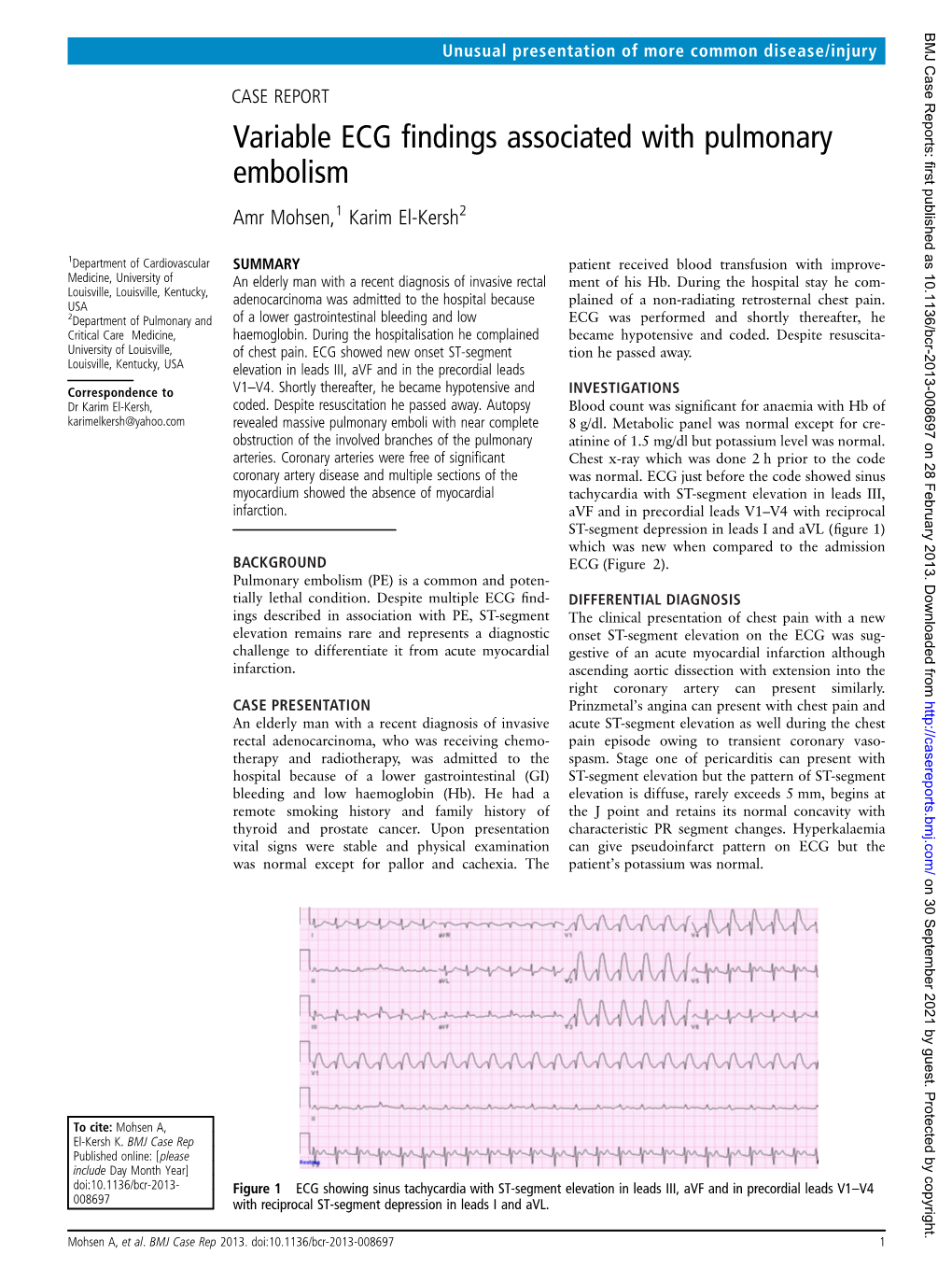
Variable ECG Findings Associated with Pulmonary Embolism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

USMLE – What's It
Purpose of this handout Congratulations on making it to Year 2 of medical school! You are that much closer to having your Doctor of Medicine degree. If you want to PRACTICE medicine, however, you have to be licensed, and in order to be licensed you must first pass all four United States Medical Licensing Exams. This book is intended as a starting point in your preparation for getting past the first hurdle, Step 1. It contains study tips, suggestions, resources, and advice. Please remember, however, that no single approach to studying is right for everyone. USMLE – What is it for? In order to become a licensed physician in the United States, individuals must pass a series of examinations conducted by the National Board of Medical Examiners (NBME). These examinations are the United States Medical Licensing Examinations, or USMLE. Currently there are four separate exams which must be passed in order to be eligible for medical licensure: Step 1, usually taken after the completion of the second year of medical school; Step 2 Clinical Knowledge (CK), this is usually taken by December 31st of Year 4 Step 2 Clinical Skills (CS), this is usually be taken by December 31st of Year 4 Step 3, typically taken during the first (intern) year of post graduate training. Requirements other than passing all of the above mentioned steps for licensure in each state are set by each state’s medical licensing board. For example, each state board determines the maximum number of times that a person may take each Step exam and still remain eligible for licensure. -

Thrombosis, Embolism, Infarction
Thrombosis, Embolism and Infarction THROMBOSIS Thrombus formation (called Virchow's triad): (1) endothelial injury, (2) stasis or turbulent blood flow (3) hypercoagulability of the blood Endothelial Injury Endothelial injury is particularly important for thrombus formation in the heart or the arterial circulation, where the normally high flow rates might otherwise impede clotting by preventing platelet adhesion and washing out activated coagulation factors. Thus, thrombus formation within cardiac chambers (e.g., after endocardial injury due to myocardial infarction), over ulcerated plaques in atherosclerotic arteries, or at sites of traumatic or inflammatory vascular injury (vasculitis) is largely a consequence of endothelial cell injury. Endothelial Injury Physical loss of endothelium can lead to exposure of the subendothelial ECM, adhesion of platelets, release of tissue factor, and local depletion of PGI2 and plasminogen activators. However, it should be emphasized that endothelium need not be denuded or physically disrupted to contribute to the development of thrombosis; any perturbation in the dynamic balance of the prothombotic and antithrombotic activities of endothelium can influence local clotting events. Thus, dysfunctional endothelial cells can produce more procoagulant factors (e.g., platelet adhesion molecules, tissue factor, PAIs) or may synthesize less anticoagulant effectors (e.g., thrombomodulin, PGI2, t-PA). Endothelial dysfunction can be induced by a wide variety of insults, including hypertension, turbulent blood flow, bacterial endotoxins, radiation injury, metabolic abnormalities such as hypercholesterolemia. Alterations in Normal Blood Flow Turbulence contributes to arterial and cardiac thrombosis by causing endothelial injury or dysfunction, as well as by forming countercurrents and local pockets of stasis; stasis is a major contributor in the development of venous thrombi. -

3. Thrombosis. Embolism. DIC. Shock
3. Thrombosis. Embolism. DIC. Shock. PATHOLOGY OF VASCULAR OCCLUSION: thrombosis, embolism, disseminated intravascular coagulation (DIC) Hemostasis (”stopping of hemorrhage”) Physiological process to maintain blood in a fluid, clot-free state in normal vessels, and to stop bleeding from ruptured vessels Main components of hemostasis: endothelium, platelets, and coagulation proteins Endothelial cells have both procoagulant and anticoagulant properties, and according to the needs of the body they may either promote clotting or inhibiting it Procoagulant functions Release of • von Willebrand factor (vWF); mediates the binding of platelets to endothelial surfaces • Tissue factor (TF); promotes the extrinsic pathway of the coagulation cascade • Inhibitors of plasminogen activator Anticoagulant functions • Inhibition of platelet aggregation via prostacyclin secretion • Dilation of blood vessels via nitric oxide secretion • Antithrombin activity, accomplished by thrombomodulin, which captures thrombin • Fibrinolysis, via secreting plasminogen activator, which generates plasmin from plasminogen Platelets Upon contact with TF and/or vWF, platelets become activated and 1) adhere to injured sites 2) release chemical mediators to induce further platelet aggregation, and activation of coagulation proteins 3) aggregate with other platelets and form the hemostatic plug. Both RBCs and leukocytes are also found in hemostatic plugs. Coagulation proteins Group of plasma proteins that are activated by acting upon each other in a sequence known as the extrinsic and intrinsic pathway. These proteins converge, and finally thrombin converts fibrinogen to fibrin within and about the platelet plug. THROMBOSIS • Intravascular clotting in a living person • Clots formed inside the blood vessels or cardiac chambers are called thrombi • Thrombi are always potential sources of further complications Factors promoting thrombus formation (Virchow’s triad) 1. -

A Whole Blood Thrombus Mimic: Constitutive Behavior Under Simple Shear a B a a a Gabriella P
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.19.210732; this version posted July 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. A Whole Blood Thrombus Mimic: Constitutive Behavior Under Simple Shear a b a a a Gabriella P. Sugerman , Sotirios Kakaletsis , Parin Thakkar , Armaan Chokshi , Sapun H. Parekh a,b,g < and Manuel K. Rausch , aUniversity of Texas at Austin, Department of Biomedical Engineering, 107 W Dean Keeton St, Austin, TX 78712 bUniversity of Texas at Austin, Department of Aerospace Engineering & Engineering Mechanics, 2617 Wichita St, Austin, TX 78712 gUniversity of Texas at Austin, Oden Institute for Computational Engineering and Sciences, 201 E 24th St, Austin, TX 78712 ARTICLEINFO ABSTRACT Keywords: Deep vein thrombosis and pulmonary embolism affect 300,000-600,000 patients each year in the US. venous thrombus The progression from deep vein thrombus to pulmonary embolism occurs when blood clots, as a hyperelasticity whole or partially, break off from the deep veins and eventually occlude the pulmonary arteries. Ve- large deformation nous thromboembolism is the cause of up to 100,000 deaths per year in the US alone. To date, we deep vein thrombosis don’t fully understand this mechanical process among other reasons because in-vivo samples are dif- pulmonary embolism ficult to obtain, highly heterogeneous, and their shapes are inappropriate for most mechanical tests. Toward overcoming these obstacles, we have set out to develop an in-vitro thrombus mimic and to test this mimic under large deformation simple shear. -

Mechanisms of Thrombosis
Mechanisms of Thrombosis Maureane Hoffman, MD, PhD Professor of Pathology Thrombosis • Formation of a blood clot in an artery or vein of a living person • Arterial thrombosis denies oxygen and nutrition to an area of the body – Thrombosis of an artery leading to the heart causes a myocardial infarction – Thrombosis of an artery leading to the brain causes a stroke • Acute arterial thrombosis often results from the deposition of atherosclerotic material in the wall of an artery, which gradually narrows the channel, precipitating clot formation Thrombosis • Extends into vessel without blocking it completely - mural thrombus • Blocks it completely - occlusive thrombus • Extends along the blood vessel - propagative thrombus Thrombosis • Venous thrombosis blocks return of deoxygenated blood to the heart • Venous thrombosis is quite common in the lower extremities, but can also occur in the upper extremeties • Symptoms include swelling, bluish discoloration and pain. • The most feared complication of venous thrombosis is pulmonary embolism Pulmonary Emboli Lines of Zahn in a pulmonary embolus Is it thrombus or post-mortem clot? • Thrombus adheres to the vessel wall • May be red, white, or mixed • Is crumbly and layered Small pulmonary emboli Thrombosis in the Aorta What Causes Thrombosis? Virchow’s Triad: Stasis Vascular Injury Hypercoagulability Vascular Injury endothelial cell TF TF VIIa Hypercoagulability The coagulant/anticoagulant proteins and the cells each play a role Evolution of the Paradigm Old: Hypercoagulable State = Systemic -
Aetiology of Deep Venous Thrombosis - Implications for Prophylaxis
6 Aetiology of Deep Venous Thrombosis - Implications for Prophylaxis Paul S. Agutter and P. Colm Malone Theoretical Medicine and Biology Group, United Kingdom 1. Introduction Clinical research on deep venous thrombosis (DVT) and thromboembolism (VTE) has focused in recent years on the contributions of potentiating factors, alone and in combination, to the risk of contracting these conditions. Many such ‘risk factors’ have been identified (Geerts et al., 2004) and are discussed elsewhere in this book. The National Institute for Clinical Excellence (NICE) in the United Kingdom has exploited this knowledge to make the prevention of DVT its main focus for 2011. In his keynote lecture introducing the policy and procedures adopted by NICE, Arya (2011) described the tools for evaluating risk in various patient groups and emphasised ‘anticoagulation’ in the design and implementation of evidence-based prophylactic measures. He claimed that the frequency of VTE in hospital patients should be reduced by 2/3 if the agreed protocols are followed. An achievement of that magnitude would be most welcome. Comparable views have been articulated elsewhere in Europe. Although NICE is distinctive in recommending assessment for thromboprophylaxis for all medical inpatients, the health services of other European Union countries offer broadly similar guidelines, especially for patients with acute medical conditions with expected durations of hospital stay longer than 3-4 days (Khoury et al., 2011). Similarly, in the USA, the Surgeon General issued a ‘Call to Action to Prevent Deep Venous Thrombosis and Pulmonary Embolism’ in 2008 (Sliwka & Fang, 2010), and the Joint Commission on Accreditation of Healthcare Organizations requires prophylaxis for patients at moderate or high risk of VTE (Rothberg et al., 2010). -
Namibia University of Science and Technology Faculty of Health and Applied Sciences
NAMIBIA UNIVERSITY OF SCIENCE AND TECHNOLOGY FACULTY OF HEALTH AND APPLIED SCIENCES DEPARTMENT OF HEALTH SCIENCES QUALIFICATION: BACHELOR OF HEALTH INFORMATION SYSTEMS MANAGEMENT QUALIFICATION CODE: 07BHIS LEVEL: 5 COURSE CODE: BPP5215S COURSE NAME: BASIC PATHOPHYSIOLOGY SESSION: JANUARY 2020 PAPER: THEORY DURATION: 3 HOURS MARKS: 100 SECOND OPPORTUNITY EXAMINATION QUESTION PAPER EXAMINER MR. JOMIN GEORGE MODERATOR: Ms. Elizabeth Van Der Colf INSTRUCTIONS Answer ALL the questions. Write clearly and neatly. Number the answers clearly. Write all answers in the answer booklet provided. PWNP PERMISSIBLE MATERIALS 1. NONE. THIS EXAMINATION QUESTION PAPER CONSISTS OF 7 PAGES (Including this front page) SECTION A [75 MARKS] QUESTION 1 [50 MARKS] 1. Evaluate the statements in each numbered section and select the most appropriate Answer or phrase from the given possibilities. Write the appropriate letter next to the number of the statement/phrase in the ANSWER BOOK. Each question carries 2 — marks 1.1 The drug of choice for stroke prevention is. A. Aspirin B. Ticlopidine C. Clopidogrel D. Warfarin 1.2 The following is not a symptom of Addison's Disease. A. Weight loss B. Bronzing of the skin C. Craving for salty foods D. Weight gain 1.3 The most sign which helps to identify COPD is. A. Pulmonary hypertension B. Cor pulmonale C. Impaired systemic muscle function D. Wheezing on auscultation 1.4 Another name for a stroke is. A. Heart attack B. Brain attack C. Myocardial infarction D. Brain Death 1.5 Type of hernia affects the oesophagus. A. Hiatus B. Gastric C. Inguinal D. Alimentary Nw 1.6 Virchow's triad refers to. -

Pulmonary Thrombo-Embolism: Difficulties Encoun- Tered in Establishing Causal Relationship and Exclud- Ing Therapeutic Mismanagement-A Case Report
Case Study International Journal of Research - GRANTHAALAYAH ISSN (Online): 2350-0530 April 2021 9(4), 150–160 ISSN (Print): 2394-3629 PULMONARY THROMBO-EMBOLISM: DIFFICULTIES ENCOUN- TERED IN ESTABLISHING CAUSAL RELATIONSHIP AND EXCLUD- ING THERAPEUTIC MISMANAGEMENT-A CASE REPORT 1 2 Sanjaya Hulathduwa and Bandula Wijesinghe 1Senior Lecturer, Department of Forensic Medicine, Faculty of Medical Sciences, University of Sri Jayawardenepure, Nuge- goda, Sri Lanka 2Senior Registrar in Forensic Medicine, Colombo South Teaching Hospital, Kalubowila, Sri Lanka ABSTRACT Pulmonary embolism designates blockage of pulmonary arteries by substances moved from elsewhere in the body through the circulation. The commonest form is thromboembolism. The presentation of pulmonary thromboembolism (PTE) is extremely variable from being completely asymptomatic to sudden car- diovascular collapse and death. Shortness of breath, chest pain and haemopty- sis are other common presentations. PTE is not a frequently encountered entity in routine autopsy practice. Out of all cases detected at autopsy, approximately ifty percent are not clinically diagnosed or even suspected, making it one of Received 27 March 2021 the top pathological entities clinically underdiagnosed or misdiagnosed. The Accepted 12 April 2021 autopsy, therefore remains the gold standard of post-mortem identiication of Published 30 April 2021 PTE. Autopsy also allows to establish or exclude a clinico-pathologic co-relation Corresponding Author between the clinical diagnosis and actual cause established -

In Vivo Noninvasive Detection and Age Definition of Arterial Thrombus By
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Journal of the American College of Cardiology Vol. 39, No. 8, 2002 © 2002 by the American College of Cardiology Foundation ISSN 0735-1097/02/$22.00 Published by Elsevier Science Inc. PII S0735-1097(02)01754-0 EXPERIMENTAL STUDIES In Vivo Noninvasive Detection and Age Definition of Arterial Thrombus by MRI Roberto Corti, MD,*† Julio I. Osende, MD,*† Zahi A. Fayad, PHD,†‡ John T. Fallon, MD, PHD, FACC,†§ Valentin Fuster, MD, PHD, FACC,† Gabor Mizsei, MS,†‡ Elisha Dickstein, BA,* Burton Drayer, MD,‡ Juan J. Badimon, PHD, FACC*† New York, New York OBJECTIVES The purpose of this study was to evaluate the potential of magnetic resonance (MR) to detect arterial thrombotic obstruction and define thrombus age. BACKGROUND Arterial thrombi underlie the clinical consequences of atherosclerosis and are not reliably detected by current noninvasive diagnostic techniques. METHODS Carotid thrombi were induced in swine (n ϭ 7) by arterial injury. Serial high-resolution in vivo MR images were obtained using black-blood T1-weighted (T1W) and T2-weighted (T2W) sequences in a clinical 1.5T MR system at 6 h, 1 day and at 1, 2, 3, 6 and 9 weeks. At each time point one animal was sacrificed and the occluded carotid artery processed for histopathology. Thrombus signal intensity (SI) was normalized to that of the adjacent muscle. Thrombus age was assessed based on MR appearance by two blinded independent observers. RESULTS Thrombus appearance and relative SI revealed characteristic temporal changes in multicontrast-weighted MR images, reflecting histologic changes in the composition. -

THROMBOSIS by Geoffrey Hadfield, M.D., F.R.C.P
THROMBOSIS by Geoffrey Hadfield, M.D., F.R.C.P. Sir William Collins Professor of Human and Comparative Pathology, Royal College of Surgeons of England THE CARDIOVASCULAR STREAM-BED has two arresting physical properties. The endothelial membrane which lines it possesses a high degree of smoothness which must very materially diminish the frictional resistance between the walls of the vessels and their contained blood. Equally obvious, but less frequently commented upon, is the exquisitely stream- lined construction of the complex pathway traversed by the flowing blood. This is planned to reduce obstruction to a minimum and to eliminate swirling, eddying, back-water formation and local stagnation. Any obstruction to the forward flow, especially in vessels in which the normal local velocity is low, carries the risk of stasis and, as blood in vivo clots when it ceases to move, we may take it that the preservation of the physical properties of the cardiovascular pathway is a natural safeguard against intravascular coagulation. It is abundantly clear that the smooth- ness and stream-lining of the vascular bed is frequently threatened in many different ways and it is most probable that some rapidly acting mechanism has been evolved to preserve its physical integrity. Fig. 1 illustrates some of the more simple conditions which, by producing physical abnormalities in the vascular walls, predispose to local stasis. Amongst these are external pressure producing internal bulging; local narrowing of a vessel from spasm, inflammation or degeneration; patho- logical dilatation ofa cardiac chamber or ofa blood vessel expanded into an aneurysmal sac; puckering, folding or corrugation from surrounding cicatrisation; valvular sclerosis and rigidity. -

Forensic Lung Pathology
31 Forensic Lung Pathology Michael A. Graham Sudden and unexpected natural deaths and nonnatural The cause of death is the disease or injury that begins deaths may result from various pulmonary conditions. the unbroken pathophysiologic sequence leading to Additionally, several nonpulmonary conditions of foren death. The disease/injury that causes death at a particular sic significance may be complicated by the development time is often referred to as the immediate cause of death. of respiratory lesions. Certain situations with pulmonary The disease/injury that starts the unbroken chain of pathology are particularly likely to be critically scruti medical events culminating in death is referred to as the nized and may form the basis of allegations of medical underlying cause of death. Proper recognition of the latter negligence, other personal injury liability, or wrongful is very important for death certification, epidemiology, death.l public policy, and the proper resolution of criminal justice The forensic evaluation of lethal or nonlethal conditions and civil liability issues. 2 The mechanism of death is the is essentially the same and conceptually differs little from nonspecific pathophysiologic alteration through which a clinician's approach to a patient with a similar condition the cause of death exerts its lethal influence. The manner (Table 31.1). In some cases this diagnostic/investigative of death is a term peculiar to death certification that process is quite broad, whereas in other cases the issues describes how death came about-through natural causes, are of very limited scope and the investigation may be homicide, suicide, or accident.2 The determination of the narrowly focused. -
Thrombosis and Emboli Peter Nagy • a Thrombus Is Any Solid Object Developing from the Blood in Vivo Within the Vascular System Or Heart
Thrombosis and emboli Peter Nagy • A thrombus is any solid object developing from the blood in vivo within the vascular system or heart. • Thrombosis is hemostasis in the wrong place. • Major components, forms: platelet aggregates platelet/white thrombus clotted blood red thrombus fibrin fibrin thrombus Pathogenesis of thrombosis (Virchow’s triad) • Changes in the vascular wall (endothelial damage) • Changes in flow (slow or turbulent flow) • Changes in the blood (hypercoagulability) Thrombosis may occur even if the triad is not complete, just two of the conditions suffice. Changes in the vascular wall • Atherosclerotic plaques • Inflamed tissues, immunological reactions • Necrotic tissues • Surgical interventions • Special conditions (TTP) Changes in flow • Sluggish flow (veins, bedridden patients, pregnancy) • Turbulent flow Changes in blood • Acquired changes (cancer, pregnancy, antiphospholipid syndrome) • Inherited conditions (Leiden mutation etc.) Steps of thrombus formation • Platelet aggregation, activation • Fibrin formation with entrapped red blood cells • Platelet aggregation Lines of Zahn The clotting stops at the level of the nearest branch, where flow dilutes the clotting factors. Fates of a thrombus • Dissolves • Propagation • Breakes off and forms embolus • Organizes • Recanalization • Calcification (phlebolith) Types of thrombus • Arterial thrombi ( white thrombi, mostly platelet aggregation) • Venous thrombi (red thrombi, coagulation) • Vegetations (thrombus on a cardiac valve) • Infected thrombi (spreading of infection) • Migrating thrombophlebitis (paraneoplasia) • Tumor thrombus • Fibrin thrombi (DIC) Disseminated intravascular coagulation (DIC) (haemorrhagic microthrombosis) • Acut (Gram negative sepsis, trauma, complications of birth, snake bite • Chronic (Paraneoplasia) • 1.Generalized activation of the clotting cascade • 2. Fibrinolysis • Consumptive coagulopathy Conseqences of DIC • I. Microvascular thrombosis (multifocal brain necroses, coma; superficial ulceration, gangrene of skin, mucous membranes; oliguria; ARDS) • II.