Exogenous Rhinolith: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chronic Suppuration in the Nasal Accessory Sinuses and Its Treatment
Hospital Clinics. CHRONIC SUPPURATION IN THE NASAL ACCESSORY SINUSES AND ITS TREATMENT. Two Lectures by "YVm. J. Chichele-Noukse, F.R.C.S.(Edin.), Surgeon to the Central London Throat, Nose, and Ear Hospital; late President of the British Laryngological, Rhinological, and Oto- logical Association. the These lectures were specially reported for during one of the specific fevers, such as typhoid,, columns of The Hospital to illustrate the nature scarlatina, or (especially) influenza. Chronic of the graduate teaching given at this important sinusitis, either the sequel of an unhealed acute been special centre. The notes have very kindly catarrh or, possibly, originating de novo. revised by the lecturer. Simple Empyema: Cystic disease or mucocele, and and tumours. Besides The Grouping of the Sinuses. benign malignant these, the sinuses are liable to be invaded by malig- For clinical purposes, the accessory sinuses of the nant disease or by gummata arising in neighbour- nose may be divided into two groups, according to ing parts, or their bony walls may become necrosed the position of their ostia. The maxillary antrum, or carious. the frontal sinus, and the anterior ethmoidal cells, Chronic Sinusitis. meatus having their ostia opening into the middle The key to the study of diseases of the sinuses is. of the form an anterior The nose, group. chronic sinusitis. To this part of the subject, there- sinus and the ethmoidal sphenoidal posterior cells, fore, as the time is limited, it is proposed to confine opening into the superior meatus, form a posterior the following observations: group. In chronic sinusitis the becomes In each muco-periosteum group the ostia lie very close together. -

Rhinolith Causing Unilateral Chronic Rhinosinusitis: a Case Report
International Journal of Otorhinolaryngology and Head and Neck Surgery Prinja S et al. Int J Otorhinolaryngol Head Neck Surg. 2020 Feb;6(2):414-417 http://www.ijorl.com pISSN 2454-5929 | eISSN 2454-5937 DOI: http://dx.doi.org/10.18203/issn.2454-5929.ijohns20200163 Case Report Rhinolith causing unilateral chronic rhinosinusitis: a case report Sumit Prinja, Garima Bansal*, Jailal Davessar, Simmi Jindal, Suchina Parmar Department of Otorhinolaryngology, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India Received: 04 November 2019 Accepted: 31 December 2019 *Correspondence: Dr. Garima Bansal, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Rhinolith or nasal stone is formed by mineralization within nasal cavity. They are calcareous concretions that are formed by the deposition of salts on an intranasal foreign body. It is an uncommon disease that may present asymptomatically or cause symptoms like nasal obstruction, consecutive sinusitis with or without purulent rhinitis, post nasal discharge, epistaxis, anosmia, nasal malodour and headache. They are usually diagnosed incidentally on radiographic examinations or depending on the symptoms. In this paper we report a 28-year-old woman admitted in the ENT department of GGS Medical College and Hospital, Faridkot with a calcified mass in the right nasal cavity causing long standing unilateral nasal obstruction for 3 years, rhinorrhoea (usually malodourous foetid), post nasal discharge and headache for 1 year. -

Two Rhinoliths in a Single Nasal Cavity in an Elderly Patient Mimicking Fungal Sinusitis
AIJCR Vishal Prasad et al 10.5005/jp-journals-10013-1201 CASE REPORT Two Rhinoliths in a Single Nasal Cavity in an Elderly Patient Mimicking Fungal Sinusitis 1Vishal Prasad, 2Chandrakala Srinivas, 3Sheetal Krishnappa, 4Suresh T Narayan Rao, 5Harshitha T Rajanna ABSTRACT only about 600 reported cases of rhinoliths. Diagnosis of Objective: To highlight an interesting and a rare case of two rhinolith is often overlooked. They are often diagnosed acci- rhinoliths in a single nasal cavity of an elderly male patient, dently, on routine examination or while treating for other mimicking fungal sinusitis or malignancy. associated conditions like sinusitis. We highlight a rare case To emphasize that rhinolith has to be considered in the diffe- of two rhinoliths seen in an elderly individual with a black rential diagnosis of unilateral nasal mass even in the elderly. necrotic mass protruding through nasal cavity, mimicking Case report: A 55-year-old man presented with a right-sided fungal sinusitis or malignancy. nasal obstruction, foul-smelling nasal discharge and a mass in the right nasal cavity of 6 months duration. Endoscopic examination revealed a gritty, blackish brown mass filling CASE REPORT the entire right nasal cavity. A clinical differential diagnosis of malignancy or fungal sinusitis was made. CT scan of A 55-year-old man presented to the Department of Otorhino- paranasal sinus was suggestive of fungal sinusitis following laryngology with a right-sided nasal obstruction and foul- which patient was posted for biopsy. Intraoperatively, patient smelling nasal discharge since 1 year with a mass protruding was found to have two separate masses in the right nasal from right nasal cavity and facial pain of 6 months duration. -

Rhinolith a Forgotten Entity: Our Experience in Remote Hilly Population of Uttarakhand
International Journal of Otorhinolaryngology and Head and Neck Surgery Bansal C et al. Int J Otorhinolaryngol Head Neck Surg. 2018 Mar;4(2):508-511 http://www.ijorl.com pISSN 2454-5929 | eISSN 2454-5937 DOI: http://dx.doi.org/10.18203/issn.2454-5929.ijohns20180715 Original Research Article Rhinolith a forgotten entity: our experience in remote hilly population of Uttarakhand Chetan Bansal*, V. P. Singh, Deeksha Nautiyal Department of ENT, Shri Guru Ram Rai Institute of Medical Sciences, Dehradun, Uttarakhand, India Received: 27 November 2017 Revised: 07 January 2018 Accepted: 09 January 2018 *Correspondence: Dr. Chetan Bansal, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Rhinoliths are mineralized foreign bodies in the nasal cavity and are diagnosed based on the presenting illness and clinical examination. Giant nasal stones are very rare in occurrence, since improved diagnostic techniques now make it possible to identify foreign bodies at an early stage of disease. The aim of the study was to revisit this rare and forgotten clinical entity with the variations in presentation in the hilly population of uttarakhand and treatment revisited. Methods: We report a case series of 33 patients with rhinoliths who presented to our institute over a period of 10 years, from January 2007 to January 2017. Results: Average age was 25.48 years (range: 5 years to 60 years). -

Fingerprint Biometric System Hygiene and the Risk of COVID-19 Transmission
JMIR BIOMEDICAL ENGINEERING Okereafor et al Viewpoint Fingerprint Biometric System Hygiene and the Risk of COVID-19 Transmission Kenneth Okereafor1*, HND, PGD, BSc, MSc, PhD, PhD; Iniobong Ekong2*, MPH, MBBS; Ini Okon Markson3*, MBBS; Kingsley Enwere1*, BSc 1Department of Information & Communications Technology, National Health Insurance Scheme, Abuja, Nigeria 2Department of Health Planning, Research & Statistics, Federal Capital Territory Health & Human Services Secretariat, Abuja, Nigeria 3Evangelical Church Winning All (ECWA) Comprehensive Medical Centre, Karu, Abuja, Nigeria *all authors contributed equally Corresponding Author: Kenneth Okereafor, HND, PGD, BSc, MSc, PhD, PhD Department of Information & Communications Technology National Health Insurance Scheme NHIS Data Centre Abuja Nigeria Phone: 234 8023148494 Email: [email protected] Abstract Biometric systems use scanners to verify the identity of human beings by measuring the patterns of their behavioral or physiological characteristics. Some biometric systems are contactless and do not require direct touch to perform these measurements; others, such as fingerprint verification systems, require the user to make direct physical contact with the scanner for a specified duration for the biometric pattern of the user to be properly read and measured. This may increase the possibility of contamination with harmful microbial pathogens or of cross-contamination of food and water by subsequent users. Physical contact also increases the likelihood of inoculation of harmful microbial -
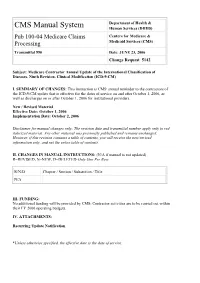
Pub 100-04 Medicare Claims Processing
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Centers for Medicare & Processing Medicaid Services (CMS) Transmittal 990 Date: JUNE 23, 2006 Change Request 5142 Subject: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. SUMMARY OF CHANGES: This instruction is CMS' annual reminder to the contractors of the ICD-9-CM update that is effective for the dates of service on and after October 1, 2006, as well as discharges on or after October 1, 2006 for institutional providers. New / Revised Material Effective Date: October 1, 2006 Implementation Date: October 2, 2006 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D Chapter / Section / Subsection / Title N/A III. FUNDING: No additional funding will be provided by CMS; Contractor activities are to be carried out within their FY 2006 operating budgets. IV. ATTACHMENTS: Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. Attachment – Recurring Update Notification Pub. 100-04 Transmittal: 990 Date: June 23, 2006 Change Request 5142 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. -

JMSCR Vol||08||Issue||09||Page 261-263||September 2020
JMSCR Vol||08||Issue||09||Page 261-263||September 2020 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v8i9.44 Long Forgotten: A Case Report on Twigs Stuffed into Nose of a Twelve Year Old Child Authors Divyanshi Singh1*, Monika Sood2, Neha Thakur3, Sarita Negi4 Department of Otorhinolaryngology, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India *Corresponding Author Divyanshi Singh Abstract Children commonly present with foreign body in nose in the age group of 2-4 years. Long-standing foreign body can go unnoticed in a neglected child or a child with history of abuse or due to the delay in treatment due to fear of pandemic of COVID-19 pandemic amongst patients. We report a case of 12 year old child who presented with chief complaint of foul smelling discharge and swelling on right side of nose. On examination, twigs of pine were visualised which on removal were found to be stuffed till posterior choana. Keywords: COVID-19 Pandemic, Foreign body nose, Neglected child, Child abuse, Nasal discharge, Otorhinolaryngology. Introduction smelling discharge and swelling on right side of Long term home quarantine has led children to nose from past six months. The father of the child explore more using their mouth, nose and ear leading told that the child was apparently well 6 months to an increase in incidence of foreign body ingestion, back when he noticed a swelling on right side of foreign bodies in nose and ear. Child abuse by neglect nose which was gradually progressive and painful. -

Arsat COSM 2015
ARS at COSM 2015 April 23-24, 2015 Hynes Convention Center Sheraton Boston Boston, MA american-rhinologic.org WEB VERSION save the date 4th Annual Summer Sinus Symposium ARS at COSM 2016 July 16-18, 2015 May 19-20, 2016 Westin Michigan Avenue Hyatt Regency Chicago Chicago, Illinois Chicago, Illinois Engage the experts: ask them your questions and debate the answers! • Hear the experts discuss the pearls and pitfalls of managing sinusitis • Watch seasoned surgeons dissect cadavers & answer your questions 5th Annual Summer • Participate in breakout sessions that are geared towards your practice Sinus Symposium • Ancillary Events, Cadaver Workshops and more! July 2016 • Become an ARS Member and enjoy FREE SSS registration! Location: TBD ARS at AAO 61st Annual Meeting September 25-26, 2015 Sheraton Dallas Dallas, Texas find Guest Countries: China • Japan • Korea • Taiwan • Thailand MEMBERSHIP & MEETING 11th Annual David W. Kennedy Lectureship information online at: Guest Speaker: James Stankiewicz, MD "Complications of ESS: 30 Years later" american-rhinologic.org ARS at AAO 62nd Annual Meeting September 16-17, 2016 Manchester Grand Hyatt San Diego San Diego, California American Rhinologic Society • american-rhinologic.org AMERICAN RHINOLOGIC SOCIETY | COSM 2015 Presidential Welcome to the ARS at COSM 2015 On behalf of the Board of Directors, it is my great honor and pleasure to welcome you to the American Rhinologic Society meeting at COSM in Boston! Under the direction of Program Chair, Peter Hwang, MD, and his program committee, we ARS at COSM 2016 Roy Casiano, MD May 19-20, 2016 once again hope to offer an exciting, valuable and enjoyable program. -

STATISTICS " RELATIVE to the FIRST THOUSAND CASES, of DISEASES of the EAR, THROAT and NOSE,Treatel) in the 'FOURTH 'SCOTTISH GENERAL HOSPITAL, STOBHILL, GLASGOW
J R Army Med Corps: first published as 10.1136/jramc-28-05-04 on 1 May 1917. Downloaded from 53~ , I STATISTICS " RELATIVE TO THE FIRST THOUSAND CASES, OF DISEASES OF THE EAR, THROAT AND NOSE,TREATEl) IN THE 'FOURTH 'SCOTTISH GENERAL HOSPITAL, STOBHILL, GLASGOW. \ .' I, \. ' \ • I' By QAPTAIN,A. BROWN KELLY, M,D., D.Se. Roy~l Army Medical, Oorps (Territorial Force), , I THE object of this short paper' is /to show tl:~e freque~cy and nature 6f the diseases of the ear, throat and nose met with in a T. F. General Hqspital, The cases referred to here had all1?een admitted to the hospital. Ih addition, a coqsiderablEi number of outdoor cases were treated, or examined with,'r~ference to pension or discharge from the/ Service: these have not 'b(3en included in the statistics. ' The hospital was opened on August 12, 1914; but no cases came under my,care until September 23. The thousandth 'case ;was seen Protected by copyright. n January 21, 1916. T,he ' p~opo:rtion of oto-rhino-Iaryngological cases to the total admissions to,. the bpspital for the year 1915, during which the 'working conditioJ;1s might be regarded as normal, was as follows:- /, ' , Total admissions . • ; 8,'684 j Cases of ear, nose and throat disease ... 866= 9'97 per cent. '.. ,~ Both totals incl,ude readmisE?ions: . those of ear, throat and nose ,patients amounting to 48. The readmissions to the' hospital' probably 'form aboJt 5 p~r ,cent of the total admissIons, but the,ir exact ,number could be summed' up only with considerable trouble'. -

Huge Rhinolith in Adult
Turkish Archives of Otolaryngology Turk Arch Otolaryngol 2014; 52: 148-50 148 Türk Otolarengoloji Arşivi Huge Rhinolith in Adult Tan Shi Nee1, Salina H2, Primuharsa Putra SHA3 Case Report 1KPJ Healthcare University College, Department of Otorhinolaryngology-Head & Neck Surgery, Kuala Lumpur, Malaysia 2Department of Otorhinolaryngology-Head & Neck Surgery, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia 3Ear, Nose, Throat-Head & Neck Consultant Clinic, KPJ Seremban Specialist Hospital, Seremban, Malaysia Abstract Objective: Rhinoliths in adult are rare and uncom- which a rhinolith was diagnosed. Both cases report mon. incidental findings of huge rhinoliths in the right na- sal cavity. Clinical Presentation and Intervention: We present two cases of rhinoliths in adult. The first case reports Conclusion: Management of the rhinolith and possi- an interesting case of a healthy adult male who pre- sented with symptoms of foul-smelling nasal dis- ble genesis of the rhinolith are discussed. charge and nasal block. The second case report merely shows an adult with the same clinical symptoms in Keywords: Nose, foreign body, adult Introduction and nasal blockage for 6 weeks. It was not asso- Rhinolithiasis is a clinical symptom caused by rhin- ciated with pain and facial swelling. He denied a oliths (1). Today, the incidence of rhinolith in adults history of frequent running nose and blocked nose is low. Rhinoliths result from mineralization of an prior to the onset of the current illness. He also endogenous or exogenous nidus and usually develop denied any history of putting a foreign body inside within the nasal cavity (1). They are a mixture of the nostril during childhood. -

Rhinolithiasis: an Unusual Cause of Nasal Obstruction*
CASE REPORT Rhinology, 40, 162-164, 2002 Rhinolithiasis: an unusual cause of nasal obstruction* Dimitrios Balatsouras1, Panagiotis Eliopoulos2, Antonis Kaberos1, Constantinos Economou1 1 Tzanion General Hospital of Piraeus, Piraeus, Greece 2 General Hospital of Sparti, Sparti, Greece SUMMARY Rhinoliths are foreign bodies of the nose, which may be encountered during the course of a routine examination. If undetected for a long time, they may grow large enough to cause symptoms of nasal obstruction, mimicking sinusitis. We report four patients with rhinoliths presenting with diverse clinical findings. Removal was easy and uneventful in all cases. Key words: rhinolith, nasal obstruction, foreign body, septal perforation. INTRODUCTION remain undetected for many years (Carder and Hiel, 1966), Rhinoliths are uncommon foreign bodies of the nose, which until the rhinoliths grow large enough to cause symptoms of may be encountered accidentally during the course of a rou- nasal obstruction and discharge, leading the unwary physician tine examination (Varley, 1964). Their formation is caused by to the erroneous diagnosis of rhinitis or unresolved sinus in situ calcification of intranasal endogenous or exogenous for- infection (Flood, 1988). eign material (Davis and Wolff, 1985). Rhinoliths are usually Though many reports of cases with rhinoliths appear in the lit- found on the floor of the nasal cavity, about halfway between erature (Appleton et al., 1988), they remain an uncommon the anterior and posterior nares (Appleton et al., 1988). condition in routine clinical practice and may escape attention Rhinolithiasis is often an asymptomatic condition, which may since they are frequently poorly visualized during rhinoscopy. It is therefore important for the practicing rhinologist to be aware of their existence and appearance, so that they are not misdiagnosed for tumors or other pathologic entities (Marano et al., 1970; Levine and Niego, 1972). -

Case Report the Rhinolith—A Possible Differential Diagnosis of a Unilateral Nasal Obstruction
Hindawi Publishing Corporation Case Reports in Medicine Volume 2010, Article ID 845671, 4 pages doi:10.1155/2010/845671 Case Report The Rhinolith—A Possible Differential Diagnosis of a Unilateral Nasal Obstruction Detlef Brehmer1 and Randolf Riemann2 1 Private ENT Clinic Goettingen, Faculty of Medicine, University Witten/Herdecke, Friedrichstraße 3/4, 37073 Goettingen, Germany 2 Department of Otorhinolaryngology, City Hospital Frankfurt-Hoechst, Gotenstr., 6–8, 65929 Frankfurt, Germany Correspondence should be addressed to Detlef Brehmer, [email protected] Received 30 March 2010; Accepted 16 May 2010 Academic Editor: Gerd J. Ridder Copyright © 2010 D. Brehmer and R. Riemann. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Rhinoliths are mineralised foreign bodies in the nasal cavity that are a chance finding at anterior rhinoscopy. Undiscovered, they grow appreciably in size and can cause a foul-smelling nasal discharge and breathing problems. Giant nasal stones are now a very rare occurrence, since improved diagnostic techniques, such as endoscopic/microscopic rhinoscopy, now make it possible to identify foreign bodies at an early stage of development. We report the case of a 37-year-old patient who, at the age of 5-6 years, introduced a foreign body, probably a stone, into his right nasal cavity. On presentation, he complained of difficulty in breathing through the right nostril that had persisted for the last 10 years. For the past four years a strong fetid smell from the nose had been apparent to those in his vicinity.