NHS Vale of York Clinical Commissioning Group Financial Performance Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

South Warwickshire NHS Foundation Trust Annual Report and Accounts
South Warwickshire NHS Foundation Trust Annual Report and Accounts for 2014/15 South Warwickshire NHS Foundation Trust Annual Report and Accounts for 2014/15 Presented to Parliament pursuant to Schedule 7, paragraph 25 (4) (a) of the National Health Service Act 2006 2 Content Introduction: pages 3-5 Section 2: Directors’ Report pages 69-90 Chief Executive’s message Chairman’s message - Directors’ Statement - Appointments and Roles Section 1: Strategic Report pages 6-68 - Board Profiles and Register of Interest - About the Trust - Executive Leadership Structure - Trust Structure - Disclosure of Corporate Governance Arrangements - Service Profile / Principal - Board Statements Activities - Board Committees - Strategy - Board and Committee - 2014/15 objectives Membership - Business Review - Directors’ Remuneration and Review of 2014/15 Pension Benefits objectives Trust performance Section 3: Council of Governors and against national Membership pages 91-112 targets Quality - Council of Governors Structure - Governor Profiles Key Developments in - Map of Constituencies 2013/14 - Meetings of the Council of Financial Performance Governors Review - Sub-committees of the Council of - Risks and Uncertainties Governors - Trends and Factors affecting the - Trust Membership Trust - Partnerships, Stakeholders and Section 4: Quality Report pages 113- Key Strategic Relationships 218 - Corporate Activity Data Part 1: Statement on Quality Part 2: Priorities for Improvement and Serious Untoward Assurance Statements Incidents Part 3: Review of Quality Performance Information Governance Section 5: Statement of Accounting Patient Experience Officers’ Responsibilities and Annual Workforce Governance Statement pages 219- Social, Community and 233 Human Rights Current Developments Section 6: Summary of Financial Environmental and Statements & Auditor’s Statement Sustainability pages 234-242 3 Chief Executive’s Message The end of another financial year provides an opportunity to reflect and to re- focus. -

NHS Foundation Trusts 29 APRIL 2003 in the Health and Social Care (Community Health and Standards) Bill Bill 70 of 2002-3
RESEARCH PAPER 03/38 NHS Foundation Trusts 29 APRIL 2003 in the Health and Social Care (Community Health and Standards) Bill Bill 70 of 2002-3 Part I of the Bill makes provision for a new type of NHS organisation in England, to be known as an NHS Foundation Trust. The Bill provides for these bodies to be regulated by a new non-ministerial department, to be called the Independent Regulator for NHS Foundation Trusts, and to have a new sort of constitution that would include a directly elected board of governors. Other Parts of the Bill will be covered in separate Library publications. Jo Roll SOCIAL POLICY SECTION HOUSE OF COMMONS LIBRARY Recent Library Research Papers include: 03/21 The Northern Ireland Assembly Elections Bill [Bill 74 of 2002-03] 13.03.03 03/22 Iraq: developments since UN Security Council Resolution 1441 13.03.03 03/23 The Convention on the Future of Europe: proposals for a 18.03.03 European Constitution 03/24 The Female Genital Mutilation Bill [Bill 21 of 2002-03] 19.03.03 03/25 The Waste and Emissions Trading Bill [Bill 66 of 2002-03] 19.03.03 03/26 Unemployment by Constituency, February 2003-03-20 19.03.03 03/27 The Licensing Bill [HL] [Bill 73 of 2002-03] 20.03.03 03/28 Ballistic Missile Defence 26.03.03 03/29 The Sustainable Energy Bill [Bill 20 of 2002-03] 26.03.03 03/30 The Crime (International Cooperation) Bill [HL] 28.03.03 [Bill 78 of 2002-03] 03/31 The Crime (International Cooperation) Bill [HL]: 'Hot Surveillance' 28.03.03 [Bill 78 of 2002-03] 03/32 Parliamentary Questions, Debate Contributions and Participation -

Board of Directors - Open
Board of Directors - Open Date: 12 August 2020 Item Ref: 05 TITLE OF PAPER Chief Executive’s Report TO BE PRESENTED BY Jan Ditheridge ACTION REQUIRED The Board are asked to consider the impact and opportunity of the letter from Sir Simon Stevens and Amanda Pritchard regarding the third phase of the NHS response to CoVid on our strategic priorities and risks. The Board are asked to approve the recommendation re Executive lead for Inequalities. The Board are asked if there are any other issues that arise from the letter from Sir Simon Stevens and Amanda Pritchard we should consider. The Board are asked to consider the National Guardian Freedom to Speak Up Index Report 2020 and if they feel confident where and how we are addressing the issues it raises for us. The Board are asked to consider the NHS People Plan 2020/21, and where we may want the People Committee to focus attentions as an organisation, given our risks and challenges and as a contributor to our health and care system. The Board are asked to consider the direction of travel of the Accountable Care Partnership; and to understand the key priorities and how they relate to our own transformation programme. The Board are asked to acknowledge the Board role changes, consider any opportunities or risks within the changes and join me in thanking individuals for their contributions and wish them well where they have changed or moved into different roles. OUTCOME To update the Board on key policies, issues and events and to stimulate debate regarding potential impact on our strategy and levels of assurance. -

Clinical Commissioning Group Governing Body Members: Role Outlines, Attributes and Skills
Clinical commissioning group governing body members: Role outlines, attributes and skills October 2012 Clinical commissioning group governing body members: Roles outlines, attributes and skills First published by the NHS Commissioning Board Authority: July 2012 Published by the NHS Commissioning Board: October 2012 This supersedes the version published in July 2012 This version incorporates The National Health Service (Clinical Commissioning Groups) Regulations 2012 S.I. 2012/16311. 1 http://www.legislation.gov.uk/uksi/2012/1631/contents/made 2 [Page left intentionally blank] 3 Contents 1. Introduction .............................................................................................................. 5 2. Core role outline – for all governing body members ................................................. 7 3. Additional information for each specified member.................................................. 10 GP or other healthcare professionals acting on behalf of member practices ............. 12 Chair of the governing body ....................................................................................... 13 Lay member on the governing body – with a lead role in overseeing key elements of financial management and audit ................................................................................ 15 Lay member on the governing body – with a lead role in championing patient and public involvement ..................................................................................................... 17 Clinical member on -

Oversight of NHS-Controlled Providers: Guidance February 2018
Oversight of NHS-controlled providers: guidance February 2018 We support providers to give patients safe, high quality, compassionate care within local health systems that are financially sustainable. Contents 1. Summary ................................................................................... 2 2. Our oversight of NHS-controlled providers ................................ 3 Annex A: NHS-controlled provider licence conditions .................... 7 1 | > Contents 1. Summary The NHS provider licence is a key part of NHS Improvement’s regulatory and oversight system (in this document, references to NHS Improvement are to Monitor and the NHS Trust Development Authority, TDA). Following the Health and Social Care Act 2012 (the Act), Monitor consulted on the first set of provider licence conditions for NHS foundation trusts and independent providers in 2013 and started issuing licences to foundation trusts in April 2013. Independent providers have been required to hold a licence since April 2014. Although NHS trusts are not legally required to hold a licence, in practice NHS Improvement applies the key conditions of the licence to NHS trusts, in line with the principles of the Single Oversight Framework (SOF) for NHS trusts and foundation trusts (collectively referred to as NHS providers). Following consultation between 13 September and 12 October 2017, we are extending our oversight of NHS-controlled providers, as outlined in section 2. 2 | > Oversight of NHS-controlled providers: our policy position 2. Our oversight of NHS- controlled providers 2.1 Why oversee NHS-controlled providers? NHS foundation trusts’ principal purpose is to provide goods and services for the purposes of the NHS in England. They are not-for-profit, public benefit corporations created to devolve decision-making from central government to local organisations and communities. -

UNDERSTANDING the NEW NHS a Guide for Everyone Working and Training Within the NHS 2 Contents 3
England UNDERSTANDING THE NEW NHS A guide for everyone working and training within the NHS 2 Contents 3 NHS ENGLAND INFORMATION READER BOX Introduction 4 Directorate ◆ The NHS belongs to us all Medical Operations Patients and information Nursing Policy Commissioning development Foreword (Sir Bruce Keogh) 5 Finance Human resources NHS values 6 Publications Gateway Reference: 01486 ◆ NHS values and the NHS Constitution Document purpose Resources ◆ An overview of the Health and Social Care Act 2012 Document name Understanding The New NHS Structure of the NHS in England 8 Author NHS England ◆ The structure of the NHS in England Publication date 26 June 2014 ◆ Finance in the NHS: your questions answered Target audience Running the NHS 12 ◆ Commissioning in the NHS Additional circulation Clinicians working and training within the NHS, allied ◆ Delivering NHS services list health professionals, GPs ◆ Health and wellbeing in the NHS Description An updated guide on the structure and function of Monitoring the NHS 17 the NHS, taking into account the changes of the Health and Social Care Act 2012 ◆ Lessons learned and taking responsibility ◆ Regulation and monitoring in the NHS Action required None Contact details for Dr Felicity Taylor Working in the NHS 20 further information National Medical Director's Clinical ◆ Better training, better care Fellow, Medical Directorate Skipton House NHS leadership 21 80 London Road SE1 6LH ◆ Leading healthcare excellence www.england.nhs.uk/nhsguide/ Quality and innovation in the NHS 22 ◆ High-quality care for all Document status This is a controlled document. While this document may be printed, the The NHS in the United Kingdom 24 electronic version posted on the intranet is the controlled copy. -
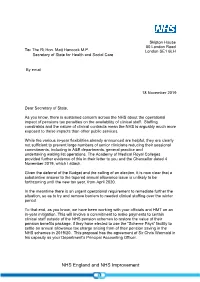
Letter from Simon Stevens to Matt Hancock on 18 November 2019
Skipton House 80 London Road To: The Rt Hon. Matt Hancock M.P. London SE1 6LH Secretary of State for Health and Social Care By email 18 November 2019 Dear Secretary of State, As you know, there is sustained concern across the NHS about the operational impact of pensions tax penalties on the availability of clinical staff. Staffing constraints and the nature of clinical contracts mean the NHS is arguably much more exposed to these impacts than other public services. While the various in-year flexibilities already announced are helpful, they are clearly not sufficient to prevent large numbers of senior clinicians reducing their sessional commitments, including in A&E departments, general practice and undertaking waiting list operations. The Academy of Medical Royal Colleges provided further evidence of this in their letter to you and the Chancellor dated 4 November 2019, which I attach. Given the deferral of the Budget and the calling of an election, it is now clear that a substantive answer to the tapered annual allowance issue is unlikely to be forthcoming until the new tax year, from April 2020. In the meantime there is an urgent operational requirement to remediate further the situation, so as to try and remove barriers to needed clinical staffing over the winter period. To that end, as you know, we have been working with your officials and HMT on an in-year mitigation. This will involve a commitment to make payments to certain clinical staff outside of the NHS pension schemes to restore the value of their pension benefits package, if they have elected to use the “Scheme Pays” facility to settle an annual allowance tax charge arising from of their pension saving in the NHS schemes in 2019/20. -

Novel Coronavirus (COVID-19): Derby and Derbyshire Stakeholder Bulletin #32
View this email in your browser 6 November 2020 Novel Coronavirus (COVID-19): Derby and Derbyshire stakeholder bulletin #32 Dear partners Any doubt as to the seriousness of the situation we now find ourselves in was firmly put to bed on Saturday when the Prime Minister announced plans for a planned four-week lockdown in England from Thursday (5 November) at a Downing Street news conference on Saturday. On Wednesday, MPs overwhelmingly voted to proceed with the second lockdown (516 votes to 38) that is due to end on Wednesday 2 December. NHS Chief Executive, Sir Simon Stevens, also confirmed at a press conference on Wednesday that the NHS in England will be returning to its highest state of alert from midnight on Wednesday to coincide with the start of the second lockdown. The switch to level 4 means the NHS’s response to the resurgence of the pandemic is being handled nationally rather than regionally. The number of people seriously ill with coronavirus who are being treated in hospitals in England has risen from 2,000 at the end of September to almost 11,000. In Derbyshire there were over 200 patients with coronavirus in our hospitals at the end of last week and we are above that now. We’re seeing significant use of Intensive Care Unit beds in Chesterfield which means they can do less of their planned care operating. General practice remains incredibly busy and we are seeing an increase in: NHS 111 use Community nursing and community beds The total number of staff absences related to COVID Our projections tell us that we are approaching April levels for admissions, though lockdown will stem this. -

My Client: Dr Sam White I Am Instructed By
Exclusively Employment Law Solicitors Sir Simon Stevens Chief Executive Officer NHS England 2 July 2021 Dear Mr Stevens Re: My Client: Dr Sam White I am instructed by Dr Sam White, a GP. Dr Sam White has had his licence to practise within the NHS suspended by letter from the NHS dated 26 June 2021. Please treat this letter as a public interest disclosure or whistle blow in that it raises allegations of alleged criminal conduct and breach of legal obligations by those leading the covid response. The reasons given for my client’s suspension have been inconsistent. My client has been told one thing verbally and another in writing. Email [email protected] What my client has been told in writing is he has been suspended on the Web www.pjhlaw.co.uk basis of his social media output. Head office 18A Maiden Lane, Stamford, Lincolnshire, PE9 2AZ My client’s social media output does not differ in any material extent to other Tel 01780 757589 clinicians also with an online presence who have not been suspended. Fax 0844 8505806 Principal Philip Hyland My client raised concerns during his NHS five year revalidation appraisal Solicitors process with the NHS in November 2020. Liam Pike Samantha Crombie Joe Hyland All of these concerns were raised during the revalidation appraisal process and overlap with what is in my client’s social media content. PJH Law is authorised and regulated by the Solicitors Regulation Authority under number 571808 The NHS took no action on either the substance of the concerns raised in my client’s appraisal nor did the NHS take any action against my client for raising those concerns during his appraisal. -

NHS Foundation Trust Annual Reporting Manual 2020/21 – March 2021
NHS foundation trust annual reporting manual 2020/21 February 2021 Updated 31 March 2021 (changes listed on page 5) Contents Introduction ..............................................................................................................3 About NHS Improvement .....................................................................................3 Requirements for foundation trust annual reports and accounts ...........................3 Summary of changes for 2020/21: annual reports ................................................3 Further changes in March 2021 ...........................................................................5 Temporary changes in 2019/20 and 2020/21 .......................................................5 Signature arrangements .......................................................................................6 Update on quality reports .....................................................................................6 1. Annual report and accounts preparation and submission requirements ......7 Annex 1 to Chapter 1: Directions........................................................................ 16 Annex 2 to Chapter 1: Example Certificate on Summarisation Schedules .......... 19 2. Annual reporting guidance for NHS foundation trusts .................................. 20 Content of the annual report ............................................................................... 20 Principles to follow when preparing the annual report ........................................ 20 Performance -

2019-20 Annual Report & Accounts
Barnsley Hospital NHS Foundation Trust Annual Report and Accounts 1 April 2019 to 31 March 2020 Presented to Parliament Pursuant to Schedule 7, Paragraph 25(4) (a) of the National Health Service Act 2006 © 2020 Barnsley Hospital NHS Foundation Trust Contents Performance Report 1 Accountability Report 44 Director’s Report 44 Remuneration Report 61 Staff Report 72 Governance Report 104 Statement of Accounting Officer’s Responsibilities 133 Annual Governance Statement 135 Financial Statements 149 1 Performance Report The purpose of this section of the report is to provide a short summary of Barnsley hospital NHS Foundation Trust, our purpose, the key risks to achievement of our objectives and how The Trust has performed during the reporting period. About Barnsley Hospital Barnsley Hospital NHS Foundation Trust is a district general hospital built in the 1970s and serving a population of approximately a quarter of a million people within the areas served by Barnsley Metropolitan Borough Council. The hospital provides a full range of district hospital services to the local community and surrounding area. These services include emergency and intensive care, medical and surgical care, elderly care, paediatric and maternity services, along with diagnostic and clinical support. The Trust provides a number of specialised services, such as cancer and surgical services in partnership with other NHS organisations. The Trust also provides national assistive technology services. Barnsley Assistive Technology is a nationally recognised specialised service that works with other professionals in local teams to provide electronic assistive technology. The service works with a wide range of electronic assistive technologies and with a wide range of individuals with severe disabilities. -

Service User Involvement in Health and Social Care Policy and Legislation
National Involvement Principles Purpose Presence Process Impact Standards This compendium aims to provide an overview of service user involvement in health and social care policy and legislation. It functions as a companion piece to the 4Pi Standards for Involvement document and aims to enable readers to use it for reference purposes. Service User Involvement in Health and Social Care Policy and Legislation Nothing about us without us In association with: National Involvement National Survivor Funded by the Partnership User Network Department of Health National 2 Involvement Standards Service User Involvement in Health and Social Care Policy and Legislation This compendium aims to provide an overview of service user involvement in health and social care policy and legislation. It charts developments chronologically from the NHS and Community Care Act of 1990 to the present day. The compendium functions as a companion piece to the 4Pi Standards for Involvement document and aims to enable readers to use it for reference purposes. Where possible, specific references and web links to original documents have been included. Whilst aiming to be as comprehensive as possible we recognise that this is an evolving document and that further key reports may come to light. A degree of selection has also been required in order to prevent the document from losing focus and becoming unwieldy. 1990 NHS and Community Care Act Legislation The NHS and Community Care Act is widely cited as the first piece of UK legislation to establish a formal requirement for user involvement in service planning. Local authorities were required to prepare Community Care Plans and consult with groups that represented people who used, or were likely to use, services.