CONCOMITANT GOUT and RHEUMATOID ARTHRITIS - a CASE Presented with Multiple Nodular Swellings on REPORT Feet, Hands, Wrists and Elbows
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accuracy of Ontario Health Administrative Databases in Identifying Patients with Rheumatoid Arthritis
ACCURACY OF ONTARIO HEALTH ADMINISTRATIVE DATABASES IN IDENTIFYING PATIENTS WITH RHEUMATOID ARTHRITIS by Jessica Widdifield A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy in Health Services Research Institute of Health Policy, Management & Evaluation University of Toronto © Copyright by Jessica Widdifield 2013 Accuracy of Ontario Health Administrative Databases in Identifying Patients with Rheumatoid Arthritis (RA): Creation of the Ontario RA administrative Database (ORAD) Jessica Widdifield Doctor of Philosophy Institute of Health Policy Management and Evaluation University of Toronto 2013 Abstract Rheumatoid arthritis (RA) is a chronic, destructive, inflammatory arthritis that places significant burden on the individual and society. This thesis represents the most comprehensive effort to date to determine the accuracy of administrative data for detecting RA patients; and describes the development and validation of an administrative data algorithm to establish a province-wide RA database. Beginning with a systematic review to guide the conduct of this research, two independent, multicentre, retrospective chart abstraction studies were performed amongst two random samples of patients from rheumatology and primary care family physician practices, respectively. While a diagnosis by a rheumatologist remains the gold standard for establishing a RA diagnosis, the high prevalence of RA in rheumatology clinics can falsely elevate positive predictive values. It was therefore important we also perform a validation study in a primary care setting where prevalence of RA would more closely approximate that observed in the general population. The algorithm of [1 hospitalization RA code] OR [3 physician RA diagnosis codes (claims) with !1 by a specialist in a 2 year period)] demonstrated a ii high degree of accuracy in terms of minimizing both the number of false positives (moderately good PPV; 78%) and true negatives (high specificity: 100%). -

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -
Uncontrolled Gout Fact Sheet
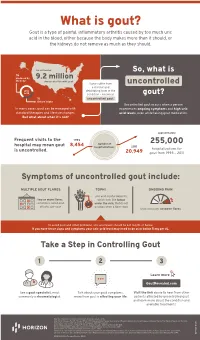
What is gout? Gout is a type of painful, inflammatory arthritis caused by too much uric acid in the blood, either because the body makes more than it should, or the kidneys do not remove as much as they should. An estimated So, what is ⅔ produced by 9.2 million the body Americans live with gout Some suffer from uncontrolled a chronic and uric debilitating form of the acid condition – known as gout? ⅓ uncontrolled gout. dietary intake Uncontrolled gout occurs when a person In many cases, gout can be managed with experiences ongoing symptoms and high uric standard therapies and lifestyle changes. acid levels, even while taking gout medication. But what about when it’s not? approximately Frequent visits to the 1993 number of 255,000 hospital may mean gout 8,454 hospitalizations 2011 is uncontrolled. hospitalizations for 20,949 gout from 1993 – 2011 Symptoms of uncontrolled gout include: MULTIPLE GOUT FLARES TOPHI ONGOING PAIN uric acid crystal deposits, two or more flares, which look like lumps sometimes called gout under the skin, that do not attacks, per year go away when a flare stops that continues between flares To avoid gout and other problems, uric acid levels should be 6.0 mg/dL or below. If you have these signs and symptoms your uric acid level may need to be at or below 5 mg per dL. Take a Step in Controlling Gout 1 2 3 Learn more GoutRevealed.com See a gout specialist, most Talk about your gout symptoms, Visit the link above to hear from other commonly a rheumatologist. -

Rheumatoid Nodules Injected Area Six Times Daily; Nodules Differential Diagnosis and Immunological Appeared in 37 of 82 of Their Patients (450/O)
Matters arising 83 3 Paolaggi J B, Chaouat D, Auquier L. An rheumatic fever, though arthritis or arthralgia but my efforts to reproduce them additional test for the diagnosis and is of a more prolonged nature appearing early experimentally failed miserably! monitoring of giant cell arteritis and after infection. polymyalgia rheumatica. Arth Rheum 1985; F DUDLEY HART Ann Rheum Dis: first published as 10.1136/ard.53.1.83 on 1 January 1994. Downloaded from 28: 837-8. Massell et al' reported in 1937 that nodules 24 Harnnont House, closely resembling those of rheumatic fever 20 Harley Street, could be produced by injecting 3 cc of a London WIN IAN, patient's blood subcutaneously into the soft United Kingdom tissue of an elbow followed by rubbing the 1 Veys E M, De Keyser F. Rheuamtoid nodules: Rheumatoid nodules injected area six times daily; nodules differential diagnosis and immunological appeared in 37 of 82 of their patients (450/o). findings. Ann Rheum Dis 1993; 52: 625-6. 2 Schlesinger B E. The public health aspects of The recent Leader on rheumatoid nodules by I was unable to confirm these findings5 in 40 heart disease in children. Lancet 1938; 1: Veys and De Keyser' gave a very interesting children with rheumatic fever in acute or 593-9, 649-54. and useful review of the subject. When I was convalescent stages, five children with 3 Fink C W. The role of the streptococcus in post- registrar with Dr chronic juvenile arthritis (Still's disease), and streptococcal reactive arthritis in childhood working as a medical polyarteritis nodosa. -

Arthritis (Overview)
ARTHRITIS Having arthritis can significantly affect your comfort & ability to walk and move with confidence. This is because it affects your joints, which are responsible for keeping you steady and moving efficiently. Your symptoms and causes will depend on the type of arthritis that you have. At Masterton Foot Clinic, our podiatrists work closely with patients with four types of arthritis. OSTEOARTHRITIS Osteoarthritis is the wear and tear arthritis that develops slowly over time as the cartilage that covers your bone ends wears down. The cause is largely from natural use over many years, though injuries, alignment issues within the joint and other diseases may result in it developing at a faster rate. We work with patients that want to feel more comfortable on their feet, despite having arthritis in their hip, knee, ankle and foot joints. RHEUMATOID ARTHRITIS Rheumatoid arthritis is an autoimmune disease that affects the joints. It occurs when your body’s immune system attacks the joints and causes damage, inflammation and pain. If the effects of rheumatoid arthritis remain uncontrolled, it can cause permanent changes in the appearance of the joints, especially at the feet and hands. We work with patients to help them manage the discomfort associated with rheumatoid arthritis, offloading prominent and painful areas that have developed due to changes in the joints. GOUT Gout is an inflammatory arthritis that results from a high concentration of uric acid in the blood. It is associated with a high intake of purine-containing foods like red meats, shellfish and red wine, hence it was previously referred to as the rich man’s disease. -

Rheumatoid Nodules Developing Under Methotrexate Treatment for Rheumatoid Arthritis
Letters to the Editor 397 Rheumatoid Nodules Developing under Methotrexate Treatment for Rheumatoid Arthritis Sir, several punched-out radiolucencies and non-calcifying nodules Rheumatoid nodules have been reported to occur in about projecting in the soft parts surrounding the joints. 20% of patients with chronic rheumatoid polyarthritis (1, 2). In the recent literature, a correlation between treatment of rheumatoid arthritis with methotrexate and the development DISCUSSION or worsening of rheumatoid nodules has been suggested (2 ± 4). Methotrexate, a common drug for the treatment of rheuma- We describe here the explosive deterioration of rheumatoid toid arthritis, has been used successfully, but various side- nodules during the course of methotrexate treatment for effects have been reported. Among patients with rheumatoid rheumatoid polyarthritis in a 63-year-old woman and discuss arthritis under methotrexate therapy, the ones whose joint current aspects of possible pathogenetic mechanisms as well symptoms are improving due to administration of metho- as therapeutic options for methotrexate-induced rheumatoid trexate frequently develop subcutaneous nodules increasing in nodules. size and number (1 ± 3, 5). Nevertheless, only in rare cases the severity or the localization of the nodules, e.g. vascular, pulmonary or cardiac manifestation, necessitated discontinua- CASE REPORT tion of the drug (3). Cause and effect relationship between methotrexate treatment and the accelerated development of A 63-year-old woman presented to our department with a 15-year nodules is supported by the regression of the nodules after history of chronic rheumatoid polyarthritis affecting her ®ngers, discontinuation of the drug (2, 6). Although the predominant hand, elbow and knee joints. Ten years previously, she ®rst developed a few ®rm nodules on her ®ngers and feet. -

Complicated Rheumatoid Nodules in Lung
Hindawi Case Reports in Rheumatology Volume 2020, Article ID 6627244, 3 pages https://doi.org/10.1155/2020/6627244 Case Report Complicated Rheumatoid Nodules in Lung Geetha Wickrematilake Sirimavo Bandaranayake Specialized Childrens Hospital, Kandy, Sri Lanka Correspondence should be addressed to Geetha Wickrematilake; [email protected] Received 18 October 2020; Revised 20 November 2020; Accepted 24 November 2020; Published 3 December 2020 Academic Editor: Gregory J. Tsay Copyright © 2020 Geetha Wickrematilake. ,is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. A 65-year-old nonsmoker lady carrying a diagnosis of seropositive erosive rheumatoid arthritis for nine years presented with acute shortness of breath, following a spontaneous pneumothorax while on combination therapy with methotrexate, leflunomide, and tocilizumab. Imaging studies revealed multiple cavitory lung nodules, and a transbronchial lung biopsy favoured a diagnosis of rheumatoid lung nodules. Her initial pathological samples were negative for any infectious cause. A follow-up computerized tomography scan (CT scan) confirmed enlargement of lung nodules with a positive antibody test for aspergillosis which needed antifungal therapy, and currently, her arthritis is managed well with rituximab therapy, sulfasalazine, and hydroxychloroquine. 1. Introduction ,e oxygen saturation was 98% while breathing room air, but -

Actemra® (Tocilizumab) Injection for Intravenous Infusion
UnitedHealthcare® Community Plan Medical Benefit Drug Policy Actemra® (Tocilizumab) Injection for Intravenous Infusion Policy Number: CS2021D0043T Effective Date: September 1, 2021 Instructions for Use Table of Contents Page Commercial Policy Application ..................................................................................... 1 • Actemra® (Tocilizumab) Injection for Intravenous Coverage Rationale ....................................................................... 1 Infusion Applicable Codes .......................................................................... 4 Background.................................................................................. 14 Clinical Evidence ......................................................................... 14 U.S. Food and Drug Administration ........................................... 18 References ................................................................................... 18 Policy History/Revision Information ........................................... 19 Instructions for Use ..................................................................... 19 Application This Medical Benefit Drug Policy does not apply to the states listed below; refer to the state-specific policy/guideline, if noted: State Policy/Guideline Indiana Immunomodulators for Inflammatory Conditions (for Indiana Only) Kansas Refer to the state’s Medicaid clinical policy ® Kentucky Actemra (Tocilizumab) Injection for Intravenous Infusion (for Kentucky Only) Louisiana Refer to the state’s Medicaid clinical -

Gout and Monoarthritis
Gout and Monoarthritis Acute monoarthritis has numerous causes, but most commonly is related to crystals (gout and pseudogout), trauma and infection. Early diagnosis is critical in order to identify and treat septic arthritis, which can lead to rapid joint destruction. Joint aspiration is the gold standard method of diagnosis. For many reasons, managing gout, both acutely and as a chronic disease, is challenging. Registrars need to develop a systematic approach to assessing monoarthritis, and be familiar with the management of gout and other crystal arthropathies. TEACHING AND • Aetiology of acute monoarthritis LEARNING AREAS • Risk factors for gout and septic arthritis • Clinical features and stages of gout • Investigation of monoarthritis (bloods, imaging, synovial fluid analysis) • Joint aspiration techniques • Interpretation of synovial fluid analysis • Management of hyperuricaemia and gout (acute and chronic), including indications and targets for urate-lowering therapy • Adverse effects of medications for gout, including Steven-Johnson syndrome • Indications and pathway for referral PRE- SESSION • Read the AAFP article - Diagnosing Acute Monoarthritis in Adults: A Practical Approach for the Family ACTIVITIES Physician TEACHING TIPS • Monoarthritis may be the first symptom of an inflammatory polyarthritis AND TRAPS • Consider gonococcal infection in younger patients with monoarthritis • Fever may be absent in patients with septic arthritis, and present in gout • Fleeting monoarthritis suggests gonococcal arthritis or rheumatic fever -

Non-Bacterial Thrombotic Endocarditis in a Patient With
Case Report http://dx.doi.org/10.4070/kcj.2016.46.3.425 Print ISSN 1738-5520 • On-line ISSN 1738-5555 Korean Circulation Journal Non-Bacterial Thrombotic Endocarditis in a Patient with Rheumatoid Arthritis Jung-Hye Choi, MD1, Jeong-Eun Park, MD1, Jang-Young Kim, MD2, and Taeyoung Kang, MD1 1Department of Rheumatology, 2Department of Cardiology, Yonsei University Wonju College of Medicine, Wonju, Korea Rheumatoid arthritis (RA) is frequently associated with various extra-joint complications. Although rare, thromboembolic complications are associated with high morbidity and mortality. We experienced a very rare case of nonbacterial thrombotic endocarditis (NBTE) and subsequent embolic stroke in a patient with RA. A 72-year-old male with a 15-year history of RA suddenly developed neurologic symptoms of vomiting and dizziness. Brain magnetic resonance imaging revealed recently developed multiple cerebellar and cerebral lacunar infarctions. Echocardiography showed a pulsating mitral valve vegetation involving the posterior cusp of the mitral valve leaflet, which was confirmed as NBTE. Immediate anti-coagulation therapy was started. The NBTE lesion disappeared in follow-up echocardiography after 4 weeks of anti-coagulation treatment. (Korean Circ J 2016;46(3):425-428) KEY WORDS: Endocarditis, non-infective; Arthritis, rheumatoid; Mitral valve. Introduction of life. Although RA patients have an increased risk of cardiovascular events such as myocardial infarction, stroke, cardiac death and Nonbacterial thrombotic endocarditis (NBTE), a very rare condition thromboembolism compared with the general population,2)3) there that refers to a spectrum of noninfectious endocarditis of the has been no report of mitral valvular NBTE in a patient with RA. -

SUPPLEMENTARY APPENDIX 4: Search Strategies Syntax Guide For
SUPPLEMENTARY APPENDIX 4: Search Strategies Pubmed, Embase Perioperative Management - PubMed Search Strategy – March 6, 2016 Syntax Guide for PubMed [MH] = Medical Subject Heading, also [TW] = Includes all words and numbers in known as MeSH the title, abstract, other abstract, MeSH terms, MeSH Subheadings, Publication Types, Substance Names, Personal Name as Subject, Corporate Author, Secondary Source, Comment/Correction Notes, and Other Terms - typically non-MeSH subject terms (keywords)…assigned by an organization other than NLM [SH] = a Medical Subject Heading [TIAB] = Includes words in the title and subheading, e.g. drug therapy abstracts [MH:NOEXP] = a command to retrieve the results of the Medical Subject Heading specified, but not narrower Medical Subject Heading terms Boolean Operators OR = retrieves results that include at least AND = retrieves results that include all the one of the search terms search terms NOT = excludes the retrieval of terms from the search Perioperative Management PubMed Search Strategy – March 6, 2016 Search Query #1 ((((ARTHROPLASTY, REPLACEMENT, HIP[MH] OR HIP PROSTHES*[TW] OR HIP REPLACEMENT*[TIAB] OR HIP ARTHROPLAST*[TIAB] OR HIP TOTAL REPLACEMENT*[TIAB] OR FEMORAL HEAD PROSTHES*[TIAB]) OR (ARTHROPLASTY, REPLACEMENT, KNEE[MH] OR KNEE PROSTHES*[TW] OR KNEE REPLACEMENT*[TW] OR KNEE ARTHROPLAST*[TW] OR KNEE TOTAL REPLACEMENT*[TIAB]) OR (ARTHROPLAST*[TW] AND (HIP[TIAB] OR HIPS[TIAB] OR KNEE*[TIAB])) AND (("1980/01/01"[PDAT] : "2016/03/06"[PDAT]) AND ENGLISH[LANG])) NOT (((("ADOLESCENT"[MESH]) OR "CHILD"[MESH]) -

19120 Arthritis Aus Gout Booklet
Taking control of your Gout A practical guide to treatments, services and lifestyle choices How can this booklet help you This booklet is designed for people who have gout. It will help you understand your • make healthy choices for your condition so that you can better general health and wellbeing manage your symptoms and continue • find support and additional to lead an active and healthy life. information to cope with the This booklet offers information and impact of gout. practical advice to help you: The information inside is based • understand what gout is and on the latest research and what it means for you recommendations, and has been reviewed by Australian experts in the • understand how medicines can field of arthritis to make sure it is help treat gout attacks and current and relevant to your needs. prevent future attacks So go ahead — take control of • work with your healthcare team your gout! to manage the disease in the short and long term © Copyright Arthritis Australia 2014 Supported by: AstraZeneca Pty Limited ABN 54 009 682 311 Alma Road, North Ryde NSW 2113 2 Taking control of your Gout Contents Understanding gout 4 Treating gout 10 Diet and lifestyle 16 Who can help? 21 Working with your GP 22 Seeing a rheumatologist 23 Other health professionals 24 Seeking support 26 Glossary of terms 28 Useful resources 29 Medical and consumer consultants Tanya deKroo, Information Resources Coordinator, Arthritis Australia Wendy Favorito, Arthritis Australia Consumer Representative and Board Member Assoc Prof Neil McGill, Rheumatologist Assoc Prof Julian McNeil, Rheumatologist and Chair of Australian Rheumatology Association’s Therapeutics Committee Assoc Prof Peter Youssef, Rheumatologist and Chair of Arthritis Australia’s Scientific Advisory Committee Arthritis Australia 3 Understanding gout What is gout? the main reason for more than Gout is an extremely painful form nine out of ten people with gout).