Vaccines Allergy and Asthma Fact Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RNA-Based Adjuvant CV8102 Enhances the Immunogenicity of a Licensed Rabies Vaccine in a first-In-Human Trial
Vaccine 37 (2019) 1819–1826 Contents lists available at ScienceDirect Vaccine journal homepage: www.elsevier.com/locate/vaccine RNA-based adjuvant CV8102 enhances the immunogenicity of a licensed rabies vaccine in a first-in-human trial Fatma Doener a,1, Henoch S. Hong a,1, Ingo Meyer b,1, Keyvan Tadjalli-Mehr c, Angelika Daehling c, ⇑ Regina Heidenreich a, Sven D. Koch a, Mariola Fotin-Mleczek a, Ulrike Gnad-Vogt c, a Curevac AG, Paul-Ehrlich-Strasse 15, 72076 Tübingen, Germany b CRS Clinical Research Services Mönchengladbach GmbH, 41061 Mönchengladbach, Germany c Curevac AG, Schumannstrasse 27, 60325 Frankfurt, Germany article info abstract Article history: Background: We report the first-in-concept human trial of the safety, tolerability and immunogenicity Received 27 September 2018 when a novel TLR 7/8/RIG I agonist RNA-based adjuvant, CV8102, was administered alone or mixed with Received in revised form 30 January 2019 fractional doses of a licensed rabies vaccine (RabipurÒ) as model antigen. Accepted 3 February 2019 Methods: The primary objective was to assess the safety and reactogenicity of various dose levels of Available online 21 February 2019 CV8102 alone or mixed with RabipurÒ in healthy 18–40 year-old male volunteers. A secondary objective was to assess the immune-enhancing potential of bedside-mixes of CV8102 with fractional doses of Keywords: Ò Rabipur by measuring induction of rabies virus neutralising titres (VNTs). Adjuvant Results: Fifty-six volunteers received 50–100 lg CV8102 alone (n = 11), bedside-mixed CV8102 and RNA Ò Ò Ò Rabies Rabipur (n = 20), or Rabipur alone (n = 25; control). -

Food Allergy Outline
Allergy Evaluation-What it all Means & Role of Allergist Sai R. Nimmagadda, M.D.. Associated Allergists and Asthma Specialists Ltd. Clinical Assistant Professor Of Pediatrics Northwestern University Chicago, Illinois Objectives of Presentation • Discuss the different options for allergy evaluation. – Skin tests – Immunocap Testing • Understand the results of Allergy testing in various allergic diseases. • Briefly Understand what an Allergist Does Common Allergic Diseases Seen in the Primary Care Office • Atopic Dermatitis/Eczema • Food Allergy • Allergic Rhinitis • Allergic Asthma • Allergic GI Diseases Factors that Influence Allergies Development and Expression Host Factors Environmental Factors . Genetic Indoor allergens - Atopy Outdoor allergens - Airway hyper Occupational sensitizers responsiveness Tobacco smoke . Gender Air Pollution . Obesity Respiratory Infections Diet © Global Initiative for Asthma Why Perform Allergy Testing? – Confirm Allergens and answer specific questions. • Am I allergic to my dog? • Do I have a milk allergy? • Have I outgrown my allergy? • Do I need medications? • Am I penicillin allergic? • Do I have a bee sting allergy Tests Performed in the Diagnostic Allergy Laboratory • Allergen-specific IgE (over 200 allergen extracts) – Pollen (weeds, grasses, trees), – Epidermal, dust mites, molds, – Foods, – Venoms, – Drugs, – Occupational allergens (e.g., natural rubber latex) • Total Serum IgE (anti-IgE; ABPA) • Multi-allergen screen for IgE antibody Diagnostic Allergy Testing Serological Confirmation of Sensitization History of RAST Testing • RAST (radioallergosorbent test) invented and marketed in 1974 • The suspected allergen is bound to an insoluble material and the patient's serum is added • If the serum contains antibodies to the allergen, those antibodies will bind to the allergen • Radiolabeled anti-human IgE antibody is added where it binds to those IgE antibodies already bound to the insoluble material • The unbound anti-human IgE antibodies are washed away. -

Egg Allergy: the Facts
Egg Allergy: The Facts Egg is a common cause of allergic reactions in infants and young children. It often begins in the child’s first year of life and in some cases lasts into the teenage years – or even into adulthood for a few people. Children who develop allergy to foods such as egg often have other allergic conditions. Eczema and food allergy often occur in early infancy and later on there may be hay-fever, asthma or both. This Factsheet aims to answer some of the questions which you and your family may have about living with egg allergy. Our aim is to provide information that will help you to understand and minimise risks. Even severe cases can be well managed with the right guidance. Many cases of egg allergy are mild, but more severe symptoms are a possibility for some people. If you believe you or your child is allergic to egg, the most important message is to visit your GP and ask for allergy tests and expert advice on management. Throughout this Factsheet you will see brief medical references given in brackets. If you wish to see the full references, please email us at [email protected]. Symptoms triggered by egg The symptoms of a food allergy, including egg allergy, may occur within seconds or minutes of contact with the culprit food. On occasions there may be a delay of more than an hour. Mild symptoms include nettle rash (otherwise known as hives or urticaria) or a tingling or itchy feeling in the mouth. More serious symptoms are uncommon but remain a possibility for some people, including children. -

Genital Allergy C Sonnex
4 Sex Transm Infect: first published as 10.1136/sti.2003.005132 on 30 January 2004. Downloaded from REVIEW Genital allergy C Sonnex ............................................................................................................................... Sex Transm Infect 2004;80:4–7. doi: 10.1136/sti.2003.005132 Genital allergy should be considered as a possible Local responses consist of genital swelling, burning, irritation, or soreness which may occur diagnosis in all patients with genital soreness or irritation during or soon after intercourse, usually becom- for which no infection or dermatosis can be identified and ing maximal at 24 hours and lasting 2–3 days.45 in whom symptoms remain unchanged or worsen with Semen contact with non-genital skin may also give rise to localised itching and urticaria.67 treatment. Type I and IV hypersensitivity reactions are most Generalised reactions associated with semen commonly encountered and can be assessed by allergy include angioedema of the lips and performing skin prick testing/radioallergosorbent test eyelids,68 laryngeal oedema,9 bronchospasm,10 and anaphylaxis347 but, to date, death has not (RAST) or patch testing, respectively. Type IV reactions been reported. Semen allergy mainly affects (contact dermatitis) may sometimes prove difficult to younger women although postmenopausal cases distinguish clinically from an irritant dermatitis. This clinical are documented.11 12 An increasing intensity of reaction with subsequent episodes of coitus is a review attempts to summarise key features of genital common feature. Levine et al described a married allergy for the practising clinician. woman with a 15 year history of hay fever who ........................................................................... initially presented with swollen eyes, nasal congestion, and sneezing an hour after coitus. -

USDA-Approved Animal Rabies Vaccines
United States Department of Agriculture (USDA) Approved Animal Rabies Vaccines Table 1. Rabies Vaccines Licensed and Marketed in the United States, 2016 Age at For use Route of Product Name Produced by Marketed by Dose primary Booster vaccination in inoculation vaccination* A) MONOVALENT (Inactivated) RAB RABVAC 1 Boehringer Boehringer Dogs 1 ml 3 months Annually IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months Annually IM or SC Vetmedica Inc Inc License No. 124 RABVAC 3 Boehringer Boehringer Dogs 1 ml 3 months 1 year later & triennially IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months 1 year later & triennially IM or SC Vetmedica Inc Inc Horses 2 ml 3 months Annually IM License No. 124 EQUIRAB with Merck Animal Merck Animal Health Horses 1 ml 4 months Annually IM Havlogen Health License No. 165A DEFENSOR 1 Zoetis Zoetis Dogs 1 ml 3 months Annually IM or SC License No. 190 Cats 1 ml 3 months Annually SC DEFENSOR 3 Zoetis Zoetis Dogs 1 ml 3 months 1 year later & triennially IM or SC License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM NOBIVAC: 1- Zoetis Merck Animal Health Dogs 1 ml 3 months Annually IM or SC Rabies License No. 190 Cats 1 ml 3 months Annually SC NOBIVAC: 3- Zoetis Merck Animal Health Dogs 1 ml 3 months 1 year later & triennially IM or SC Rabies and 3- License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Rabies CA Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM IMRAB 1 Merial, Inc Merial, Inc Dogs 1 ml 3 months Annually SC License No. -
What You Need to Know
WhatWhat YouYou NeedNeed ToTo KnowKnow 11 inin 1313 childrenchildren That’sThat’s roughlyroughly inin thethe U.S.U.S. hashas 66 millionmillion aa foodfood allergy...allergy... children.children. That'sThat's aboutabout 22 kidskids inin everyevery classroom.classroom. MoreMore thanthan 15%15% ofof schoolschool agedaged childrenchildren withwith foodfood allergiesallergies havehave hadhad aa reactionreaction inin school.school. A food allergy occurs when Food allergy is an IgE-mediated immune the immune system targets a reaction and is not the same as a food food protein and sets off a intolerance or sensitivity. It occurs quickly reaction throughout the body. and can be life-threatening. IgE, or Immunoglobulin E, are antibodies produced by the immune system. IgE antibodies fight allergenic food by releasing chemicals like histamine that trigger symptoms of an allergic reaction. ANTIBODY HISTAMINE Mild Symptoms Severe Symptoms Redness around Swelling of lips, Difficulty Hives mouth or eyes tongue and/or throat swallowing Shortness of Low blood Itchy mouth, Stomach pain breath, wheezing pressure nose or ears or cramps Loss of Chest pain consciousness Nausea or Sneezing Repetitive coughing vomiting AccordingAccording toto thethe CDC,CDC, foodfood allergiesallergies resultresult inin moremore thanthan 300,000300,000 doctordoctor visitsvisits eacheach yearyear amongamong childrenchildren underunder thethe ageage ofof 18.18. Risk Factors Family history Children are at Having asthma or an of asthma or greater risk allergic condition such allergies than adults as hay fever or eczema WhatWhat CanCan YouYou BeBe AllergicAllergic To?To? Up to 4,145,700 people in the U.S. are PEANUTSPEANUTS allergic to peanuts. That’s more than the entire country population 25-40% of Panama! of people who are allergic to peanuts also have reactions to at least one tree nut. -
A Guide to Vaccinations for Parents
A GUIDE TO VACCINATIONS FOR PARENTS What are vaccines? When should my child be vaccinated? Why does my child need the HPV vaccine? HISTORY OF VACCINATIONS Smallpox is a serious infectious disease that causes fever and a distinctive, progressive 600 1796 skin rash. years ago Edward Jenner developed Variolation, intentionally a vaccine against smallpox. Cases of paralysis from polio in the U.S. exposing an individual to Almost 200 years later, in 1980, in the early 1950s: smallpox material, traces back the World Health Organization more than to 16th-century China. This declared that smallpox process resulted in a milder had been eradicated, 15,000 form of the disease. or wiped out. In the year 2017: Childhood vaccines can prevent 14 potentially serious 0 diseases or conditions throughout your child’s lifetime. 1955 1940s 1885 Jonas Salk’s polio vaccine The routine immunization Louis Pasteur developed a was proven safe and effective. schedule included vaccines vaccine against rabies. The Polio has now been eliminated against four potentially serious rabies vaccine series, which in the U.S., and organizations diseases (smallpox, diphtheria, can be given to people who are currently working tetanus, and pertussis). may have been exposed to to eradicate polio Now the schedule includes the virus, has made rabies worldwide. vaccines to prevent a total infection very rare in the of 14 conditions. United States. In the U.S., vaccines go through three phases of clinical trials to make sure they are safe and effective before they are licensed. 2006 Today The HPV vaccine was Vaccine research licensed in the U.S. -

Early Exposure to Egg: Egg Allergy Prevention
Early exposure to egg: egg allergy prevention Intervention Introduction of egg to the diet of infants aged 4–6 months. Indication Infants, particularly those at higher risk of food allergy, with the aim of reducing the risk of developing egg allergy. (See Precautions.) [Hen’s egg allergy is the second most common food allergy Infants who started eating egg between 4 and 6 months of age show a 40% relative in infants and young children risk reduction of egg allergy compared with children who started egg later in life. (cow’s milk is the most common). In terms of absolute risk reduction, in a population where 5.4% of people have egg Most children outgrow egg allergy (ie reported UK prevalence rate), early egg introduction could prevent allergy by adolescence.] 24 cases of egg allergy per 1000 people. The Australasian Society of Clinical Immunology and Allergy recommends introduction of solids (including egg and peanut) for all infants between 4 and 6 months of age. Precautions Infants with a personal history of atopy (particularly moderate-severe eczema) or with a family history of atopy are at high risk of developing allergic disease, including food allergies. These infants may benefit from evaluation by an allergist or a general practitioner trained in management of allergic diseases in this age group to diagnose food allergy and assist in early egg introduction if appropriate. Adverse effects There were no deaths in the studies (which included children at higher risk) and no significant differences in rates of serious adverse events in egg consumption groups and egg avoidance groups. -

Mm7002e1 Allergic Reactions Including Anaphylaxis After Receipt
Morbidity and Mortality Weekly Report Early Release / Vol. 70 January 6, 2021 Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine — United States, December 14–23, 2020 CDC COVID-19 Response Team; Food and Drug Administration As of January 3, 2021, a total of 20,346,372 cases of were determined not to be anaphylaxis, 86 were judged to coronavirus disease 2019 (COVID-19) and 349,246 associ- be nonanaphylaxis allergic reactions, and 61 were considered ated deaths have been reported in the United States. Long- nonallergic adverse events. Seven case reports were still under term sequalae of COVID-19 over the course of a lifetime investigation. This report summarizes the clinical and epide- currently are unknown; however, persistent symptoms and miologic characteristics of case reports of allergic reactions, serious complications are being reported among COVID-19 including anaphylaxis and nonanaphylaxis allergic reactions, survivors, including persons who initially experience a mild after receipt of the first dose of Pfizer-BioNTech COVID-19 acute illness.* On December 11, 2020, the Food and Drug vaccine during December 14–23, 2020, in the United States. Administration (FDA) issued an Emergency Use Authorization CDC has issued updated interim clinical considerations for (EUA) for Pfizer-BioNTech COVID-19 vaccine to prevent use of mRNA COVID-19 vaccines currently authorized in the COVID-19, administered as 2 doses separated by 21 days. On United States (4) and interim considerations for preparing for December 12, 2020, the Advisory Committee on Immunization the potential management of anaphylaxis (5). In addition to Practices (ACIP) issued an interim recommendation for use screening for contraindications and precautions before admin- of Pfizer-BioNTech COVID-19 vaccine (1); initial doses were istering COVID-19 vaccines, vaccine locations should have recommended for health care personnel and long-term care the necessary supplies available to manage anaphylaxis, should facility residents (2). -
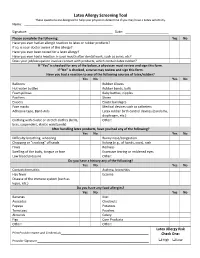
Latex Allergy Screening Tool These Questions Are Designed to Help Your Physician Determine If You May Have a Latex Sensitivity
Latex Allergy Screening Tool These questions are designed to help your physician determine if you may have a Latex sensitivity. Name: ____________________________________ __________ Signature: _________________________________ __________ Date: ______ _______________ Please complete the following: Yes No Have you ever had an allergic reaction to latex or rubber products? If so, is your doctor aware of this allergy? Have you ever been tested for a latex allergy? Have you ever had a reaction in your mouth after dental work, such as sores, etc? Does your job/occupation involve contact with products, which contain latex rubber? If “Yes” is checked for any of the below, a physician must review and sign this form. If “No” is checked, a nurse may review and sign this form. Have you had a reaction to any of the following sources of latex/rubber? Yes No Yes No Balloons Rubber Gloves Hot water bottles Rubber bands, balls Foam pillows Baby bottles, nipples Pacifiers Shoes Erasers Elastic bandages Face masks Medical devices such as catheters Adhesive tape, Band‐Aids Latex rubber birth control devices (condoms, diaphragm, etc.) Clothing with elastic or stretch clothes (belts, Other: bras, suspenders, elastic waistbands) After handling latex products, have you had any of the following? Yes No Yes No Difficulty breathing, wheezing Runny nose/congestion Chapping or “cracking” of hands Itching (e.g., of hands, eyes), rash Hives Redness Swelling of the body, tongue or face Excessive tearing or reddened eyes Low blood pressure Other: Do you have a history any of the following? Yes No Yes No Contact dermatitis Asthma, bronchitis Hay fever Eczema Disease of the immune system (such as lupus, etc.) Do you have any food allergies? Yes No Yes No Bananas Kiwi Avocados Chestnuts Papaya Potatoes Tomatoes Peaches Almonds Celery Figs Corn Products Other: Other: Latex Allergy Risk Print Provider Name and Credentials_________________________________________________ Check One: Provider Signature ______________________________________________________________ High Low . -

BSACI Egg Allergy (PDF)
Egg allergy What is egg allergy? How is egg allergy diagnosed? Egg allergy is caused by an allergic reaction to The diagnosis of egg allergy is based on the egg protein. This protein is found mostly in the history of previous reactions, and can be egg white but also on the yolk. It is common in confirmed by skin tests or blood tests. children under 5 years and usually first noticed in infancy when egg is introduced into the diet What is the treatment? for the first time. It is rare for egg allergy to The best current treatment is to avoid all food develop in adulthood. Those who develop egg containing egg for 1-2 years, allowing the allergy as adults may also be allergic to birds or allergy time to resolve. Egg may be found in a feathers which contain a protein which is similar wide range of foods, including: cakes, pastries, to that found in egg yolk. desserts, meat products, salad dressings, glazes, pasta, battered and bread crumbed What are the symptoms? foods, ice cream, chocolates and sweets. It Most reactions are mild. Commonly infants may also be referred to by unusual terms refuse the egg-containing food, develop especially on imported foods e.g. egg lecithin or redness and sometimes swelling around the albumen (=egg white). The proteins in eggs mouth soon after skin contact and then vomit from other birds are very similar to those in after eating. Stomach ache or diarrhoea may hens’ eggs and should be avoided too. This list also occur. Rarely, some children also develop is not exhaustive and because ingredients can a more severe reaction with cough, an asthma- change food labels must be read carefully type wheeze or even anaphylaxis. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert,