Png Medical Manual Volume 5 Part E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ocean Data Standards
Manuals and Guides 54 Ocean Data Standards Volume 2 Recommendation to Adopt ISO 8601:2004 as the Standard for the Representation of Date and Time in Oceanographic Data Exchange UNESCO Manuals and Guides 54 Ocean Data Standards Volume 2 Recommendation to Adopt ISO 8601:2004 as the Standard for the Representation of Date and Time in Oceanographic Data Exchange UNESCO 2011 IOC Manuals and Guides, 54, Volume 2 Version 1 January 2011 For bibliographic purposes this document should be cited as follows: Paris. Intergovernmental Oceanographic Commission of UNESCO. 2011.Ocean Data Standards, Vol.2: Recommendation to adopt ISO 8601:2004 as the standard for the representation of dates and times in oceanographic data exchange.(IOC Manuals and Guides, 54, Vol. 2.) 17 pp. (English.)(IOC/2011/MG/54-2) © UNESCO 2011 Printed in France IOC Manuals and Guides No. 54 (2) Page (i) TABLE OF CONTENTS page 1. BACKGROUND ......................................................................................................................... 1 2. DATE AND TIME FOR DATA EXCHANGE ......................................................................... 1 3. INTERNATIONAL STANDARD ISO 8601:2004 .............................................................. 1 4. DATE AND TIME REPRESENTATION................................................................................ 2 4.1 Date ................................................................................................................................................. 2 4.2 Time ............................................................................................................................................... -

Islamic Calendar from Wikipedia, the Free Encyclopedia
Islamic calendar From Wikipedia, the free encyclopedia -at اﻟﺘﻘﻮﻳﻢ اﻟﻬﺠﺮي :The Islamic, Muslim, or Hijri calendar (Arabic taqwīm al-hijrī) is a lunar calendar consisting of 12 months in a year of 354 or 355 days. It is used (often alongside the Gregorian calendar) to date events in many Muslim countries. It is also used by Muslims to determine the proper days of Islamic holidays and rituals, such as the annual period of fasting and the proper time for the pilgrimage to Mecca. The Islamic calendar employs the Hijri era whose epoch was Islamic Calendar stamp issued at King retrospectively established as the Islamic New Year of AD 622. During Khaled airport (10 Rajab 1428 / 24 July that year, Muhammad and his followers migrated from Mecca to 2007) Yathrib (now Medina) and established the first Muslim community (ummah), an event commemorated as the Hijra. In the West, dates in this era are usually denoted AH (Latin: Anno Hegirae, "in the year of the Hijra") in parallel with the Christian (AD) and Jewish eras (AM). In Muslim countries, it is also sometimes denoted as H[1] from its Arabic form ( [In English, years prior to the Hijra are reckoned as BH ("Before the Hijra").[2 .(ﻫـ abbreviated , َﺳﻨﺔ ﻫِ ْﺠﺮﻳّﺔ The current Islamic year is 1438 AH. In the Gregorian calendar, 1438 AH runs from approximately 3 October 2016 to 21 September 2017.[3] Contents 1 Months 1.1 Length of months 2 Days of the week 3 History 3.1 Pre-Islamic calendar 3.2 Prohibiting Nasī’ 4 Year numbering 5 Astronomical considerations 6 Theological considerations 7 Astronomical -

Alexander Jones Calendrica I: New Callippic Dates
ALEXANDER JONES CALENDRICA I: NEW CALLIPPIC DATES aus: Zeitschrift für Papyrologie und Epigraphik 129 (2000) 141–158 © Dr. Rudolf Habelt GmbH, Bonn 141 CALENDRICA I: NEW CALLIPPIC DATES 1. Introduction. Callippic dates are familiar to students of Greek chronology, even though up to the present they have been known to occur only in a single source, Ptolemy’s Almagest (c. A.D. 150).1 Ptolemy’s Callippic dates appear in the context of discussions of astronomical observations ranging from the early third century B.C. to the third quarter of the second century B.C. In the present article I will present new attestations of Callippic dates which extend the period of the known use of this system by almost two centuries, into the middle of the first century A.D. I also take the opportunity to attempt a fresh examination of what we can deduce about the Callippic calendar and its history, a topic that has lately been the subject of quite divergent treatments. The distinguishing mark of a Callippic date is the specification of the year by a numbered “period according to Callippus” and a year number within that period. Each Callippic period comprised 76 years, and year 1 of Callippic Period 1 began about midsummer of 330 B.C. It is an obvious, and very reasonable, supposition that this convention for counting years was instituted by Callippus, the fourth- century astronomer whose revisions of Eudoxus’ planetary theory are mentioned by Aristotle in Metaphysics Λ 1073b32–38, and who also is prominent among the authorities cited in astronomical weather calendars (parapegmata).2 The point of the cycles is that 76 years contain exactly four so-called Metonic cycles of 19 years. -
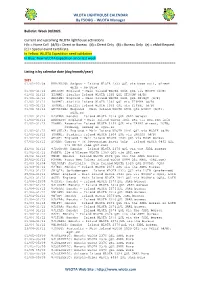
WLOTA LIGHTHOUSE CALENDAR by F5OGG – WLOTA Manager
WLOTA LIGHTHOUSE CALENDAR By F5OGG – WLOTA Manager Bulletin: Week 30/2021 Current and upcoming WLOTA lighthouse activations H/c = Home Call (d/B) = Direct or Bureau (d) = Direct Only (B) = Bureau Only (e) = eMail Request [C] = Special event Certificate In Yellow: WLOTA Expedition need validation In Blue: New WLOTA Expedition since last week ================================================================================== Listing is by calendar date (day/month/year) 2021 01/01-22/08 KH0/KC0W: Saipan – Island WLOTA 1333 QSL via home call, direct only - No Buro 01/01-31/12 GB1OOH: England - Main Island WLOTA 1841 QSL via M0GPN (d/B) 01/01-31/12 II9MMI: Sicilia Island WLOTA 1362 QSL IT9GHW (d/B) 01/01-31/12 GB0LMR: England - Main Island WLOTA 1841 QSL 2E1HQY (d/B) 01/01-31/12 IO9MMI: Sicilia Island WLOTA 1362 QSL via IT9MRM (d/B) 01/01-31/12 IR9MMI: Sicilia Island WLOTA 1362 QSL via IT9YBL (d/B) 01/01-31/12 GB75ISWL: England - Main Island WLOTA 1841 QSL G6XOU (d/B), eQSL.cc 01/01-31/12 8J3ZNJ: Honshu – Island WLOTA 2376 QSL JARL bureau 01/01-31/12 GB80ATC: England - Main Island WLOTA 1841 QSL via QRZ.com info 01/01-31/12 ZD8HZ: Ascension Island WLOTA 1491 QSL via TA1HZ direct, LOTW, ClubLog, HRDLog or eQSL.cc 01/01-31/12 MX1SWL/A: England - Main Island WLOTA 1841 QSL via M5DIK (d/B) 01/01-31/12 IO0MMI: Sardinia Island WLOTA 1608 QSL via IM0SDX (d/B) 01/01-31/12 GB5ST: England - Main Island WLOTA 1841 QSL via RSGB bureau 07/01-31/12 ZC4GR: Cyprus - UK Souvereign Bases Only – Island WLOTA 0892 QSL via EB7DX (see QRZ.com) 23/01-31/12 8J2SUSON: -
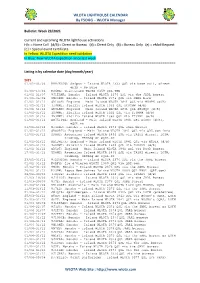
WLOTA LIGHTHOUSE CALENDAR by F5OGG – WLOTA Manager
WLOTA LIGHTHOUSE CALENDAR By F5OGG – WLOTA Manager Bulletin: Week 23/2021 Current and upcoming WLOTA lighthouse activations H/c = Home Call (d/B) = Direct or Bureau (d) = Direct Only (B) = Bureau Only (e) = eMail Request [C] = Special event Certificate In Yellow: WLOTA Expedition need validation In Blue: New WLOTA Expedition since last week ================================================================================== Listing is by calendar date (day/month/year) 2021 01/01-06/06 KH0/KC0W: Saipan – Island WLOTA 1333 QSL via home call, direct only - No Buro 01/01-13/06 KG4MA: Guantanamo WLOTA 0358 QSL TBD 01/01-31/07 8J1TANA: Honshu – Island WLOTA 2376 QSL via the JARL bureau 01/01-06/08 8N2OBU: Honshu – Island WLOTA 2376 QSL via JARL Buro 01/01-31/12 GB1OOH: England - Main Island WLOTA 1841 QSL via M0GPN (d/B) 01/01-31/12 II9MMI: Sicilia Island WLOTA 1362 QSL IT9GHW (d/B) 01/01-31/12 GB0LMR: England - Main Island WLOTA 1841 QSL 2E1HQY (d/B) 01/01-31/12 IO9MMI: Sicilia Island WLOTA 1362 QSL via IT9MRM (d/B) 01/01-31/12 IR9MMI: Sicilia Island WLOTA 1362 QSL via IT9YBL (d/B) 01/01-31/12 GB75ISWL: England - Main Island WLOTA 1841 QSL G6XOU (d/B), eQSL.cc 01/01-31/12 8J3ZNJ: Honshu – Island WLOTA 2376 QSL JARL bureau 01/01-31/12 GB80ATC: England - Main Island WLOTA 1841 QSL via QRZ.com info 01/01-31/12 ZD8HZ: Ascension Island WLOTA 1491 QSL via TA1HZ direct, LOTW, ClubLog, HRDLog or eQSL.cc 01/01-31/12 MX1SWL/A: England - Main Island WLOTA 1841 QSL via M5DIK (d/B) 01/01-31/12 IO0MMI: Sardinia Island WLOTA 1608 QSL via IM0SDX (d/B) 01/01-31/12 -
Feasts and Festivals Around the World Culturally Significant Events
Feasts and Festivals around the World Culturally Significant Events Religiously Significant Dates Eastern Christian Religions Commonly referred to as the “Orthodox” Church – followers in Greece, Russia, Ukraine, Belarus, Bulgaria, Romania, Georgia, Serbia, Armenia, Ethiopia and Egypt. Name Day Celebration – followers celebrate Saints’ Days, after whom a person is named. This may be a more significant day of celebration than birthdays, particularly for 1st generation migrants. Easter usually falls at a different time in the year to the date celebrated by Western Christianity. The Orthodox Churches in Eastern Europe continued to follow the Julian calendar for Easter celebrations, after the Catholic Church adopted the Gregorian calendar in 1582. 2013: 5 May 2014: same date as Western Christianity 20 April 2015: 12 April 2016: 1 May 2017: same date as Western Christianity 16 April 2018: 18 April Christmas may be celebrated on 7 January by those followers of Eastern Christianity known as the “Old Calendarists”, who continue to follow the Julian calendar, and by followers of the Coptic Orthodox Church of Alexandria (Egypt). Islam Communities who identify as Moslem Ramadan: an important annual month-long fast occurring on different dates each year. Although Ramadan is always on the same day of the Islamic (lunar) calendar, the date on the Gregorian (solar) calendar varies from year to year. 2013: 9 July –7 August 2014: 28 June – 27 July 2015: 18 June – 16 July Developed 1997: Ms Lena Dimopoulos, Manager Transcultural Services Eastern Health Last Reviewed: 2013 [email protected] 2016: 6 June – 5 July 2017: 27 May – 25 July 2018: 16 May – 14 June New Year: some Moslems may fast during daylight hours. -

International Standard Iso 8601-1:2019(E)
This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80010314 INTERNATIONAL ISO STANDARD 8601-1 First edition 2019-02 Date and time — Representations for information interchange — Part 1: Basic rules Date et heure — Représentations pour l'échange d'information — Partie 1: Règles de base Reference number ISO 8601-1:2019(E) © ISO 2019 This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80010314 ISO 8601-1:2019(E) COPYRIGHT PROTECTED DOCUMENT © ISO 2019 All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address belowCP 401or ISO’s • Ch. member de Blandonnet body in 8 the country of the requester. ISO copyright office Phone: +41 22 749 01 11 CH-1214 Vernier, Geneva Fax:Website: +41 22www.iso.org 749 09 47 PublishedEmail: [email protected] Switzerland ii © ISO 2019 – All rights reserved This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80010314 ISO 8601-1:2019(E) Contents Page Foreword ..........................................................................................................................................................................................................................................v -

SCO Handbook, Courses & Catalog
DLIELC Directory If You Have Questions About: Contact: Phone / FAX / E-mail • Programming Students POCs on SAN Web_Training_Country Program Manager_DLIELC: Resident • Course Description and Availability • International Resident Flight DSN FAX: (312) 473-4268 • Student Academic Progress (637 ISS/IRF) COMM FAX: (210) 671-4268 • Student Disciplinary Status E-mail: [email protected] DSN: (312) 473-4060 • Protocol • Arranging for DLIELC Visits COMM: (210) 671-4060 (DLIELC/CCP) E-mail: [email protected] DSN: (312) 473-2929 / 2928 / 2927 • International DSN FAX: (312) 473-7437 • Getting to DLIELC from the Support Flight COMM: (210) 671-2929 / 2928 / 2927 San Antonio Airport (637 ISS/ISF) FAX: (210) 671-7437 E-mail: [email protected] • Language Testing: ALCPT, ECL and OPI DSN: (312) 473-4889 • Test Security • English Testing Flight COMM: (210) 671-4889 • Approval of ALCPT Sales (332 TRS/ETF) E-mail: [email protected] E-mail: [email protected] • Arranging Telephonic OPIs • Nonresident English Language Training Programs (ELTPs) DSN: (312) 473-3783 DSN FAX: (312) 473-5362 • DLIELC Advisors/Instructors for • International COMM: (210) 671-3783 Overseas Assignments Nonresident Flight FAX: (210) 671-5362 • ELTP Development Consulting (637 ISS/INF) E-mail: (ALC Materials / Site Surveys) [email protected] • Ordering Materials DSN: (312) 473-4711 DSN FAX: (312) 473-3063 COMM: (210) 671-4711 • Training Logistics Flight • Shipping Orders FAX: (210) 671-3063 (637 TRSS/TLF) E-mail: [email protected] Mailing address for all DLIELC offices: DLIELC/[OFFICE SYMBOL] 2235 ANDREWS AVENUE JBSA-LACKLAND, TX 78236-5259 DLIELC web page: www.dlielc.edu Defense Language Institute English Language Center Defense English Language Program Catalog and Security Cooperation Handbook Since 1954, the Defense Language Institute English Language Center (DLIELC) has performed its mission to support the policies and objectives of the US Government and the US Department of Defense (DoD). -

Shapeshifter – Knowledge of the Moon in Graeco-Roman Egypt
SHAPESHIFTER – KNOWLEDGE OF THE MOON IN GRAECO-ROMAN EGYPT VICTORIA ALTMANN-WENDLING (MUNICH) Introduction Apart from the sun, the moon is the largest and brightest celestial phenomenon as seen from earth. Furthermore, in pre-industrial societies without electric lighting the shifting intensity of nocturnal illumination by the moon played a significantly larger role than today. Hence, it is not astonishing that people used to reflect on the causes and effects of its shift in shape and other associat- ed phenomena. Besides the day-and-night-cycle, the moon’s phases are clearly the most evident means of chronological orientation and therefore lunar-based calendrical systems are quite universal.1 This paper will present the practical application of the lunar phases to the calendar, the regulation of religious festivals, and the temporal organisation of the priests’ services. These indirect pieces of evidence will be further elaborat- ed by Demotic and Greek papyri that contain computations of the moon’s movement and phases. Another topic is the role of the moon in astrology, i.e. how visual phenomena (like eclipses), lunar phases or positions of the moon in the zodiac were used to predict the future. Furthermore, I will also show how the moon and the astronomical phenomena related to it were integrated into the religious imagery and symbolism of ancient Egypt. Since the sources derive mainly from the Graeco-Roman period, during which Egypt was characterised by its multicultural society with increasing contacts to the rest of the Mediter- 1 Cf. NILSSON, 1920, pp. 4f., 15f., 147-239. 213 Victoria Altmann-Wendling ranean and Near Eastern world, reflections on possible exchange, transfer or adoption of knowledge are possible. -

Algol As Horus in the Cairo Calendar 233 Radius Than Algol A
Open Astron. 2018; 27: 232–264 Research Article Sebastian Porceddu*, Lauri Jetsu, Tapio Markkanen, Joonas Lyytinen, Perttu Kajatkari, Jyri Lehtinen, and Jaana Toivari-Viitala Algol as Horus in the Cairo Calendar: the possible means and the motives of the observations https://doi.org/10.1515/astro-2018-0033 Received Feb 15, 2018; accepted May 04, 2018 Abstract: An ancient Egyptian Calendar of Lucky and Unlucky Days, the Cairo Calendar (CC), assigns luck with the period of 2.850 days. Previous astronomical, astrophysical and statistical analyses of CC support the idea that this was the period of the eclipsing binary Algol three millennia ago. However, next to nothing is known about who recorded Algol’s period into CC and especially how. Here, we show that the ancient Egyptian scribes had the possible means and the motives for such astronomical observations. Their principles of describing celestial phenomena as activity of gods reveal why Algol received the title of Horus Keywords: Algol, Horus, ancient Egyptian Astronomy, variable stars, the Cairo Calendar, hemerologies 1 Introduction dated to 1271-1163 B.C. (Bakir 1966, p2-5), (Van Walsem 1982, p233) and (Helck et al. 1975–1992, p156), and pub- lished by Abd el-Mohsen Bakir. As in all our three pre- The ancient Egyptian texts known as the Calendars of vious studies (Porceddu et al. 2008; Jetsu et al. 2013; Lucky and Unlucky Days, or hemerologies, are literary Jetsu and Porceddu 2015), we use only the best preserved works that assign prognoses to each day of the Egyptian continuous calendar which is found on pages recto III- year (Wells 2001a, p117-118), (Leitz 1994, p1-2) (Bacs XXX and verso I-IX of papyrus Cairo 86637. -

The Calendar: Its History, Structure And
!!i\LENDAR jS, HISTORY, STRUCTURE 1 III i; Q^^feiTAA^gvyuLj^^ v^ i Jb^ n n !> f llfelftr I ^'^\C)SL<^ THE CALENDAR BY THE SAME AUTHOR THE IMPROVEMENT OF THE GREGORIAN CALENDAR, WITH NOTES OF AN ADDRESS ON CALENDAR REFORM AND SOCIAL PRO- GRESS DELIVERED TO THE ABERDEEN ROTARY CLUB. 32 pp. Crown 8vo. zs.dd. GEORGE ROUTLEDGE & SONS, Ltd. A PLEA FOR AN ORDERLY ALMANAC. 62 pp. Crown 8vo. Cloth zs. 6d. Stiff boards is. 6d. BRECHIN : D. H. EDWARDS. LONDON : GEORGE ROUTLEDGE & SONS, Ltd. THE CALENDAR ITS HISTORY, STRUCTURE AND IMPROVEMENT BY ALEXANDER PHILIP, LL.B., F.R.S. Edin. CAMBRIDGE AT THE UNIVERSITY PRESS I 9 2 I CAMBRIDGE UNIVERSITY PRESS C. F. Clay, Manager LONDON : FETTER LANE, E.C.4 fij n*'A NEW YORK : THE MACMILLAN CO. BOM HAY ) CALCUTTA I MACMILLAN AND CO., Ltd. MADRAS j TORONTO : THE MACMILLAN CO. OF CANADA, Ltd. TOKYO : MARUZEN-KABUSHIKI-KAISHA ALL RIGHTS RESERVED M u rO(Ku CE 73 f.HS PREFACE THE following essay is intended to serve as a text-book for those interested in current discussion concerning the Calendar. Its design is to exhibit a concise view of the origin and develop- ment of the Calendar now in use in Europe and America, to explain the principles and rules of its construction, to show the human purposes for which it is required and employed and to indicate how far it effectively serves these purposes, where it is deficient and how its deficiencies can be most simply and efficiently amended. After the reform of the Calendar initiated by Pope Gregory XIII there were published a number of exhaustive treatises on the subject—^voluminous tomes characterised by the prolix eru- dition of the seventeenth century. -
About Eritrea and Eritreans…
About Eritrea and Eritreans… Eritrea is Located in N.E. Africa: North of Ethiopia, East of Sudan, On the Red Sea The People: 3.5 million, Mixture of Muslim and Christian; Approved religions are Sunni Muslim; Eritrean Orthodox Christian (the church is controlled by the state), Lutheran and Roman Catholic. Others, such as Jehovah’s Witnesses and Pentecostals are persecuted). Primary Languages: Tigrinya and Arabic. Languages/Ethnic Groups: Tigrinya, Tigre; Kunama; Saho; Afar; Nara; Blein; Hbdrib. With Ethiopia, Eritreans share the only indigenous alphabet in Africa. The Refugees: Thousands flee the country every month because of the malevolent dictatorship in control and: • Unending abusive, intolerant, essentially unpaid military impressment characterized as slave labor. • Lack of basic human rights: freedom to worship, to congregate, etc. • Surveillance; abuse of families of those who flee; arbitrary jailing. • No free speech, no public media; journalists jailed. • No rule of law; arbitrary arrests and imprisonment without charge or trial. • Acute and extensive cruelty, torture and rapacity. Where They Have Fled: Ethiopia (camps in the north & east, and urban), Sudan (camps in the east; urban); Israel (not welcome by govt.); Libya (often trafficked); Yemen; Djibouti; Egypt; South Africa; Uganda; Kenya; Saudi Arabia; S. Sudan; most countries in Europe; USA (via Latin America); Canada. Resettled to various western countries – USA, Canada, Sweden, Norway, Germany, Australia, etc. Many unaccompanied children have fled Eritrea, particularly to Ethiopia. Difficulties Encountered by Eritrean Refugees: • Being shot or captured at the Eritrean border by Eritrean security forces. • Long, unproductive, frustrating lives in camps, often resulting in vulnerability to trafficking. • Limited resettlement opportunities.