Greenwood - is Nottinghamshire's Community captured and harnessed; or may be its because it can Forest. A forest that will benefit everyone, whether be seen as a sound investment for ourselves and our they be in the city, the towns or the vilages in the children to pass on to future generations. -

10 Cutts Row, Annesley Woodhouse, Nottinghamshire
10 CUTTS ROW ANNESLEY WOODHOUSE KIRKBY-IN-ASHFIELD NOTTINGHAMSHIRE NG17 9HY £100,000 VIEWING By appointment through the selling agent on (01623) 422000 16 Albert Street, Mansfield, Nottinghamshire, NG18 1EB TENURE Freehold • Mid Terrace Property • Off Street Parking for Two Cars • Two Bedrooms • Low Maintenance Garden • Two Reception Rooms • Fantastic Transport Links • Bathroom and Shower Room • Workshop / Outside Store / Home • Gas Central Heating Office 10 CUTTS ROW, ANNESLEY WOODHOUSE, NOTTINGHAMSHIRE DIRECTIONS From Derby Road if coming from Kirkby or from Annesley by-pass if heading from Hucknall and the M1 turn at the Badger Box pub onto Forest Road towards Annesley Woodhouse. Continue forward for half a mile taking the seventh right onto Fox Street. Take the first left onto Cuts Row where the property can be located towards the end of the road on the right-hand side. This surprisingly spacious property is located on a quiet street yet close to Kirkby-in- Ashfield town centre with great commuter links. It would be the perfect first step onto the property ladder or the ideal investment property. With two reception rooms, two good sized bedrooms, a modern bathroom and a shower room this property offers plenty of space and all for a great price! Externally this property offers a low maintenance rear garden with the addition of a substantial garden room which poses a variety of uses. What’s more there is that all- important off-street parking, a rare find for a terrace property. UPVC double glazed front entrance door opening into: LOUNGE 11’6” x 11’6” This welcoming reception room has some wonderful features to include a traditional fireplace and brick archway. -

STATEMENT of PERSONS NOMINATED, NOTICE of POLL and SITUATION of POLLING STATIONS Election of a County Councillor
STATEMENT OF PERSONS NOMINATED, NOTICE OF POLL AND SITUATION OF POLLING STATIONS Nottinghamshire County Council Election of a County Councillor for Ashfields Division Notice is hereby given that: 1. A poll for the election of a County Councillor for Ashfields Division will be held on Thursday 6 May 2021, between the hours of 7:00 am and 10:00 pm. 2. One County Councillor is to be elected. 3. The names, home addresses and descriptions of the Candidates remaining validly nominated for election and the names of all persons signing the Candidates nomination paper are as follows: Names of Signatories Name of Description (if Home Address Proposers(+), Seconders(++) & Candidate any) Assentors FELTON (Address in The Conservative Flowers Carina(+) Flowers Cameron Ashfield District) Party Candidate Shaun A(++) LAMB (Address in Labour Party Fleet Natalie S(+) Fleet Elodie-Mai(++) Stefan Ashfield District) ZADROZNY 74 Sutton Road, Ashfield Gent Sarah(+) Barsby Kier(++) Jason Bernard Kirkby In Ashfield, Independents Nottinghamshire, Working All Year NG17 8GZ Round 4. The situation of Polling Stations and the description of persons entitled to vote thereat are as follows: Situation of Polling Station Station Number Ranges of electoral register numbers of persons entitled to vote thereat Mobile Unit at The Changing Rooms, Off Bluebell Wood Way, Sutton in Ashfield 1 ASH1-1 to ASH1-2087 The Changing Rooms, Off Bluebell Wood Way, Sutton In Ashfield 2 ASH2-1 to ASH2-874 Bentinck Miners Welfare, Sutton Road, Kirkby In Ashfield, Nottingham 3 LAR1-1 to LAR1-1876 Bentinck Miners Welfare, Sutton Road, Kirkby In Ashfield, Nottingham 4 LAR2-1 to LAR2-1126 Willetts Court Community Centre, Limb Crescent, Sutton In Ashfield 5 LEM1-1 to LEM1-1345/1 Willetts Court Community Centre, Limb Crescent, Sutton In Ashfield 6 LEM2-1 to LEM2-1510/1 5. -

White's 1857 Directory of Derbyshire
DALE ABBEY PARISH. 261 took up his abode at Depedale, where he had been sometime, when about 1135, Sir Ralph, son of Lord Geremund, being out hunting, found his course intercepted by a morass; surveying this wild and secluded scene more closely, he at length perceived a column of smoke rising above the trees; making his way with difficulty through the plants and shrubs, he reached the place and found a rudely constructed hut, before it was a fire of sticks, and by it sat an aged man with unshorn hair and untrimmed beard. After hearing his tale, Sir Ralph proceeded to Derby, where it was verified, and the next day he returned with garments and food to the Hermit of the Dale—brought him tools and endowed him with the toll of his mill at Burgh, (Borrowash,) and encouraged him to fulfill the Virgin‟s pleasure. The recluse immediately commenced scooping out a habitation in the rock, which after several years labour was completed, as also an oratory at the foot of the hill for his patroness the Virgin. After living in this solitude for many years, he was found by a pilgrim attracted by the fame of his sanctity, stretched upon the floor of his cell apparently asleep, but dead. At his death, Serlo-de-Greudon, a knight of eminent valour and great wealth, who married the daughter of the above Sir Ralph, gave the place of Depedale to his godmother, who had a son, whom she educated for holy orders, that he might perform divine service in her chapel there; but a short time afterwards, and with her consent, he invited canons from Calke, and gave them Depedale. -

Skegby Road, Annesley Woodhouse, Notts, NG17 9JE £400 Per Calendar Month
CHARTERED SURVEYORS AUCTIONEERS VALUERS ESTATE AGENTS barnes EST. 1932 Skegby Road, Annesley Woodhouse, Notts, NG17 9JE £400 Per calendar month Located within this extremely popular and sought after location is this well presented and nicely decorated two double bedroom terrace home which benefits from a gas fired central heating system and upvc double glazing with carpets as fitted. The accommodation in brief comprises of modern fitted kitchen, front dining room and middle living room which has a lovely feature fireplace and open plan staircase to first floor. From the landing are two double bedrooms both with built in wardrobes plus a modern white 4 piece bathroom suite having separate shower cubicle. Outside there is a small rear patio / pebbled garden area. An early viewing is strongly recommended to appreciate the quality of accommodation on offer. Excellent references are required. Would suit a single or professional couple /small family. Not available for occupation until end of May. Please No Pets. DSS considered. EPC Rating D a copy of which can be obtained by request. Bond £500 VIEWING ACCOMPANIED WITH CURRENT TENANT NOTE:- W A BARNES LLP FEES PAYABLE AS FOLLOWS:- £20 inclusive of VAT per applicant over the age of 18 years to undertake a credit check. An additional fee of £150 inclusive of VAT per property will be charged when signing the 6 month Assured Shorthold Tenancy Agreement • Two double bedrooms • Nicely decorated throughout • Excellent references req • Mid Terraced Home • Carpets as fitted • Please No Pets • Gas centrally heated • Modern 4 piece bathroom • Ready end of May • upvc double glazing • Small rear patio garden • Bond £500 W A BARNES LLP PORTLAND SQUARE SUTTON IN ASHFIELD NOTTINGHAMSHIRE NG17 1DA tel 01623 554084 / 553929 fax 01623 550764 email [email protected] web www.wabarnes.co.uk barnes EST.