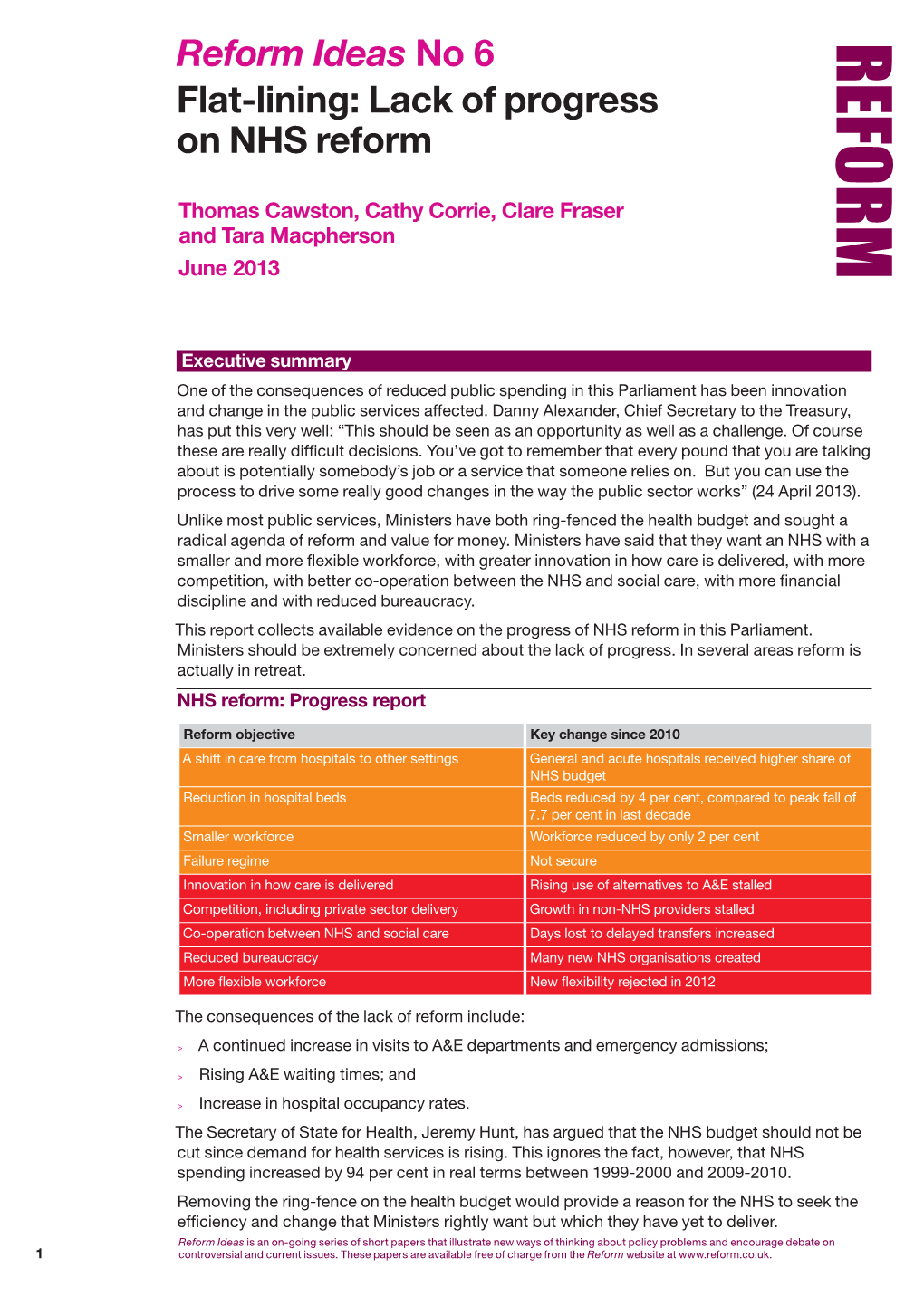
Reform Ideas No 6 Flat-Lining: Lack of Progress on NHS Reform
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

South Warwickshire NHS Foundation Trust Annual Report and Accounts
South Warwickshire NHS Foundation Trust Annual Report and Accounts for 2014/15 South Warwickshire NHS Foundation Trust Annual Report and Accounts for 2014/15 Presented to Parliament pursuant to Schedule 7, paragraph 25 (4) (a) of the National Health Service Act 2006 2 Content Introduction: pages 3-5 Section 2: Directors’ Report pages 69-90 Chief Executive’s message Chairman’s message - Directors’ Statement - Appointments and Roles Section 1: Strategic Report pages 6-68 - Board Profiles and Register of Interest - About the Trust - Executive Leadership Structure - Trust Structure - Disclosure of Corporate Governance Arrangements - Service Profile / Principal - Board Statements Activities - Board Committees - Strategy - Board and Committee - 2014/15 objectives Membership - Business Review - Directors’ Remuneration and Review of 2014/15 Pension Benefits objectives Trust performance Section 3: Council of Governors and against national Membership pages 91-112 targets Quality - Council of Governors Structure - Governor Profiles Key Developments in - Map of Constituencies 2013/14 - Meetings of the Council of Financial Performance Governors Review - Sub-committees of the Council of - Risks and Uncertainties Governors - Trends and Factors affecting the - Trust Membership Trust - Partnerships, Stakeholders and Section 4: Quality Report pages 113- Key Strategic Relationships 218 - Corporate Activity Data Part 1: Statement on Quality Part 2: Priorities for Improvement and Serious Untoward Assurance Statements Incidents Part 3: Review of Quality Performance Information Governance Section 5: Statement of Accounting Patient Experience Officers’ Responsibilities and Annual Workforce Governance Statement pages 219- Social, Community and 233 Human Rights Current Developments Section 6: Summary of Financial Environmental and Statements & Auditor’s Statement Sustainability pages 234-242 3 Chief Executive’s Message The end of another financial year provides an opportunity to reflect and to re- focus. -
Health Care Systems in the Eu a Comparative Study
EUROPEAN PARLIAMENT DIRECTORATE GENERAL FOR RESEARCH WORKING PAPER HEALTH CARE SYSTEMS IN THE EU A COMPARATIVE STUDY Public Health and Consumer Protection Series SACO 101 EN This publication is available in the following languages: EN (original) DE FR The opinions expressed in this document are the sole responsibility of the author and do not necessarily represent the official position of the European Parliament. Reproduction and translation for non-commercial purposes are authorized, provided the source is acknowledged and the publisher is given prior notice and sent a copy. Publisher: EUROPEAN PARLIAMENT L-2929 LUXEMBOURG Author: Dr.med. Elke Jakubowski, MSc. HPPF, Advisor in Public Health Policy Department of Epidemiology and Social Medicine, Medical School Hannover Co-author: Dr.med. Reinhard Busse, M.P.H., Department of Epidemiology and Social Medicine, Medical School Hannover Editor: Graham R. Chambers BA Directorate-General for Research Division for Policies on Social Affairs, Women, Health and Culture Tel.: (00 352) 4300-23957 Fax: (00 352) 4300-27720 e-mail: [email protected] WITH SPECIAL GRATITUDE TO: James Kahan, Panos Kanavos, Julio Bastida-Lopez, Elias Mossialos, Miriam Wiley, Franco Sassi, Tore Schersten, Juha Teperi for their helpful comments and reviews of earlier drafts of the country chapters, and Manfred Huber for additional explanatory remarks on OECD Health Data. The manuscript was completed in May 1998. EUROPEAN PARLIAMENT DIRECTORATE GENERAL FOR RESEARCH WORKING PAPER HEALTH CARE SYSTEMS IN THE EU A COMPARATIVE STUDY Public Health and Consumer Protection Series SACO 101 EN 11-1998 Health Care Systems CONTENTS INTRODUCTION ........................................................... 5 PART ONE: A Comparative Outline of the Health Care Systems of the EU Member States ........................................ -
Full-Text Provided on Manchester Research Explorer Is the Author Accepted Manuscript Or Proof Version This May Differ from the Final Published Version
The University of Manchester Research Moving Services out of hospital: Joining up General Practice and community services? Link to publication record in Manchester Research Explorer Citation for published version (APA): Bramwell, D., Checkland, K., Allen, P., & Peckham, S. (2014). Moving Services out of hospital: Joining up General Practice and community services? Policy Research Unit in Commissioning and the Healthcare System Manchester Centre for Health Economics. Citing this paper Please note that where the full-text provided on Manchester Research Explorer is the Author Accepted Manuscript or Proof version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version. General rights Copyright and moral rights for the publications made accessible in the Research Explorer are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Takedown policy If you believe that this document breaches copyright please refer to the University of Manchester’s Takedown Procedures [http://man.ac.uk/04Y6Bo] or contact [email protected] providing relevant details, so we can investigate your claim. Download date:04. Oct. 2021 Moving Services out of hospital: Joining up General Practice and community services? August 2014 Research Team: Dr Donna Bramwell1 Dr Kath Checkland1 Dr Pauline Allen2 Professor Stephen Peckham3 Disclaimer: This research is funded by the Department of Health via the Policy Research Programme. The views expressed are those of the researchers and not necessarily those of the Department of Health. -

31 DECEMBER 2013 GIFTS GIVEN OVER £140 the Rt Hon
HM TREASURY MINISTERS QUARTERLY INFORMATION: 1 OCTOBER – 31 DECEMBER 2013 GIFTS GIVEN OVER £140 The Rt Hon George Osborne MP, Chancellor of the Exchequer Date gift given To Gift Value (over £140) Nil return The Rt Hon Danny Alexander MP, Chief Secretary to the Treasury Date gift given To Gift Value (over £140) Nil return Greg Clark MP, Financial Secretary (1 October – 6 October 2013) Date gift given To Gift Value (over £140) Nil return Sajid Javid MP, Financial Secretary (7 October 2013 – Present) Date gift given To Gift Value (over £140) Nil return David Gauke MP, Exchequer Secretary Date gift given To Gift Value (over £140) Nil return Sajid Javid MP, Economic Secretary (1 October - 6 October 2013) Date gift given To Gift Value (over £140) Nil return Nicky Morgan MP, Economic Secretary (7 October 2013 – Present) Date gift given To Gift Value (over £140) Nil return Lord Deighton, Commercial Secretary Date gift given To Gift Value (over £140) Nil return 1 GIFTS RECEIVED OVER £140 The Rt Hon George Osborne MP, Chancellor of the Exchequer Date gift From Gift Value Outcome received 16 October Huawei Mobile Over the Held by the 2013 telephone limit Department The Rt Hon Danny Alexander MP, Chief Secretary to the Treasury Date gift From Gift Value Outcome received Nil return Greg Clark MP, Financial Secretary (1 October – 6 October 2013) Date gift From Gift Value Outcome received Nil return Sajid Javid MP, Financial Secretary (7 October 2013 - Present) Date gift From Gift Value Outcome received Nil return David Gauke MP, Exchequer Secretary -

Parliamentary Debates (Hansard)
Tuesday Volume 563 14 May 2013 No. 5 HOUSE OF COMMONS OFFICIAL REPORT PARLIAMENTARY DEBATES (HANSARD) Tuesday 14 May 2013 £5·00 © Parliamentary Copyright House of Commons 2013 This publication may be reproduced under the terms of the Open Parliament licence, which is published at www.parliament.uk/site-information/copyright/. 477 14 MAY 2013 478 and in the Budget we announced the Help to Buy House of Commons scheme, a major new package to increase the supply of low-deposit mortgages for creditworthy households, which Tuesday 14 May 2013 I hope the hon. Lady will welcome. Ann McKechin: In evidence to the Treasury Select The House met at half-past Eleven o’clock Committee, the distinguished commentator, Martin Wolf, described the Government’s mortgage indemnity guarantee PRAYERS as “good politics and horrendous economics.” Why are the Government pursuing a policy that is likely [MR SPEAKER in the Chair] to increase the price of already over-inflated property, Mr Speaker: Order. I draw Members’ attention to the rather than financing affordable social housing that is fact that the book for entering the private Member’s Bill needed by hundreds of thousands of people across the ballot is now open for Members to sign in the No country? Lobby. It will be open until the House rises today and when the House is sitting on Wednesday 15 May. The Danny Alexander: The hon. Lady comments on ballot will be drawn on Thursday 16 May, and a note affordable social housing, but I note that during Labour’s setting out those arrangements, and the dates when 13 years in office the amount of social housing fell by ten-minute rule motions can be made and presentation 421,000. -

Inverness, Nairn, Badenoch & Strathspey
. BURN’S SUPPER REMINDER Inverness, Nairn, Badenoch & Strathspey January Have you booked you tickets yet? 2014 Secretary of State for Scotland Alistair Carmichael MP for Orkney and NEWSLETTER Edited by John Melling Shetland will be our guest of honour. The supper will be a traditional Burns Night event, attended by members and supporters from across the Highlands. There will be the raffle on the night, for which donation would be welcome. HIGHLAND CAMPAIGNER TO STAND For tickets or further information, please do not hesitate to contact the office on IN SKYE, LOCHABER & BADENOCH FOR 01463 711280. SCOTTISH PARLIAMENT ELECTIONS Highland Liberal Democrats have Friday 7th February 2014, 7.30pm-11pm welcomed Cllr Kate Stephen as their prospective candidate for Skye, Lochaber & Badenoch for the Scottish Parliamentary Highland Liberal Democrats election in 2016. Burns Supper As a local councillor, Mrs Stephen has a long record of serving the people of the Palace Hotel, Ness Walk, Inverness Robert Burns Highlands. She spent several years 1759-1796 working for the UHI Centre for Rural Health, £25 per person. leading an award-winning project tackling issues affecting older people in rural areas. GOODBYE TO KAREN FRASER Danny said: “Kate will be a fantastic MSP for the Highlands. I know that This January we say good bye to Karen after 5 years working for the party, latterly Kate will work for our area, and bring the focus of the Scottish as Head of Office for Danny Alexander MP. A graduate of Aberdeen University, Government back to the issues that matter most, like creating jobs, Karen first volunteered with the Liberal Democrats in the Gordon Constituency building homes and investing in our infrastructure locally.” Office. -

Health Care Facilities Hospitals Report on Training Visit
SLOVAK UNIVERSITY OF TECHNOLOGY IN BRATISLAVA FACULTY OF ARCHITECTURE INSTITUTE OF HOUSING AND CIVIC STRUCTURES HEALTH CARE FACILITIES HOSPITALS REPORT ON TRAINING VISIT In the frame work of the project No. SAMRS 2010/12/10 “Development of human resource capacity of Kabul polytechnic university” Funded by UÜtà|áÄtät ECDC cÜÉA Wtâw f{t{ YtÜâÖ December, 14, 2010 Prof. Daud Shah Faruq Health Care Facilities, Hospitals 2010/12/14 Acknowledgement: I Daud Shah Faruq professor of Kabul Poly Technic University The author of this article would like to express my appreciation for the Scientific Training Program to the Faculty of Architecture of the Slovak University of Technology and Slovak Aid program for financial support of this project. I would like to say my hearth thanks to Professor Arch. Mrs. Veronika Katradyova PhD, and professor Arch. Mr. stanislav majcher for their guidance and assistance during the all time of my training visit. My thank belongs also to Ing. Juma Haydary, PhD. the coordinator of the project SMARS/2010/10/01 in the frame work of which my visit was realized. Besides of this I would like to appreciate all professors and personnel of the faculty of Architecture for their good behaves and hospitality. Best regards cÜÉyA Wtâw ft{t{ YtÜâÖ December, 14, 2010 2 Prof. Daud Shah Faruq Health Care Facilities, Hospitals 2010/12/14 VISITING REPORT FROM FACULTY OF ARCHITECTURE OF SLOVAK UNIVERSITY OF TECHNOLOGY IN BRATISLAVA This visit was organized for exchanging knowledge views and advices between us (professor of Kabul Poly Technic University and professors of this faculty). My visit was especially organized to the departments of Public Buildings and Interior design. -

Annual Report 2010
nd 22 Annual Conference Annual Report 2010 The major challenge since the 21st Annual Conference in December 2009 has been the national DHB MECA negotiations. Other challenges include promoting clinical leadership and engagement in DHBs consistent with the Time for Quality agreement and the In Good Hands policy statement, and the Government’s proposed amendments to the Employment Relations Act. The members of the National Executive are: President Jeff Brown (MidCentral) Vice President David Jones (Capital & Coast) Region 1 Judy Bent (Auckland) Himadri Seth (Waitemata) Region 2 John Bonning (Waikato) Paul Wilson (Bay of Plenty) Region 3 Hein Stander (Tairawhiti) - since June following the resignation of Torben Iversen in May Tim Frendin (Hawke’s Bay) Region 4 Brian Craig (Canterbury) John MacDonald (Canterbury) In May Torben Iversen resigned to take up a specialist position in Victoria (although still working one week every four in Tairawhiti). While technically eligible to continue on the National Executive practical considerations meant that he chose to resign. The Association is appreciative of the important contribution Dr Iversen made while on the Executive including bringing to the fore the position of members in smaller provincial DHBs, and for his role as Association representative in Tairawhiti. In June Hein Stander was elected unopposed in a by-election. The National Executive has met on four occasions in Wellington since the last Annual Conference, with a fifth meeting to be held immediately preceding this Conference. On 17-18 February the National Executive held its annual two day meeting to discuss strategic directions, the first day being informal. The informal day included: • Preparing for the national DHB MECA negotiations, including strategic direction and the draft claim. -

NHS Foundation Trusts 29 APRIL 2003 in the Health and Social Care (Community Health and Standards) Bill Bill 70 of 2002-3
RESEARCH PAPER 03/38 NHS Foundation Trusts 29 APRIL 2003 in the Health and Social Care (Community Health and Standards) Bill Bill 70 of 2002-3 Part I of the Bill makes provision for a new type of NHS organisation in England, to be known as an NHS Foundation Trust. The Bill provides for these bodies to be regulated by a new non-ministerial department, to be called the Independent Regulator for NHS Foundation Trusts, and to have a new sort of constitution that would include a directly elected board of governors. Other Parts of the Bill will be covered in separate Library publications. Jo Roll SOCIAL POLICY SECTION HOUSE OF COMMONS LIBRARY Recent Library Research Papers include: 03/21 The Northern Ireland Assembly Elections Bill [Bill 74 of 2002-03] 13.03.03 03/22 Iraq: developments since UN Security Council Resolution 1441 13.03.03 03/23 The Convention on the Future of Europe: proposals for a 18.03.03 European Constitution 03/24 The Female Genital Mutilation Bill [Bill 21 of 2002-03] 19.03.03 03/25 The Waste and Emissions Trading Bill [Bill 66 of 2002-03] 19.03.03 03/26 Unemployment by Constituency, February 2003-03-20 19.03.03 03/27 The Licensing Bill [HL] [Bill 73 of 2002-03] 20.03.03 03/28 Ballistic Missile Defence 26.03.03 03/29 The Sustainable Energy Bill [Bill 20 of 2002-03] 26.03.03 03/30 The Crime (International Cooperation) Bill [HL] 28.03.03 [Bill 78 of 2002-03] 03/31 The Crime (International Cooperation) Bill [HL]: 'Hot Surveillance' 28.03.03 [Bill 78 of 2002-03] 03/32 Parliamentary Questions, Debate Contributions and Participation -

NHS Vale of York Clinical Commissioning Group Financial Performance Report
NHS Vale of York Clinical Commissioning Group Financial Performance Report Report produced: January 2016 Financial Period: April - December 2015 Summary of Key Financial Measures Year to Date Forecast Outturn Target Actual Variance RAG Target Actual Variance RAG Indicator £000 £000 £000 rating £000 £000 £000 rating Achieve planned surplus 2,959 132 -2,826 A 3,945 -7,351 -11,296 R Programme expenditure does not exceed 329,983 330,428 -445 R 429,695 437,956 -8,261 R programme allocation Running costs expenditure does not exceed running 5,701 5,124 577 G 7,602 6,692 910 G costs allocation Risk adjusted surplus 3,945 -7,351 -11,296 R QIPP delivery (see section 5) Better Payment Practice Code (Value) 95.00% 99.58% 4.58% G 95.00% >95% 0.00% G Better Payment Practice Code (Number) 95.00% 97.19% 2.19% G 95.00% >95% 0.00% G Cash balance at month end is within 1.5% of monthly 464 16 448 G drawdown CCG cash drawdown does not exceed maximum 437,321 437,321 0 G cash drawdown Note – The first 3 metrics correspond to those reported in Note 42 of the Annual Accounts, and represent the statutory duties of the CCG. The full finance dashboard is presented in Appendix 1 Key Messages - The CCG is currently classed as an organisation in turnaround due to the deteriorating financial position. - The CCG is forecasting a year end deficit of £7.35m, which is £11.30m below plan. This position includes several significant variances which are detailed in section 3. -

Board of Directors - Open
Board of Directors - Open Date: 12 August 2020 Item Ref: 05 TITLE OF PAPER Chief Executive’s Report TO BE PRESENTED BY Jan Ditheridge ACTION REQUIRED The Board are asked to consider the impact and opportunity of the letter from Sir Simon Stevens and Amanda Pritchard regarding the third phase of the NHS response to CoVid on our strategic priorities and risks. The Board are asked to approve the recommendation re Executive lead for Inequalities. The Board are asked if there are any other issues that arise from the letter from Sir Simon Stevens and Amanda Pritchard we should consider. The Board are asked to consider the National Guardian Freedom to Speak Up Index Report 2020 and if they feel confident where and how we are addressing the issues it raises for us. The Board are asked to consider the NHS People Plan 2020/21, and where we may want the People Committee to focus attentions as an organisation, given our risks and challenges and as a contributor to our health and care system. The Board are asked to consider the direction of travel of the Accountable Care Partnership; and to understand the key priorities and how they relate to our own transformation programme. The Board are asked to acknowledge the Board role changes, consider any opportunities or risks within the changes and join me in thanking individuals for their contributions and wish them well where they have changed or moved into different roles. OUTCOME To update the Board on key policies, issues and events and to stimulate debate regarding potential impact on our strategy and levels of assurance. -

The Middlesex Hospital Orthopaedic Department 1920 – 2005 the 85
The Middlesex Hospital Orthopaedic Department 1920 – 2005 The 85 years 1 Contents 1. Charles Bell (1774-1842) The Middlesex Hospital Sean Hughes Medical School 2. A Brief Overview of The Middlesex Hospital 1745 – Michael Edgar 2005 3. Blundell Bankart (1879 –1951) Roger Emery 4. Phillip Wiles (1899 – 1967) A. Total Hip Replacement James Scott B. Contribution to Scoliosis Surgery Michael Edgar 5. Phillip Newman (1912 – 1994) A. Sir Winston Churchill’s Hip Fracture: Liam Mcloughlin The Middlesex Hospital June 1962 B. Spinal Surgery Michael Edgar 6. Rodney Sweetnam (1927 – 2013) Michael Benson 7. Nursing in The Middlesex Orthopaedic Department Fiona Hamblin 8. The Athletes’ Clinic Fares Haddad Michael Edgar Reflections on being a Registrar in the Patrick Boland Athletes’ Clinic 9. The Last Fifteen years of The Middlesex Orthopaedic Department 1991 – 1996 Michael Edgar 1995 – 2005 Justin Cobb 10. The Middlesex in Africa Chris Lavy 11. The Contributions of The Middlesex Orthopaedic Steve Cannon Department to the National and International Scene 2 The Middlesex Hospital 2000, (taken after a fire drill). 3 Chapter 1 Sir Charles Bell (1774 – 1842) and The Middlesex Hospital Medical School Sean Hughes Charles Bell (1774 – 1842), a surgeon and anatomist, was also an artist and philosopher. He was born in Fountainbridge, an area of Edinburgh, the youngest of four sons of the Reverend William Bell (1704 –1779), who died when Charles was five years old. His mother, Margaret Morris, was William Bell’s second wife and was the elder daughter of an Episcopalian clergyman in St Andrews, a seaside town north-east of Edinburgh. Her father was the head of the Episcopalian Church of Scotland, the Primus, in his time, reflecting the strong religious upbringing in Charles’s early development.