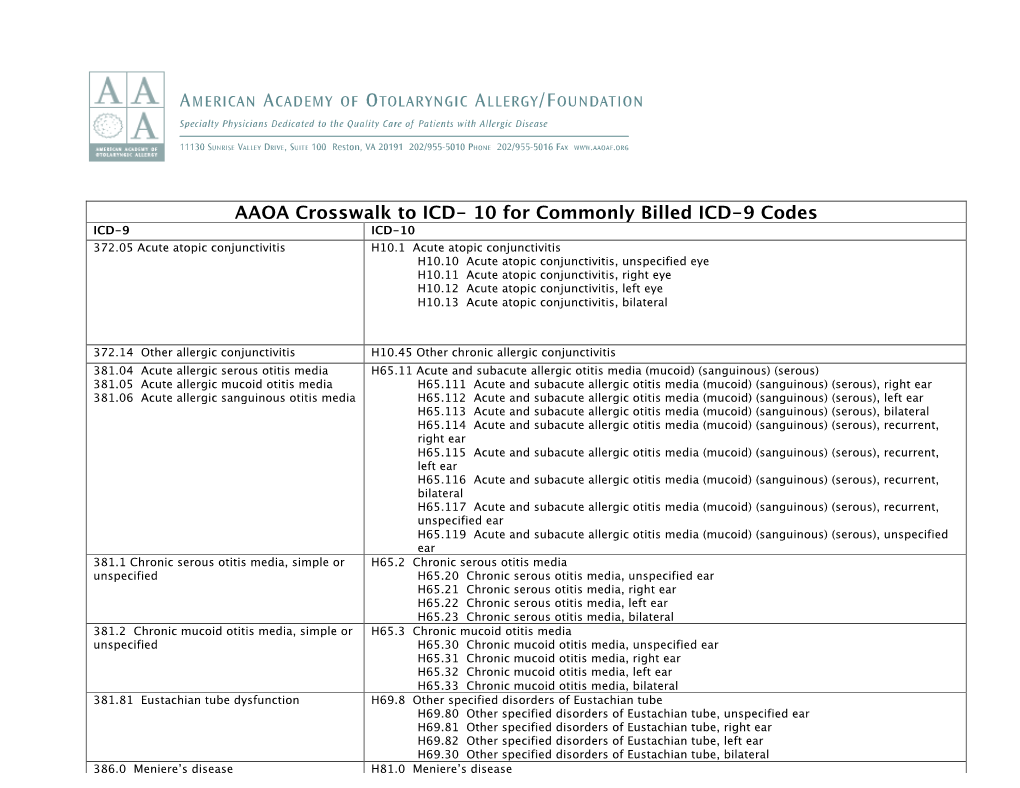
AAOA Crosswalk to ICD- 10 for Commonly Billed ICD-9 Codes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nasal Polyposis, Eosinophil Dominated Inflammation, and Allergy
Thorax 2000;55 (Suppl 2):S79–S83 S79 Nasal polyposis, eosinophil dominated Thorax: first published as 10.1136/thorax.55.suppl_2.S79 on 1 October 2000. Downloaded from inflammation, and allergy Niels Mygind, Ronald Dahl, Claus Bachert A polyp is an oedematous mucous membrane computed tomographic (CT) scanning). The which forms a pedunculating process with a overall prevalence rate is probably about slim or broad stalk or base. Nasal polyps origi- 2–4%5–7 which increases with age of the study nate in the upper part of the nose around the population. Nasal polyposis occurs with a high openings to the ethmoidal sinuses. The polyps frequency in groups of patients with specified extend into the nasal cavity from the middle airway diseases (table 1). meatus, resulting in nasal blockage and re- Although symptomatic nasal polyposis is stricted airflow to the olfactory region. The rare in the general population, much higher polyp stroma is highly oedematous with a vary- figures for the occurrence of isolated nasal ing density of inflammatory cells. Nasal polyps have been obtained from necropsy polyposis, consisting of recurrent, multiple studies. A thorough endoscopic examination of polyps, is part of an inflammatory reaction removed nasoethmoidal blocks and endoscopic involving the mucous membrane of the nose, examination of unselected necropsy specimens paranasal sinuses, and often the lower airways. have shown polyps in as many as 25–40% of The polyps are easily accessible for immuno- specimens.89 logical and histological studies and an increas- Allergic rhinitis has a high prevalence rate of ing number of publications have appeared in about 15–20%.10 Most cases in the western recent years, including two monographs.12 world are caused by pollen allergy, having a Nasal polyps have long been associated with seasonal occurrence. -

Bacterial Tracheitis and the Child with Inspiratory Stridor
Bacterial Tracheitis and the Child With Inspiratory Stridor Thomas Jevon, MD, and Robert L. Blake, Jr, MD Columbia, Missouri Traditionally the presence of inspiratory stridor The child was admitted to the hospital with a and upper respiratory tract disease in a child has presumptive diagnosis of croup and was treated led the primary care physician to consider croup, with mist, hydration, and racemic epinephrine. epiglottitis, and foreign body aspiration in the Initially he improved slightly, but approximately differential diagnosis. The following case demon eight hours after admission he was in marked res strates the importance of considering another piratory distress and had a fever of 39.4° C. At this condition, bacterial tracheitis, in the child with time he had a brief seizure. After this episode his upper airway distress. arterial blood gases on room air were P02 3 8 mmHg and PC02 45 mm Hg, and pH 7.38. Direct laryngos copy was performed, revealing copious purulent Case Report secretions below the chords. This material was A 30-month-old boy with a history of atopic removed by suction, and an endotracheal tube was dermatitis and recurrent otitis media, currently re placed. He was treated with oxygen, frequent suc ceiving trimethoprim-sulfamethoxazole, presented tioning, and intravenous nafcillin and chloramphen to the emergency room late at night with a one-day icol. Culture of the purulent tracheal secretions history of low-grade fever and cough and a three- subsequently grew alpha and gamma streptococci hour history of inspiratory stridor. He was in mod and Hemophilus influenzae resistant to ampicillin. erate to severe respiratory distress with a respira Blood cultures were negative. -

Nasal Polyposis: a Review
Global Journal of Otolaryngology ISSN 2474-7556 Review Article Glob J Otolaryngol - Volume 8 Issue 2 May 2017 Copyright © All rights are reserved by Sushna Maharjan DOI: 10.19080/GJO.2017.0 Nasal Polyposis: A Review Sushna Maharjan1*, Puja Neopane2, Mamata Tiwari1 and Ramesh Parajuli3 1Department of Pathology, Chitwan Medical College Teaching Hospital, Nepal 2Department of Oral Medicine and Pathology, Health Sciences University of Hokkaido, Japan 3Department of Department of Otorhinolaryngology, Chitwan Medical College Teaching Hospital, Nepal Submission: May 07, 2017; Published: May 30, 2017 *Corresponding author: Sushna Maharjan, Department of Pathology, Chitwan Medical College Teaching Hospital (CMC-TH), P.O. Box 42, Bharatpur, Chitwan, Nepal, Email: Abstract Nasal polyp is a benign lesion that arises from the mucosa of the nasal sinuses or from the mucosa of the nasal cavity as a macroscopic usuallyedematous present mass. with The nasalexact obstruction,etiology is still rhinorrhea unknown and and postnasalcontroversial, drip. but Magnetic it is assumed resonance that imagingmain causes is suggested, are inflammatory particularly conditions to rule andout allergy. It is more common in allergic patients with asthma. Interleukin-5 has found to be significantly raised in nasal polyps. The patients seriousKeywords: conditions Allergy; such Interleukin-5; as neoplasia. Nasal Histopathological polyp; Neoplasia examination is also suggested to rule out malignancy and for definite diagnosis. Abbreviations: M:F- Male: Female; IgE: Immunoglobulin E; IL: Interleukin; CRS: Chronic Rhinosinusitis; HLA: Human Leucocyte Antigen; CT: Computerized Tomography; MRI: Magnetic Resonance Imaging Introduction the nose and nasal sinuses characterized by stromal edema and Nasal polyps are characterized by benign lesions that arise from the mucosa of the nasal sinuses, most often from the cause may be different. -

Chest Pain and Non-Respiratory Symptoms in Acute Asthma
Postgrad Med J 2000;76:413–414 413 Chest pain and non-respiratory symptoms in Postgrad Med J: first published as 10.1136/pmj.76.897.413 on 1 July 2000. Downloaded from acute asthma W M Edmondstone Abstract textbooks. Occasionally the combination of The frequency and characteristics of chest dyspnoea and chest pain results in diagnostic pain and non-respiratory symptoms were confusion. This study was prompted by the investigated in patients admitted with observation that a number of patients admitted acute asthma. One hundred patients with with asthmatic chest pain had been suspected a mean admission peak flow rate of 38% of having cardiac ischaemia, pleurisy, pericardi- normal or predicted were interviewed tis, or pulmonary embolism. It had also been using a questionnaire. Chest pain oc- observed that many patients admitted with curred in 76% and was characteristically a asthma complained of a range of non- dull ache or sharp, stabbing pain in the respiratory symptoms, something which has sternal/parasternal or subcostal areas, been noted previously in children1 and in adult worsened by coughing, deep inspiration, asthmatics in outpatients.2 The aim of this or movement and improved by sitting study was to examine the frequency and char- upright. It was rated at or greater than acteristics of chest pain and other symptoms in 5/10 in severity by 67% of the patients. A patients admitted with acute asthma. wide variety of upper respiratory and sys- temic symptoms were described both Patients and methods before and during the attack. One hundred patients (66 females, mean (SD) Non-respiratory symptoms occur com- age 45.0 (19.7) years) admitted with acute monly in the prodrome before asthma asthma were studied. -

Chronic Suppuration in the Nasal Accessory Sinuses and Its Treatment
Hospital Clinics. CHRONIC SUPPURATION IN THE NASAL ACCESSORY SINUSES AND ITS TREATMENT. Two Lectures by "YVm. J. Chichele-Noukse, F.R.C.S.(Edin.), Surgeon to the Central London Throat, Nose, and Ear Hospital; late President of the British Laryngological, Rhinological, and Oto- logical Association. the These lectures were specially reported for during one of the specific fevers, such as typhoid,, columns of The Hospital to illustrate the nature scarlatina, or (especially) influenza. Chronic of the graduate teaching given at this important sinusitis, either the sequel of an unhealed acute been special centre. The notes have very kindly catarrh or, possibly, originating de novo. revised by the lecturer. Simple Empyema: Cystic disease or mucocele, and and tumours. Besides The Grouping of the Sinuses. benign malignant these, the sinuses are liable to be invaded by malig- For clinical purposes, the accessory sinuses of the nant disease or by gummata arising in neighbour- nose may be divided into two groups, according to ing parts, or their bony walls may become necrosed the position of their ostia. The maxillary antrum, or carious. the frontal sinus, and the anterior ethmoidal cells, Chronic Sinusitis. meatus having their ostia opening into the middle The key to the study of diseases of the sinuses is. of the form an anterior The nose, group. chronic sinusitis. To this part of the subject, there- sinus and the ethmoidal sphenoidal posterior cells, fore, as the time is limited, it is proposed to confine opening into the superior meatus, form a posterior the following observations: group. In chronic sinusitis the becomes In each muco-periosteum group the ostia lie very close together. -
Guidelines for Prevention of Healthcare Associated Lower
State of Kuwait Ministry of Health Infection Control Directorate Guidelines for Prevention of Healt Care Associated LRTI Aug. 2006 1 I- Introduction Respiratory tract infections are extremely common health-care associated infections. Lower respiratory tract infection incorporates a spectrum of disease from acute bronchitis to pneumonia. Several factors (age, underlying disease, environment) influence mortality, morbidity and also microbial aetiology especially with the most frequently identified antibiotic resistance of respiratory pathogens. Of the lower respiratory tract infections, pneumonia remains the most common infection seen among hospitalized patients. It is defined as a lower respiratory tract infection occurring > 48 hrs of admission to a hospital or nursing home in a patient who was not incubating the infection on admission. It is the second most common health-care associated infection worldwide after urinary tract infection accounting for 13-18% of all health-care associated infections. Health-care associated pneumonia tends to be more serious because defense mechanisms against infection are often impaired , and the kind of infecting organisms are more dangerous than those generally encountered in the community. It is commonly caused by pathogens that need aggressive diagnostic approach with prompt recognition and urgent treatment to reduce morbidity and mortality; often the strains causing health-care associated pneumonia are multiple. It is complicate up to 1% of all hospitalizations. Critically ill patients who require mechanical ventilation are especially vulnerable to develop ventilator associated pneumonia (VAP). Because of its tremendous risk in the last two decades, most of the research on hospital associated pneumonia has been focused on VAP. As treatment, prognosis and outcome of VAP may differ significantly from other forms of hospital acquired pneumonia, it will be discussed extensively. -

Upper and Lower Respiratory Tract Infections Dr
Upper and Lower Respiratory Tract Infections Dr. Shannon MacPhee IWK Emergency Department April 4, 2014 Declaration of Disclosure • I have no actual or potential conflict of interest in relation to this program. • I also assume responsibility for ensuring the scientific validity, objectivity, and completeness of the content of my presentation. Objectives Stridor Community acquired pneumonia Pathogenesis Clinical presentation and medical workup Treatment Complications: Pleural effusion Bronchiolitis Croup • 15% of all pediatric emergency visits in North America • Abrupt onset • Night • 8% admission rate Croup Laryngotracheobronchitis 6 months to 6 years Parainfluenza (75%) Hoarse voice, Inspiratory stridor, Barky cough Croup radiograph Biennial variation in croup Croup scores No matter which system is used, the presence of retractions and stridor at rest are the two most critical clinical features. Croup treatment Humidified air (not mist!) Dexamethasone Dose and population Budesonide not recommended $$$ Inhaled epinephrine Discharge after 1.5‐3 hours of observation in ER if completely stable Mild croup RCT O.6 mg/kg Follow up on Days 1,2,3,7,21 Detailed analysis of costs for the “payer” (ED visit, Physician billing, med cost) Cost for family (parking, lost work, ambulance service, lost productivity) Average societal cost of $92 versus $72 (Dex versus placeb0) Return visits reduced by more than 50% with dexamethasone arm Dex initial effects within 30 minutes Croup Disposition 1.5‐3 hours post epinephrine Disposition should -

Rhinolith Causing Unilateral Chronic Rhinosinusitis: a Case Report
International Journal of Otorhinolaryngology and Head and Neck Surgery Prinja S et al. Int J Otorhinolaryngol Head Neck Surg. 2020 Feb;6(2):414-417 http://www.ijorl.com pISSN 2454-5929 | eISSN 2454-5937 DOI: http://dx.doi.org/10.18203/issn.2454-5929.ijohns20200163 Case Report Rhinolith causing unilateral chronic rhinosinusitis: a case report Sumit Prinja, Garima Bansal*, Jailal Davessar, Simmi Jindal, Suchina Parmar Department of Otorhinolaryngology, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India Received: 04 November 2019 Accepted: 31 December 2019 *Correspondence: Dr. Garima Bansal, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Rhinolith or nasal stone is formed by mineralization within nasal cavity. They are calcareous concretions that are formed by the deposition of salts on an intranasal foreign body. It is an uncommon disease that may present asymptomatically or cause symptoms like nasal obstruction, consecutive sinusitis with or without purulent rhinitis, post nasal discharge, epistaxis, anosmia, nasal malodour and headache. They are usually diagnosed incidentally on radiographic examinations or depending on the symptoms. In this paper we report a 28-year-old woman admitted in the ENT department of GGS Medical College and Hospital, Faridkot with a calcified mass in the right nasal cavity causing long standing unilateral nasal obstruction for 3 years, rhinorrhoea (usually malodourous foetid), post nasal discharge and headache for 1 year. -

New Medical Treatments for Nasal Polyps
New Medical Treatments for Nasal Polyps February 7, 2020 Brian Modena, MD, MSc 1 Disclosures Research support: NHLBI‐Supported Researcher Self Care Catalysts: architect of Health StorylinesTM app Personal Fees: AstraZeneca, GSK, Regeneron, Sanofi 42nd Annual Pulmonary and Allergy Update Objectives 1. Discuss the epidemiology, biology, pathophysiology, and symptoms of CRS with nasal polyposis (CRSwNP). 2. Review treatment guidelines and recommendations for CRSwNP. 3. Review the many scoring systems used to evaluate CRSwNP. 4. Discuss in detail the Phase II and Phase III clinical trials using biologics for treatment of CRSwNP. Nasal Polyposis Epidemiology Prevalence = ~4%1; (CRS = ~11‐12%)2 Costs: Genetic inheritance = ~14% 2 Increases with age; peak ~50 years CRS = ~$8 billion/year Caucasians = Th2‐driven inflammation. Per patient per year: $13,000; Male to female = 2:1 $26,000 if surgery performed. Asians = Th1‐driven inflammation. Association with allergic rhinitis is weak. Surgeries/year = ~500,000 Disease Prevalence estimates 1. Hastan, Fokkens, et al, 2011 Allergic rhinitis Adult: 0.1%; Children 1.5%1 2. Lange, Holst, et al., Clin Otolaryngol 2013. 3. Mygind. JACI. 1990 Dec;86(6 Pt 1):827‐9. Asthma 5‐22% 4. Schleimer RP. Annu Rev Pathol. 2017;12:331‐57. 5. Hunter TD, DeConde AS, Manes RP. J Med Econ. 2018;21(6):610‐5. CRS 20‐25%1‐4 6. Palmer JN, Messina JC, Biletch R, et al. Allergy Asthma Proc. 2018;39:1‐9. NSAID intolerance 36‐72% 7. Pearlman AN, Chandra RK, Chang D, et al. Am J Rhinol Allergy. 2009;23(2):145‐8. NSAID intolerance and asthma 80% 8. -

Studies on Influenza in the Pandemic of 1957-1958. Ii. Pulmonary Complications of Influenza
STUDIES ON INFLUENZA IN THE PANDEMIC OF 1957-1958. II. PULMONARY COMPLICATIONS OF INFLUENZA Donald B. Louria, … , Edwin D. Kilbourne, David E. Rogers J Clin Invest. 1959;38(1):213-265. https://doi.org/10.1172/JCI103791. Research Article Find the latest version: https://jci.me/103791/pdf STUDIES ON INFLUENZA IN THE PANDEMIC OF 1957-1958. II. PULMONARY COMPLICATIONS OF INFLUENZA * t By DONALD B. LOURIAt HERBERT L. BLUMENFELDt JOHN T. ELLIS, EDWIN D. KILBOURNE, AND DAVID E. ROGERS (From the Departments of Medicine, Pathology, and Public Health and Preventive Medicine, The New York Hospital-Cornell Medical Center, New York, N. Y.) (Submitted for publication July 10, 1958; accepted August 7, 1958) Influenza presents a paradox. To the clinician edge of influenza derived from modern virologic practicing medicine in 1918, influenza was a fear- studies of the epidemic (interpandemic) disease some disease attended by frequent and often fatal must be applied with caution to the 1918-19 pan- pulmonary complications. To the student of in- demic. In the new pandemic in 1957, certain old terpandemic influenza in the last quarter century, questions remained unanswered: the disease is an acute, temporarily incapacitating 1. What is the etiologic agent of pandemic in- infection of the upper respiratory tract which is fluenza? benign except on the rare occasion when bacterial 2. Is the pandemic disease more severe than the pneumonia supervenes. This contrast in the mani- interpandemic form or only more widespread? festations of influenza has led to speculation that 3. Is bacterial pneumonia the major cause of the disease of 1918 was either a different disease fatalities in pandemic influenza; if so, may fatali- entity or caused by an agent of greater virulence ties be prevented by modem antimicrobials? than influenza viruses now encountered. -

Surgical Management of Polyps in the Treatment of Nasal Airway
Surgical Management of Polyps in the TreatmentofNasal Airway Obstruction Samuel S. Becker, MD KEYWORDS FESS Nasal polyps Sinonasal polyps Polyp treatment Nasal obstruction In addition to their role in chronic rhinosinusitis and nasal congestion, sinonasal polyps are associated with significant nasal obstruction. Via a purely mechanical effect (ie, obstruction at its simplest level), polyps alter and otherwise block the normal flow of air through the nose. Similarly, by blocking the drainage pathways of the paranasal sinuses, sinus inflammation and its associated symptom of congestion occur. Because the pathway that leads to the formation of sinonasal polyps has not been completely elucidated, effective long-term treatments remain difficult to pinpoint. Management of these polyps, therefore, is a difficult challenge for the contemporary otolaryngologist. Some of the more common medical treatment options include: topical and oral steroids; macrolide antibiotics; diuretic nasal washes; and intrapolyp steroid injection. Surgical options include polypectomy and functional endoscopic sinus surgery (FESS). In addition, novel treatments for polyps are introduced with some frequency. This article presents an overview of management options for sino- nasal polyps, focusing on the indications, efficacy, and complications of the more common interventions. DIAGNOSIS AND PREVALENCE OF SINONASAL POLYPS Diagnosis of sinonasal polyps relies primarily on nasal endoscopy, with computed tomography (CT) to evaluate the extent of disease. Although unilateral -

Statistical Analysis Plan
Non-Interventional Study Protocol Study Code << DXXXRXXX >> Version V1.4 Date 14 July 2017 Decline In lung-function Among Patients with chronic obstructive Lung disease On maintenance therapy (DIAPLO) An observational study evaluating the benefits of early intervention with maintenance therapies to prevent or slow down rapid lung function decline in patients who are at high risk at the time of COPD diagnosis in the combined Optimum Patient Care Research Database and Clinical Practice Research Datalink databases TITLE PAGE Non-Interventional Study Protocol Study Code << DXXXRXXX >> Version 14 July 2017 Date 14 July 2017 TABLE OF CONTENTS PAGE TITLE PAGE ........................................................................................................... 1 TABLE OF CONTENTS ......................................................................................... 2 LIST OF ABBREVIATIONS .................................................................................. 5 RESPONSIBLE PARTIES ...................................................................................... 6 PROTOCOL SYNOPSIS DIAPLO STUDY ........................................................... 7 AMENDMENT HISTORY ................................................................................... 12 MILESTONES ....................................................................................................... 13 1. BACKGROUND AND RATIONALE .................................................................. 14 1.1 Background ...........................................................................................................