Monoarticular Inflammatory Arthritis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Updated Treatment for Calcium Pyrophosphate Deposition Disease: an Insight
Open Access Review Article DOI: 10.7759/cureus.3840 Updated Treatment for Calcium Pyrophosphate Deposition Disease: An Insight Shumaila M. Iqbal 1 , Sana Qadir 2 , Hafiz M. Aslam 3 , Madiha A. Qadir 4 1. Internal Medicine, University at Buffalo / Sisters of Charity Hospital, Buffalo, USA 2. Internal Medicine, S & A Pediatrics, Parsippany, USA 3. Internal Medicine, Seton Hall University / Hackensack Meridian School of Medicine, Trenton, USA 4. Internal Medicine, Jinnah Sindh Medical University, Karachi, PAK Corresponding author: Shumaila M. Iqbal, [email protected] Abstract Calcium pyrophosphate disease (CPPD) is caused by the deposition of calcium pyrophosphate (CPP) crystals in the joint tissues, particularly fibrocartilage and hyaline cartilage. CPP crystals trigger inflammation, causing local articular tissue damage. Our review article below covers different aspects of CPPD. It discusses how CPPD can manifest as different kinds of arthritis, which may be symptomatic or asymptomatic. The metabolic and endocrine disease associations and routine investigations used in the diagnostic workup are briefly reviewed. Conventional and newer therapies for the treatment of CPPD are outlined. Overall, this extensive review would provide an updated insight to clinicians for evidence-based treatment of CPPD. Categories: Rheumatology Keywords: calcium pyrophosphate deposition disease, calcium pyrophosphate crystal, arthritis, colchicine, immunomodulants, nsaid Introduction And Background Calcium pyrophosphate deposition disease (CPPD) is caused by the deposition of calcium pyrophosphate (CCP) crystals in the articular cartilage, resulting in inflammation and degenerative changes in the affected joint. CPPD is a collective term that comprises all the various forms of CPP crystal-induced arthropathies. The acute arthritis attack caused by CPP crystals deposition triggers the same inflammatory reaction in the joint tissues as do the monosodium urate crystals in gout patients. -

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -
Uncontrolled Gout Fact Sheet
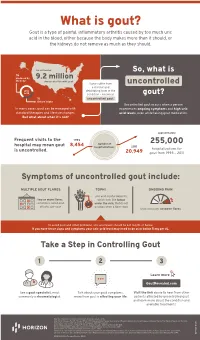
What is gout? Gout is a type of painful, inflammatory arthritis caused by too much uric acid in the blood, either because the body makes more than it should, or the kidneys do not remove as much as they should. An estimated So, what is ⅔ produced by 9.2 million the body Americans live with gout Some suffer from uncontrolled a chronic and uric debilitating form of the acid condition – known as gout? ⅓ uncontrolled gout. dietary intake Uncontrolled gout occurs when a person In many cases, gout can be managed with experiences ongoing symptoms and high uric standard therapies and lifestyle changes. acid levels, even while taking gout medication. But what about when it’s not? approximately Frequent visits to the 1993 number of 255,000 hospital may mean gout 8,454 hospitalizations 2011 is uncontrolled. hospitalizations for 20,949 gout from 1993 – 2011 Symptoms of uncontrolled gout include: MULTIPLE GOUT FLARES TOPHI ONGOING PAIN uric acid crystal deposits, two or more flares, which look like lumps sometimes called gout under the skin, that do not attacks, per year go away when a flare stops that continues between flares To avoid gout and other problems, uric acid levels should be 6.0 mg/dL or below. If you have these signs and symptoms your uric acid level may need to be at or below 5 mg per dL. Take a Step in Controlling Gout 1 2 3 Learn more GoutRevealed.com See a gout specialist, most Talk about your gout symptoms, Visit the link above to hear from other commonly a rheumatologist. -

Acute < 6 Weeks Subacute ~ 6 Weeks Chronic >
Pain Articular Non-articular Localized Generalized . Regional Pain Disorders . Myalgias without Weakness Soft Tissue Rheumatism (ex., fibromyalgia, polymyalgia (ex., soft tissue rheumatism rheumatica) tendonitis, tenosynovitis, bursitis, fasciitis) . Myalgia with Weakness (ex., Inflammatory muscle disease) Clinical Features of Arthritis Monoarthritis Oligoarthritis Polyarthritis (one joint) (two to five joints) (> five joints) Acute < 6 weeks Subacute ~ 6 weeks Chronic > 6 weeks Inflammatory Noninflammatory Differential Diagnosis of Arthritis Differential Diagnosis of Arthritis Acute Monarthritis Acute Polyarthritis Inflammatory Inflammatory . Infection . Viral - gonococcal (GC) - hepatitis - nonGC - parvovirus . Crystal deposition - HIV - gout . Rheumatic fever - calcium . GC - pyrophosphate dihydrate (CPPD) . CTD (connective tissue diseases) - hydroxylapatite (HA) - RA . Spondyloarthropathies - systemic lupus erythematosus (SLE) - reactive . Sarcoidosis - psoriatic . - inflammatory bowel disease (IBD) Spondyloarthropathies - reactive - Reiters . - psoriatic Early RA - IBD - Reiters Non-inflammatory . Subacute bacterial endocarditis (SBE) . Trauma . Hemophilia Non-inflammatory . Avascular Necrosis . Hypertrophic osteoarthropathy . Internal derangement Chronic Monarthritis Chronic Polyarthritis Inflammatory Inflammatory . Chronic Infection . Bony erosions - fungal, - RA/Juvenile rheumatoid arthritis (JRA ) - tuberculosis (TB) - Crystal deposition . Rheumatoid arthritis (RA) - Infection (15%) - Erosive OA (rare) Non-inflammatory - Spondyloarthropathies -

Arthritis (Overview)
ARTHRITIS Having arthritis can significantly affect your comfort & ability to walk and move with confidence. This is because it affects your joints, which are responsible for keeping you steady and moving efficiently. Your symptoms and causes will depend on the type of arthritis that you have. At Masterton Foot Clinic, our podiatrists work closely with patients with four types of arthritis. OSTEOARTHRITIS Osteoarthritis is the wear and tear arthritis that develops slowly over time as the cartilage that covers your bone ends wears down. The cause is largely from natural use over many years, though injuries, alignment issues within the joint and other diseases may result in it developing at a faster rate. We work with patients that want to feel more comfortable on their feet, despite having arthritis in their hip, knee, ankle and foot joints. RHEUMATOID ARTHRITIS Rheumatoid arthritis is an autoimmune disease that affects the joints. It occurs when your body’s immune system attacks the joints and causes damage, inflammation and pain. If the effects of rheumatoid arthritis remain uncontrolled, it can cause permanent changes in the appearance of the joints, especially at the feet and hands. We work with patients to help them manage the discomfort associated with rheumatoid arthritis, offloading prominent and painful areas that have developed due to changes in the joints. GOUT Gout is an inflammatory arthritis that results from a high concentration of uric acid in the blood. It is associated with a high intake of purine-containing foods like red meats, shellfish and red wine, hence it was previously referred to as the rich man’s disease. -

Variation in the Initial Treatment of Knee Monoarthritis in Juvenile Idiopathic Arthritis: a Survey of Pediatric Rheumatologists in the United States and Canada
Variation in the Initial Treatment of Knee Monoarthritis in Juvenile Idiopathic Arthritis: A Survey of Pediatric Rheumatologists in the United States and Canada TIMOTHY BEUKELMAN, JAMES P. GUEVARA, DANIEL A. ALBERT, DAVID D. SHERRY, and JON M. BURNHAM ABSTRACT. Objective. To characterize variations in initial treatment for knee monoarthritis in the oligoarthritis sub- type of juvenile idiopathic arthritis (OJIA) by pediatric rheumatologists and to identify patient, physi- cian, and practice-specific characteristics that are associated with treatment decisions. Methods. We mailed a 32-item questionnaire to pediatric rheumatologists in the United States and Canada (n = 201). This questionnaire contained clinical vignettes describing recent-onset chronic monoarthritis of the knee and assessed physicians’ treatment preferences, perceptions of the effective- ness and disadvantages of nonsteroidal antiinflammatory drugs (NSAID) and intraarticular corticos- teroid injections (IACI), proficiency with IACI, and demographic and office characteristics. Results. One hundred twenty-nine (64%) questionnaires were completed and returned. Eighty-three per- cent of respondents were board certified pediatric rheumatologists. Respondents’ treatment strategies for uncomplicated knee monoarthritis were broadly categorized: initial IACI at presentation (27%), initial NSAID with contingent IACI (63%), and initial NSAID with contingent methotrexate or sulfasalazine (without IACI) (10%). Significant independent predictors for initial IACI were believing that IACI is more effective than NSAID, having performed > 10 IACI in a single patient at one time, and initiating methotrexate via the subcutaneous route for OJIA. Predictors for not recommending initial or contin- gent IACI were believing that the infection risk of IACI is significant and lacking comfort with per- forming IACI. Conclusion. There is considerable variation in pediatric rheumatologists’ initial treatment strategies for knee monoarthritis in OJIA. -

Concurrent Onset of Adult Onset Still's Disease and Insulin Dependent Diabetes Mellitus
Annals ofthe Rheumatic Diseases 1990; 49: 547-548 547 Concurrent onset of adult onset Still's disease and Ann Rheum Dis: first published as 10.1136/ard.49.7.547 on 1 July 1990. Downloaded from insulin dependent diabetes mellitus J T Sibley Abstract time, partial thromboplastin time, C3, C4, Clq Within two weeks after symptoms of an upper binding, tri-iodothyronine, thyroxine, serum respiratory tract infection a 32 year old man amylase, serum protein electrophoresis, and developed Still's disease and insulin dependent gallium scan. diabetes mellitus, both ofwhich have persisted Initial and convalescent serum rubella titres for 24 months. Investigations failed to confirm (haemagglutination inhibition) were both 1/640. acute infection but did show isolated persistent Hepatic transaminases were five times normal. increase of serum antibodies to rubelia virus. Abdominal ultrasound confirmed splenomegaly The simultaneous onset of these two diseases and showed decreased echogenicity of the suggests a shared cause, possibly associated pancreas. An abdominal computed tomography with rubella infection. scan was normal except for hepatosplenomegaly. Percutaneous liver biopsy showed only minor focal portal tract inflammation. A two dimen- Adult onset Still's disease is an uncommon sional echocardiogram showed a small peri- entity characterised by a multisystem illness cardial effusion. HLA typing results were with a wide constellation of features, notably A2,-;B44,5 1 ;Cw2,-;DR1,7. fever, rash, and arthritis.' Its cause is unknown, The diagnosis of adult onset Still's disease though there are a few reports of association was based on the typical clinical features, with viral illness.2A Insulin dependent diabetes including the characteristic evanescent rash and mellitus is also thought in some cases to have a daily fever in the absence ofclinical or laboratory viral cause,5 but I am unaware of any reports of confirmation of other diagnostic possibilities.' 6 the simultaneous onset of these two diseases. -

Biological Treatment in Resistant Adult-Onset Still's Disease: a Single-Center, Retrospective Cohort Study
Arch Rheumatol 2021;36(x):i-viii doi: 10.46497/ArchRheumatol.2021.8669 ORIGINAL ARTICLE Biological treatment in resistant adult-onset Still’s disease: A single-center, retrospective cohort study Seda Çolak, Emre Tekgöz, Maghrur Mammadov, Muhammet Çınar, Sedat Yılmaz Department of Internal Medicine, Division of Rheumatology, Gülhane Training and Research Hospital, Ankara, Turkey ABSTRACT Objectives: The aim of this study was to assess the demographic and clinical characteristics of patients with adult-onset Still’s disease (AOSD) under biological treatment. Patients and methods: This retrospective cohort study included a total of 19 AOSD patients (13 males, 6 females; median age: 37 years; range, 28 to 52 years) who received biological drugs due to refractory disease between January 2008 and January 2020. The data of the patients were obtained from the patient files. The response to the treatment was evaluated based on clinical and laboratory assessments at third and sixth follow-up visits. Results: Interleukin (IL)-1 inhibitor was prescribed for 13 (68.4%) patients and IL-6 inhibitor prescribed for six (31.6%) patients. Seventeen (89.5%) patients experienced clinical remission. Conclusion: Biological drugs seem to be effective for AOSD patients who are resistant to conventional therapies. Due to the administration methods and the high costs of these drugs, however, tapering the treatment should be considered, after remission is achieved. Keywords: Adult-onset Still’s disease, anakinra, tocilizumab, treatment. Adult-onset Still’s disease (AOSD) is a rare diseases that may lead to similar clinical and systemic inflammatory disease with an unknown laboratory findings. etiology. The main clinical manifestations of It is well known that proinflammatory the disease are fever, maculopapular salmon- pink rash, arthralgia, and arthritis. -

ACR Appropriateness Criteria® Chronic Knee Pain
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Chronic Knee Pain Variant 1: Adult or child greater than or equal to 5 years of age. Chronic knee pain. Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography knee Usually Appropriate ☢ Image-guided aspiration knee Usually Not Appropriate Varies CT arthrography knee Usually Not Appropriate ☢ CT knee with IV contrast Usually Not Appropriate ☢ CT knee without and with IV contrast Usually Not Appropriate ☢ CT knee without IV contrast Usually Not Appropriate ☢ MR arthrography knee Usually Not Appropriate O MRI knee without and with IV contrast Usually Not Appropriate O MRI knee without IV contrast Usually Not Appropriate O Bone scan knee Usually Not Appropriate ☢☢☢ US knee Usually Not Appropriate O Radiography hip ipsilateral Usually Not Appropriate ☢☢☢ Variant 2: Adult or child greater than or equal to 5 years of age. Chronic knee pain. Initial knee radiograph negative or demonstrates joint effusion. Next imaging procedure. Procedure Appropriateness Category Relative Radiation Level MRI knee without IV contrast Usually Appropriate O Image-guided aspiration knee May Be Appropriate Varies CT arthrography knee May Be Appropriate ☢ CT knee without IV contrast May Be Appropriate ☢ US knee May Be Appropriate (Disagreement) O Radiography hip ipsilateral May Be Appropriate ☢☢☢ Radiography lumbar spine May Be Appropriate ☢☢☢ MR arthrography knee May Be Appropriate O MRI knee without and with IV contrast Usually Not Appropriate O CT knee with IV contrast Usually Not Appropriate ☢ CT knee without and with IV contrast Usually Not Appropriate ☢ Bone scan knee Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Chronic Knee Pain Variant 3: Adult or child greater than or equal to 5 years of age. -

Gout and Monoarthritis
Gout and Monoarthritis Acute monoarthritis has numerous causes, but most commonly is related to crystals (gout and pseudogout), trauma and infection. Early diagnosis is critical in order to identify and treat septic arthritis, which can lead to rapid joint destruction. Joint aspiration is the gold standard method of diagnosis. For many reasons, managing gout, both acutely and as a chronic disease, is challenging. Registrars need to develop a systematic approach to assessing monoarthritis, and be familiar with the management of gout and other crystal arthropathies. TEACHING AND • Aetiology of acute monoarthritis LEARNING AREAS • Risk factors for gout and septic arthritis • Clinical features and stages of gout • Investigation of monoarthritis (bloods, imaging, synovial fluid analysis) • Joint aspiration techniques • Interpretation of synovial fluid analysis • Management of hyperuricaemia and gout (acute and chronic), including indications and targets for urate-lowering therapy • Adverse effects of medications for gout, including Steven-Johnson syndrome • Indications and pathway for referral PRE- SESSION • Read the AAFP article - Diagnosing Acute Monoarthritis in Adults: A Practical Approach for the Family ACTIVITIES Physician TEACHING TIPS • Monoarthritis may be the first symptom of an inflammatory polyarthritis AND TRAPS • Consider gonococcal infection in younger patients with monoarthritis • Fever may be absent in patients with septic arthritis, and present in gout • Fleeting monoarthritis suggests gonococcal arthritis or rheumatic fever -

Differential Diagnosis of Juvenile Idiopathic Arthritis
pISSN: 2093-940X, eISSN: 2233-4718 Journal of Rheumatic Diseases Vol. 24, No. 3, June, 2017 https://doi.org/10.4078/jrd.2017.24.3.131 Review Article Differential Diagnosis of Juvenile Idiopathic Arthritis Young Dae Kim1, Alan V Job2, Woojin Cho2,3 1Department of Pediatrics, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea, 2Department of Orthopaedic Surgery, Albert Einstein College of Medicine, 3Department of Orthopaedic Surgery, Montefiore Medical Center, New York, USA Juvenile idiopathic arthritis (JIA) is a broad spectrum of disease defined by the presence of arthritis of unknown etiology, lasting more than six weeks duration, and occurring in children less than 16 years of age. JIA encompasses several disease categories, each with distinct clinical manifestations, laboratory findings, genetic backgrounds, and pathogenesis. JIA is classified into sev- en subtypes by the International League of Associations for Rheumatology: systemic, oligoarticular, polyarticular with and with- out rheumatoid factor, enthesitis-related arthritis, psoriatic arthritis, and undifferentiated arthritis. Diagnosis of the precise sub- type is an important requirement for management and research. JIA is a common chronic rheumatic disease in children and is an important cause of acute and chronic disability. Arthritis or arthritis-like symptoms may be present in many other conditions. Therefore, it is important to consider differential diagnoses for JIA that include infections, other connective tissue diseases, and malignancies. Leukemia and septic arthritis are the most important diseases that can be mistaken for JIA. The aim of this review is to provide a summary of the subtypes and differential diagnoses of JIA. (J Rheum Dis 2017;24:131-137) Key Words. -

Imaging in Gout and Other Crystal-Related Arthropathies 625
ImaginginGoutand Other Crystal-Related Arthropathies a, b Patrick Omoumi, MD, MSc, PhD *, Pascal Zufferey, MD , c b Jacques Malghem, MD , Alexander So, FRCP, PhD KEYWORDS Gout Crystal arthropathy Calcification Imaging Radiography Ultrasound Dual-energy CT MRI KEY POINTS Crystal deposits in and around the joints are common and most often encountered as inci- dental imaging findings in asymptomatic patients. In the chronic setting, imaging features of crystal arthropathies are usually characteristic and allow the differentiation of the type of crystal arthropathy, whereas in the acute phase and in early stages, imaging signs are often nonspecific, and the final diagnosis still relies on the analysis of synovial fluid. Radiography remains the primary imaging tool in the workup of these conditions; ultra- sound has been playing an increasing role for superficially located crystal-induced ar- thropathies, and computerized tomography (CT) is a nice complement to radiography for deeper sites. When performed in the acute stage, MRI may show severe inflammatory changes that could be misleading; correlation to radiographs or CT should help to distinguish crystal arthropathies from infectious or tumoral conditions. Dual-energy CT is a promising tool for the characterization of crystal arthropathies, partic- ularly gout as it permits a quantitative assessment of deposits, and may help in the follow-up of patients. INTRODUCTION The deposition of microcrystals within and around the joint is a common phenomenon. Intra-articular microcrystals