Complications Resulting from Misdiagnosing Pseudogout As Sepsis
Total Page:16
File Type:pdf, Size:1020Kb
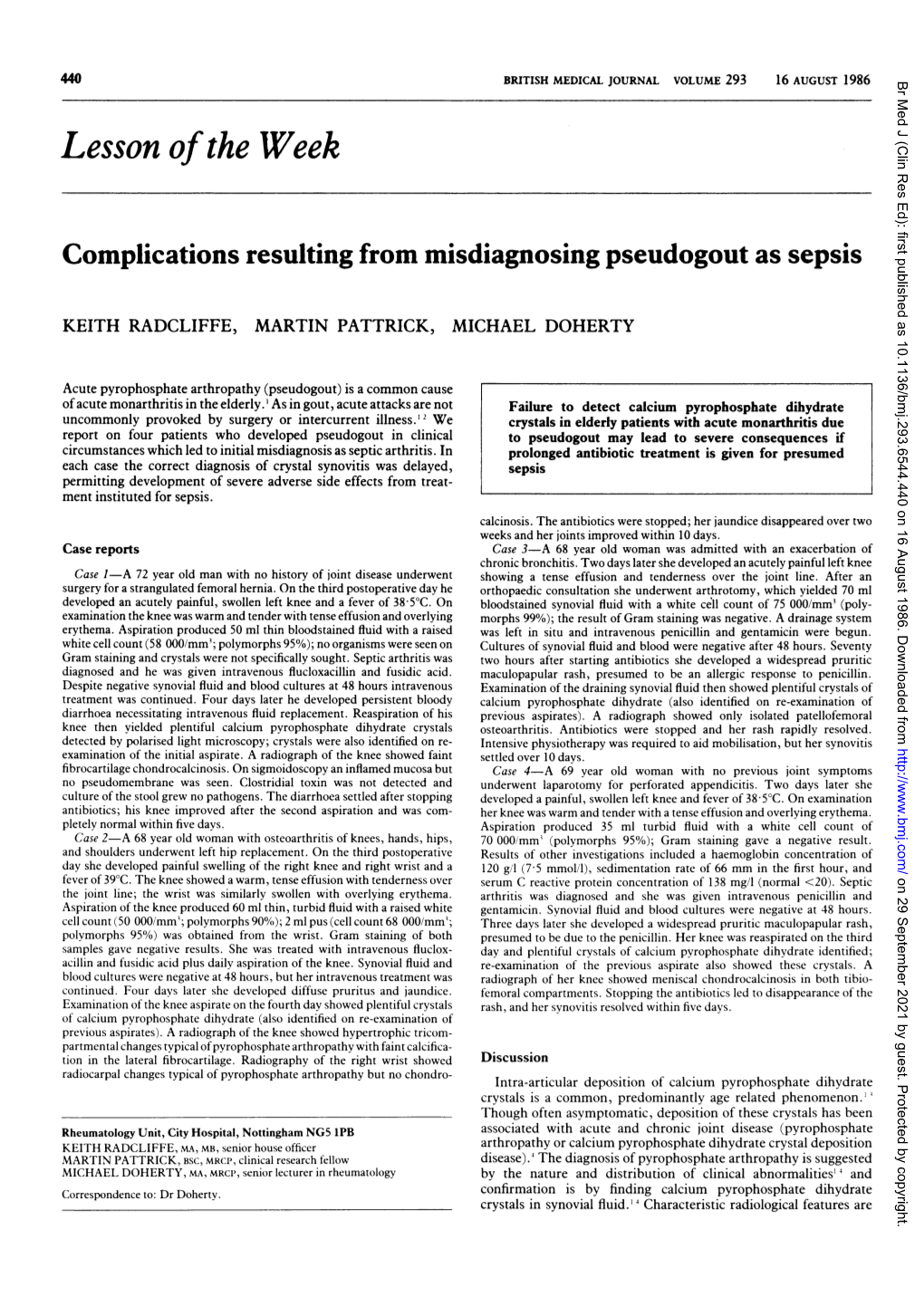
Load more
Recommended publications
-

Updated Treatment for Calcium Pyrophosphate Deposition Disease: an Insight
Open Access Review Article DOI: 10.7759/cureus.3840 Updated Treatment for Calcium Pyrophosphate Deposition Disease: An Insight Shumaila M. Iqbal 1 , Sana Qadir 2 , Hafiz M. Aslam 3 , Madiha A. Qadir 4 1. Internal Medicine, University at Buffalo / Sisters of Charity Hospital, Buffalo, USA 2. Internal Medicine, S & A Pediatrics, Parsippany, USA 3. Internal Medicine, Seton Hall University / Hackensack Meridian School of Medicine, Trenton, USA 4. Internal Medicine, Jinnah Sindh Medical University, Karachi, PAK Corresponding author: Shumaila M. Iqbal, [email protected] Abstract Calcium pyrophosphate disease (CPPD) is caused by the deposition of calcium pyrophosphate (CPP) crystals in the joint tissues, particularly fibrocartilage and hyaline cartilage. CPP crystals trigger inflammation, causing local articular tissue damage. Our review article below covers different aspects of CPPD. It discusses how CPPD can manifest as different kinds of arthritis, which may be symptomatic or asymptomatic. The metabolic and endocrine disease associations and routine investigations used in the diagnostic workup are briefly reviewed. Conventional and newer therapies for the treatment of CPPD are outlined. Overall, this extensive review would provide an updated insight to clinicians for evidence-based treatment of CPPD. Categories: Rheumatology Keywords: calcium pyrophosphate deposition disease, calcium pyrophosphate crystal, arthritis, colchicine, immunomodulants, nsaid Introduction And Background Calcium pyrophosphate deposition disease (CPPD) is caused by the deposition of calcium pyrophosphate (CCP) crystals in the articular cartilage, resulting in inflammation and degenerative changes in the affected joint. CPPD is a collective term that comprises all the various forms of CPP crystal-induced arthropathies. The acute arthritis attack caused by CPP crystals deposition triggers the same inflammatory reaction in the joint tissues as do the monosodium urate crystals in gout patients. -

ACR Appropriateness Criteria® Chronic Knee Pain
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Chronic Knee Pain Variant 1: Adult or child greater than or equal to 5 years of age. Chronic knee pain. Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography knee Usually Appropriate ☢ Image-guided aspiration knee Usually Not Appropriate Varies CT arthrography knee Usually Not Appropriate ☢ CT knee with IV contrast Usually Not Appropriate ☢ CT knee without and with IV contrast Usually Not Appropriate ☢ CT knee without IV contrast Usually Not Appropriate ☢ MR arthrography knee Usually Not Appropriate O MRI knee without and with IV contrast Usually Not Appropriate O MRI knee without IV contrast Usually Not Appropriate O Bone scan knee Usually Not Appropriate ☢☢☢ US knee Usually Not Appropriate O Radiography hip ipsilateral Usually Not Appropriate ☢☢☢ Variant 2: Adult or child greater than or equal to 5 years of age. Chronic knee pain. Initial knee radiograph negative or demonstrates joint effusion. Next imaging procedure. Procedure Appropriateness Category Relative Radiation Level MRI knee without IV contrast Usually Appropriate O Image-guided aspiration knee May Be Appropriate Varies CT arthrography knee May Be Appropriate ☢ CT knee without IV contrast May Be Appropriate ☢ US knee May Be Appropriate (Disagreement) O Radiography hip ipsilateral May Be Appropriate ☢☢☢ Radiography lumbar spine May Be Appropriate ☢☢☢ MR arthrography knee May Be Appropriate O MRI knee without and with IV contrast Usually Not Appropriate O CT knee with IV contrast Usually Not Appropriate ☢ CT knee without and with IV contrast Usually Not Appropriate ☢ Bone scan knee Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Chronic Knee Pain Variant 3: Adult or child greater than or equal to 5 years of age. -

Imaging in Gout and Other Crystal-Related Arthropathies 625
ImaginginGoutand Other Crystal-Related Arthropathies a, b Patrick Omoumi, MD, MSc, PhD *, Pascal Zufferey, MD , c b Jacques Malghem, MD , Alexander So, FRCP, PhD KEYWORDS Gout Crystal arthropathy Calcification Imaging Radiography Ultrasound Dual-energy CT MRI KEY POINTS Crystal deposits in and around the joints are common and most often encountered as inci- dental imaging findings in asymptomatic patients. In the chronic setting, imaging features of crystal arthropathies are usually characteristic and allow the differentiation of the type of crystal arthropathy, whereas in the acute phase and in early stages, imaging signs are often nonspecific, and the final diagnosis still relies on the analysis of synovial fluid. Radiography remains the primary imaging tool in the workup of these conditions; ultra- sound has been playing an increasing role for superficially located crystal-induced ar- thropathies, and computerized tomography (CT) is a nice complement to radiography for deeper sites. When performed in the acute stage, MRI may show severe inflammatory changes that could be misleading; correlation to radiographs or CT should help to distinguish crystal arthropathies from infectious or tumoral conditions. Dual-energy CT is a promising tool for the characterization of crystal arthropathies, partic- ularly gout as it permits a quantitative assessment of deposits, and may help in the follow-up of patients. INTRODUCTION The deposition of microcrystals within and around the joint is a common phenomenon. Intra-articular microcrystals -

21362 Arthritis Australia a to Z List
ARTHRITISINFORMATION SHEET Here is the A to Z of arthritis! A D Goodpasture’s syndrome Achilles tendonitis Degenerative joint disease Gout Achondroplasia Dermatomyositis Granulomatous arteritis Acromegalic arthropathy Diabetic finger sclerosis Adhesive capsulitis Diffuse idiopathic skeletal H Adult onset Still’s disease hyperostosis (DISH) Hemarthrosis Ankylosing spondylitis Discitis Hemochromatosis Anserine bursitis Discoid lupus erythematosus Henoch-Schonlein purpura Avascular necrosis Drug-induced lupus Hepatitis B surface antigen disease Duchenne’s muscular dystrophy Hip dysplasia B Dupuytren’s contracture Hurler syndrome Behcet’s syndrome Hypermobility syndrome Bicipital tendonitis E Hypersensitivity vasculitis Blount’s disease Ehlers-Danlos syndrome Hypertrophic osteoarthropathy Brucellar spondylitis Enteropathic arthritis Bursitis Epicondylitis I Erosive inflammatory osteoarthritis Immune complex disease C Exercise-induced compartment Impingement syndrome Calcaneal bursitis syndrome Calcium pyrophosphate dehydrate J (CPPD) F Jaccoud’s arthropathy Crystal deposition disease Fabry’s disease Juvenile ankylosing spondylitis Caplan’s syndrome Familial Mediterranean fever Juvenile dermatomyositis Carpal tunnel syndrome Farber’s lipogranulomatosis Juvenile rheumatoid arthritis Chondrocalcinosis Felty’s syndrome Chondromalacia patellae Fibromyalgia K Chronic synovitis Fifth’s disease Kawasaki disease Chronic recurrent multifocal Flat feet Kienbock’s disease osteomyelitis Foreign body synovitis Churg-Strauss syndrome Freiberg’s disease -
View a Copy of This Licence, Visit Iveco Mmons. Org/ Licen Ses/ By/4. 0/
Leyens et al. Orphanet J Rare Dis (2021) 16:326 https://doi.org/10.1186/s13023-021-01945-8 RESEARCH Open Access The combined prevalence of classifed rare rheumatic diseases is almost double that of ankylosing spondylitis Judith Leyens1,2, Tim Th. A. Bender1,3, Martin Mücke1, Christiane Stieber4, Dmitrij Kravchenko1,5, Christian Dernbach6 and Matthias F. Seidel7* Abstract Background: Rare diseases (RDs) afect less than 5/10,000 people in Europe and fewer than 200,000 individuals in the United States. In rheumatology, RDs are heterogeneous and lack systemic classifcation. Clinical courses involve a variety of diverse symptoms, and patients may be misdiagnosed and not receive appropriate treatment. The objec- tive of this study was to identify and classify some of the most important RDs in rheumatology. We also attempted to determine their combined prevalence to more precisely defne this area of rheumatology and increase awareness of RDs in healthcare systems. We conducted a comprehensive literature search and analyzed each disease for the speci- fed criteria, such as clinical symptoms, treatment regimens, prognoses, and point prevalences. If no epidemiological data were available, we estimated the prevalence as 1/1,000,000. The total point prevalence for all RDs in rheumatol- ogy was estimated as the sum of the individually determined prevalences. Results: A total of 76 syndromes and diseases were identifed, including vasculitis/vasculopathy (n 15), arthritis/ arthropathy (n 11), autoinfammatory syndromes (n 11), myositis (n 9), bone disorders (n 11),= connective tissue diseases =(n 8), overgrowth syndromes (n 3), =and others (n 8).= Out of the 76 diseases,= 61 (80%) are clas- sifed as chronic, with= a remitting-relapsing course= in 27 cases (35%)= upon adequate treatment. -

Hemarthrosis
Case Report DOI: 10.5455/amaj.2016.02.012 Hemarthrosis: Concurrent acute presentation of pyrophosphate dehydrate and uric acid crystals in an elderly patient with a history of rheumatoid ar- thritis diagnosed with septic arthritis Feredun Azari, BS-MD Rauf Shahbazov, MD, PhD* Concomitant septic arthritis in the presence of crystalline disease is a rare presen- tation of acute hemarthrosis and knee pain. Literature review showed that co-occur- Department of Surgery, rence of these entities is an infrequent phenomenon but it needs to be acknowledged University of Virginia, that these studies are few in number and were done on small patient population. This Charlottesville, Virginia, USA case challenges the notion that presence of crystals in the synovial fluid rules out sep- tic arthritis even in the setting of low synovial WBC count. Additionally, the presence Correspondence: of pseudogout in patients suffering from gout is a rare entity as well. These findings Rauf Shahbazov MD, PhD, Organ Trans- in literature are described in case reports dispersed over the past three decades. We plantation Unit, University of Virginia present a case where concurrent treatment of gout, pseudogout, and septic arthritis Medical Center, Charlottesville, Virginia, in a patient who presented with acute hemarhtrosis. USA email: [email protected] Keywords: gout, pseudogout, rheumatoid arthritis, infection Phone: 434-872-1373 Introduction tions [1]. Vigilance is needed to have a low ge related crystal induced arthropathies threshold for ruling out septic arthritis in Aare a common phenomenon presenting this patient population. This is usually done to the primary care office or the emergency via synovial fluid analysis but as demon- department [1,2]. -

New Knowledge of Chondrocalcinosis
J Clin Pathol: first published as 10.1136/jcp.s3-12.1.214 on 1 January 1978. Downloaded from J. clin. Path., 31, Suppl. (Roy. Coll. Path.), 12, 214-222 New knowledge of chondrocalcinosis PAUL DIEPPE From the Department ofMedicine, University ofBristol There are three varieties of cartilage-hyaline, parathyroidism, haemachromatosis, hypothy- elastic, and fibrocartilage. Hyaline cartilage is the roidism, hypophosphataxia, hypomagnesaemia, precursor of bone. In the adult it is mainly found at gout(?), diabetes mellitus (?), Wilson's disease (?), bone ends, forming the load-bearing surface of ochronosis (?)). synovial joints. Extra-articular fibrocartilages such as those of the trachea and ribs often calcify with Historical perspective advancing age. Articular cartilage, however, usually remains free from mineral deposits. The term Intra-articular calcification has been recognisedforat 'chondrocalcinosis' may be defined as a pathological least a century. It was mentioned by Garrod (1876) state characterised by the precipitation of insoluble and by Adams (1872). With the advent of joint calcium salts in articular and periarticular cartilage. radiography there were a number of reports of The presence of chondrocalcinosis can be proved calcification of knee menisci (Pearson and Davin, only by crystallographic examination. Its presence 1921). Wolke (1935) described five cases from 2569 may be inferred by radiological examination or the knee radiographs. Zit'nan and Sifaj (1957) described discovery of crystals in synovial fluid. In addition, 12 cases, and they later identified familial cases with articular chondrocalcinosis is sometimes accom- polyarticular lesions and an associated arthritis copyright. panied by arthritis. There are therefore three (2itnian and Silaj, 1976). separate phenomena associated with chondrocal- While 2ithan and Sifaj surveyed joint radiographs cinosis-radiological changes, crystals in synovial Hollander and McCarty (1961) examined joint fluid, and arthritis. -

Mutations in ANKH Cause Chondrocalcinosis Adrian Pendleton,1,2,* Michelle D
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Am. J. Hum. Genet. 71:933–940, 2002 Mutations in ANKH Cause Chondrocalcinosis Adrian Pendleton,1,2,* Michelle D. Johnson,3,* Anne Hughes,1 Kyle A. Gurley,3,* Andrew M. Ho,3 Michael Doherty,4 Josh Dixey,5 Pierre Gillet,7 Damien Loeuille,7 Rodney McGrath,6 Antonio Reginato,8 Rita Shiang,9 Gary Wright,2 Patrick Netter,7 Charlene Williams,6 and David M. Kingsley3 1Department of Medical Genetics, The Queen’s University of Belfast, and 2Department of Rheumatology, Royal Victoria Hospital, Belfast; 3HHMI and Department of Developmental Biology, Stanford University School of Medicine, Stanford CA; 4Academic Rheumatology, City Hospital, Nottingham, United Kingdom; 5Rheumatology, Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, United Kingdom; 6Departments of Medicine and Biochemistry/Molecular Pharmacology, Thomas Jefferson University, Philadelphia; 7UMR 7561 Centre National de la Recherche Scientifique-Universite Henri Poincare et Clinique Rhumatologique, Nancy, France; 8Division of Rheumatology, University of Medicine and Dentistry of New Jersey, Camden; and 9Department of Human Genetics, Virginia Commonwealth University, Richmond Chondrocalcinosis (CC) is a common cause of joint pain and arthritis that is caused by the deposition of calcium- containing crystals within articular cartilage. Although most cases are sporadic, rare familial forms have been linked to human chromosomes 8 (CCAL1)or5p(CCAL2) (Baldwin et al. 1995; Hughes et al. 1995; Andrew et al. 1999). Here, we show that two previously described families with CCAL2 have mutations in the human homolog of the mouse progressive ankylosis gene (ANKH). -

Pseudogout: Uncommon and Under-Recognized
20 Osteopathic Family Physician (2019) 20 - 22 Osteopathic Family Physician | Volume 11, No. 6 | November/December, 2019 Review ARTICLE Pseudogout: Uncommon and Under-Recognized Scott R. Brown, DO1; Alissa M. Cohen, MS, DO1 1University of Pittsburgh Medical Center, Shadyside Hospital, Pittsburgh, PA KEYWORDS: ABSTRACT: Pseudogout or calcium pyrophosphate deposition (CPPD) disease is an uncommon and often under-recognized presentation in primary care. Patients may initially develop Chondrocalcinosis asymptomatic crystal deposition, but these changes can evolve to synovitis, arthritis, and CPPD cartilage calcification. An initial differential diagnosis includes traditional gout, osteoarthritis, rheumatoid arthritis, septic arthritis, and Lyme disease. Acute attacks of CPPD may be CPPD Disease indistinguishable from these conditions clinically, and a definitive diagnosis requires synovial fluid analysis. Fluid should be microscopically analyzed for cell count, crystal analysis under Calcium Pyrophosphate compensated polarizing microscopy, Gram stain, and culture. CPPD crystals are weakly Deposition Disease birefringent under polarized light and have a rhomboid or rod-shaped appearance. No therapy Pseudogout is proven optimal, so CPPD treatment is instead tailored to symptoms, with goals of controlling acute pain, preventing additional attacks, and impeding the degenerative joint disease associated with CPPD disease arthropathy. Current treatment methods include intra-articular corticosteroid injections, NSAIDs, DMARDs, OMT, and in severe, refractory cases, surgery. INTRODUCTION/EPIDEMIOLOGY asymptomatic crystal deposition, these changes can evolve to synovitis and arthritis, and even cartilage calcification. Given these Calcium Pyrophosphate Deposition disease, also known as features, an initial differential diagnosis includes traditional gout, CPPD disease or Pseudogout, is an uncommon and often osteoarthritis, rheumatoid arthritis, septic arthritis, and Lyme under-recognized presentation in primary care. -

Chondrocalcinosis, Osteophytes and Osteoarthritis
LEADER 499 Osteoarthritis limitations of the standing anteroposte- ................................................................................... rior radiograph for accurate and repro- Ann Rheum Dis: first published as 10.1136/ard.62.6.499 on 1 June 2003. Downloaded from ducible assessment of JSN in patients with OA.8 The issue concerns the import- Chondrocalcinosis, osteophytes and ance of alignment of the central x ray beam with the plane of the medial tibial osteoarthritis plateau in assessment of tibiofemoral compartment joint space width, a de- K D Brandt crease in which is generally taken as an indication of the radiographic severity of ................................................................................... OA and, in serial examinations, of progression of cartilage damage. Fluoro- Crystals, spurs, and osteoarthritis scopically assisted positioning of the joints to align the tibiofemoral compart- Association between OA and the articular surface in vivo.4 Further- ment (that is, with anterior and posterior chondrocalcinosis more, calcium crystals are phlogistic; margins of the medial tibial plateau An association between osteoarthritis their presence within the joint space and superimposed ±1 mm), as with the tech- 9 (OA) and radiographic evidence of chon- synovium may initiate an inflammatory nique described by Buckland-Wright, is drocalcinosis (CC) has been recognised response.5 associated with a more rapid rate of JSN, for years. Crystals of calcium pyrophos- and smaller standard deviation of the phate dihydrate (CPPD) may be found in Radiography of OA rate of narrowing, than protocols that synovial fluid from patients with OA who The paper by Neame et al in this issue of are less effective in providing tibial 10 are relatively asymptomatic as well as the Annals examines the association plateau alignment. -
Calcium Pyrophosphate Crystal Deposition
Review Calcium pyrophosphate crystal deposition Even though frequently asymptomatic, for some patients calcium pyrophosphate crystal deposition remains a troublesome disorder; these patients can present with recurrent episodes of painful monoarthritis, with persistent polyarticular inflammation or with mechanical joint pain and osteoarthritic changes. The features of the disease may mimic other rheumatic and nonrheumatic conditions, with misdiagnosis being a common problem. Frequently, calcium pyrophosphate crystal deposition is discovered through the incidental finding of chondrocalcinosis on x‑rays. Despite being a relevant and poorly understood disorder, it has received little attention from the medical community and the flux of new insights is low when compared with other rheumatic diseases. This paper will review calcium pyrophosphate crystal deposition, stressing the significance of recent contributions in terminology, pathogenesis and management. 1 k Eywords: calcium pyrophosphate crystals n chondrocalcinosis n CPPd Francisca Sivera* , n pseudogout n pyrophosphate arthropathy n synovial fluid analysis Mariano Andres2 & Eliseo Pascual2,3 1S. Reumatologia. Hospital de Elda. Arthropathy related to calcium pyrophosphate lanthanic or asymptomatic (type E), pseudo‑ Alicante, Spain 2S. Reumatologia. Hospital General (CPP) dihydrate crystals has received little critical neuropathic (type F) and others [3]. Furthermore Universitario de Alicante. Alicante, attention. In the most typical cases – acute knee the term pyrophosphate arthropathy -

The Relationship Between Vitamin K and Osteoarthritis: a Review of Current Evidence
nutrients Review The Relationship between Vitamin K and Osteoarthritis: A Review of Current Evidence Kok-Yong Chin Department of Pharmacology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Cheras 56000, Malaysia; [email protected]; Tel.: +603-9145-9573 Received: 10 February 2020; Accepted: 23 April 2020; Published: 25 April 2020 Abstract: Vitamin K is a cofactor of γ-glutamyl carboxylase, which plays an important role in the activation of γ-carboxyglutamate (gla)-containing proteins that negatively regulate calcification. Thus, vitamin K status might be associated with osteoarthritis (OA), in which cartilage calcification plays a role in the pathogenesis of the disease. This review collates the evidence on the relationship between vitamin K status (circulating or dietary intake level of vitamin K, or circulating uncarboxylated gla proteins) and OA from human observational studies and clinical trial, to examine its potential as an agent in preventing OA. The current literature generally agrees that a sufficient level of vitamin K is associated with a lower risk of OA and pathological joint features. However, evidence from clinical trials is limited. Mechanistic study shows that vitamin K activates matrix gla proteins that inhibit bone morphogenetic protein-mediated cartilage calcification. Gla-rich proteins also inhibit inflammatory cascade in monocytic cell lines, but this function might be independent of vitamin K-carboxylation. Although the current data are insufficient to establish the optimal dose of vitamin K to prevent OA, ensuring sufficient dietary intake seems to protect the elderly from OA. Keywords: carboxylation; cartilage; joint; menaquinone; phylloquinone 1. Introduction Osteoarthritis (OA) is a debilitating disease of the movable joints commonly experienced by the elderly.