New Medical Treatments for Nasal Polyps
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nasal Polyposis, Eosinophil Dominated Inflammation, and Allergy
Thorax 2000;55 (Suppl 2):S79–S83 S79 Nasal polyposis, eosinophil dominated Thorax: first published as 10.1136/thorax.55.suppl_2.S79 on 1 October 2000. Downloaded from inflammation, and allergy Niels Mygind, Ronald Dahl, Claus Bachert A polyp is an oedematous mucous membrane computed tomographic (CT) scanning). The which forms a pedunculating process with a overall prevalence rate is probably about slim or broad stalk or base. Nasal polyps origi- 2–4%5–7 which increases with age of the study nate in the upper part of the nose around the population. Nasal polyposis occurs with a high openings to the ethmoidal sinuses. The polyps frequency in groups of patients with specified extend into the nasal cavity from the middle airway diseases (table 1). meatus, resulting in nasal blockage and re- Although symptomatic nasal polyposis is stricted airflow to the olfactory region. The rare in the general population, much higher polyp stroma is highly oedematous with a vary- figures for the occurrence of isolated nasal ing density of inflammatory cells. Nasal polyps have been obtained from necropsy polyposis, consisting of recurrent, multiple studies. A thorough endoscopic examination of polyps, is part of an inflammatory reaction removed nasoethmoidal blocks and endoscopic involving the mucous membrane of the nose, examination of unselected necropsy specimens paranasal sinuses, and often the lower airways. have shown polyps in as many as 25–40% of The polyps are easily accessible for immuno- specimens.89 logical and histological studies and an increas- Allergic rhinitis has a high prevalence rate of ing number of publications have appeared in about 15–20%.10 Most cases in the western recent years, including two monographs.12 world are caused by pollen allergy, having a Nasal polyps have long been associated with seasonal occurrence. -

Bronchiolitis
6 Sand Hill Road, Suite 102 Flemington, NJ 08822 PHONE 908-782-6700 FAX 908-788-5861 hunterdonpediatrics.org BRONCHIOLITIS Bronchiolitis is an infection of the small breathing tubes (bronchioles) that lead to the lung. Bronchiolitis is not the same as bronchitis, which is an infection in the large breathing tubes (bronchi). Bronchiolitis is usually seen in infants and young toddlers. It is not usually seen in older children or adults. A virus causes bronchiolitis. The most common virus is RSV (respiratory syncytial virus). Since RSV infection does not usually result in immunity, people can get it again; however, beyond the age of two, RSV usually causes just a bad cold. RSV is very contagious and spreads rapidly through childcare groups and families from October through April. Some studies suggest that babies who get RSV are more likely to have asthma in the future. Also, people with asthma who get RSV infection may trigger an asthma attack. Babies with RSV have severe nasal congestion, usually followed by a worsening cough. There may be a mild fever at the beginning of the illness. Signs of trouble with RSV include: ● Poor feeding/decreased urine output ● Rapid breathing ● Grunting sound with breathing ● Tightening of chest or stomach muscles with breathing ● Wheezing (high pitched whistling sound with breathing out) ● Blue tint around mouth or fingers/toes ● Fever lasting more than two days, or over 104 The vast majority of patients with bronchiolitis recover well. Certain children are especially likely to have trouble with bronchiolitis: ● Infants under two months of age ● Infants who were premature and have not reached their “due date” yet ● Patients with lung diseases like cystic fibrosis or bronchopulmonary dysplasia (BPD) ● Patients with severe heart disease ● Patients with AIDS or other immunity problems ● Patients on chemotherapy or with organ transplants Treatment for bronchiolitis is mostly supportive; that is, treatment is aimed at helping the patient breathe better. -

The Common Cold.Pdf
PATIENT TEACHING AID The Common Cold PERFORATION ALONG TEAR Everyone has experienced the misery of the common Rhinovirus Infection cold. A cold causes familiar symptoms such as a runny nose, sore throat, congestion, postnasal drip, and cough. For most sufferers, these symptoms are annoying, but not serious. Cold symptoms gradually improve and disappear over 7 to 10 days without complications. Colds are viral infections, so treatment with an antibiotic is not helpful. The best treatment for a cold is rest, fluids, and nonprescription medicines to help relieve symptoms. Although there is no vaccine to prevent colds, the spread of cold viruses can be slowed by frequent hand washing and avoiding close contact with those suffering from a cold. ILLUSTRATION: KRISTEN WIENANDT MARZEJON 2016 MARZEJON WIENANDT KRISTEN ILLUSTRATION: Copyright Jobson Medical Information LLC, 2016 continued MEDICAL PATIENT TEACHING AID Antibiotics Should Not Be Used to Treat a Cold Colds are caused by a variety of viruses, most commonly rhinoviruses. These viruses are highly contagious, and they are spread through the air or when someone is in contact with an infected person or contaminated object. There is no good evidence that exposure to cold or being overheated © Jobson Medical Information LLC, 2016 LLC, Information Medical Jobson © increases the risk of contracting a cold. Although most Wash your hands thoroughly and frequently colds occur in the winter months, some viruses that cause to prevent the spread of cold viruses. colds are more common in the fall or spring. Infants and young children are more prone to colds, as are people with weakened immunity. -

SEPTOPLASTY SURGICAL INFORMED CONSENT the Nasal
.SEPTOPLASTY SURGICAL INFORMED CONSENT The nasal septum is the wall inside your nose that divides it into two separate nasal passages. It is made of cartilage and bone. In a healthy nose, there is usually nearly equal airflow on both sides. Sometimes, the nasal septum is crooked or twisted. This condition is called a deviated nasal septum, and it can be caused by trauma to the nose, or patients can be born this way. The primary problem with a deviated nasal septum is nasal blockage, either on one or both sides. This nasal blockage can also contribute to nosebleeds, sinus infections, and often worsens obstructive sleep apnea. Occasionally, a deviated septum can be associated with a specific type of headache. A deviated septum can be surgically repaired with an operation called a septoplasty. This is typically done through a closed approach, which takes about one hour. More complicated or severely deviated septa may require an open approach, which can take up to 2-3 hours. In either case, septoplasty surgery is done under general anesthesia. It is an outpatient procedure so patients will be discharged home the same day. Some patients have multiple causes of nasal obstruction. Aside from a deviated septum, other reasons for a stuffy nose include chronic sinusitis, turbinate hypertrophy, nasal polyps, or nasal valve collapse. In these cases, septoplasty surgery may be performed in conjunction with other procedures such as endoscopic sinus surgery, turbinate reduction, or insertion of alar batten or spreader grafts. These procedures are discussed in their own individual sections on our website. Your physician will discuss what surgery is most appropriate for you. -

Nasal Polyposis: a Review
Global Journal of Otolaryngology ISSN 2474-7556 Review Article Glob J Otolaryngol - Volume 8 Issue 2 May 2017 Copyright © All rights are reserved by Sushna Maharjan DOI: 10.19080/GJO.2017.0 Nasal Polyposis: A Review Sushna Maharjan1*, Puja Neopane2, Mamata Tiwari1 and Ramesh Parajuli3 1Department of Pathology, Chitwan Medical College Teaching Hospital, Nepal 2Department of Oral Medicine and Pathology, Health Sciences University of Hokkaido, Japan 3Department of Department of Otorhinolaryngology, Chitwan Medical College Teaching Hospital, Nepal Submission: May 07, 2017; Published: May 30, 2017 *Corresponding author: Sushna Maharjan, Department of Pathology, Chitwan Medical College Teaching Hospital (CMC-TH), P.O. Box 42, Bharatpur, Chitwan, Nepal, Email: Abstract Nasal polyp is a benign lesion that arises from the mucosa of the nasal sinuses or from the mucosa of the nasal cavity as a macroscopic usuallyedematous present mass. with The nasalexact obstruction,etiology is still rhinorrhea unknown and and postnasalcontroversial, drip. but Magnetic it is assumed resonance that imagingmain causes is suggested, are inflammatory particularly conditions to rule andout allergy. It is more common in allergic patients with asthma. Interleukin-5 has found to be significantly raised in nasal polyps. The patients seriousKeywords: conditions Allergy; such Interleukin-5; as neoplasia. Nasal Histopathological polyp; Neoplasia examination is also suggested to rule out malignancy and for definite diagnosis. Abbreviations: M:F- Male: Female; IgE: Immunoglobulin E; IL: Interleukin; CRS: Chronic Rhinosinusitis; HLA: Human Leucocyte Antigen; CT: Computerized Tomography; MRI: Magnetic Resonance Imaging Introduction the nose and nasal sinuses characterized by stromal edema and Nasal polyps are characterized by benign lesions that arise from the mucosa of the nasal sinuses, most often from the cause may be different. -

Allergic/Non-Allergic Rhinitis
Tips to Remember: Rhinitis Do you have a runny or stuffy nose that doesn't seem to go away? If so, you may have rhinitis, which is an inflammation of the mucous membranes of the nose. Rhinitis is one of the most common allergic conditions in the United States, affecting about 40 million people. It often coexists with other allergic disorders, such as asthma. It is important to treat rhinitis because it can contribute to other conditions such as sleep disorders, fatigue and learning problems. There are two general types of rhinitis: Allergic rhinitis is caused by substances called allergens. Allergens are often common, usually harmless substances that can cause an allergic reaction in some people. Causes • When allergic rhinitis is caused by common outdoor allergens, such as airborne tree, grass and weed pollens or mold, it is called seasonal allergic rhinitis, or "hay fever." • Allergic rhinitis is also triggered by common indoor allergens, such as animal dander (dried skin flakes and saliva), indoor mold or droppings from cockroaches or dust mites. This is called perennial allergic rhinitis. Symptoms • Sneezing • Congestion • Runny nose • Itchiness in the nose, roof of the mouth, throat, eyes and ears Diagnosis If you have symptoms of allergic rhinitis, an allergist/immunologist can help determine which specific allergens are triggering your reaction. He or she will take a thorough health history, and then test you to determine if you have allergies. Skin tests or Blood (RAST) tests are the most common methods for determining your allergic triggers. Treatment Once your allergic triggers are determined, your physician or nurse will work with you to develop a plan to avoid the allergens that trigger your symptoms. -

Influenza (PDF)
INFLUENZA Outbreaks of influenza, or “flu”, typically occur every winter. Colds may occur at any time of year with seasonal peaks occurring in fall and spring. Influenza is a respiratory illness usually caused by infection with one of two influenza viruses – influenza A or influenza B. Outbreaks of influenza (flu) typically occur every winter. Influenza is characterized by an abrupt onset of fever, chills, headache, body aches, and lack of energy accompanied by respiratory symptoms, most frequently cough and sore throat. Most people are largely recovered in one week, although many feel fatigued for several weeks. Serious complications of flu, such as pneumonia, however, can occur, especially if the body’s defenses are weakened by age or disease. Influenza is spread by inhaling the influenza virus which is usually carried on tiny, invisible water droplets in the air generated by coughs and sneezes. Hand-to-hand contact as well as contact with infected secretions on a hard surface may also cause transmission of the virus. Each year influenza viruses change and new vaccines are made to combat the particular strains that are expected to cause illness that year. The flu vaccine may reduce the chance of getting the flu by 60-80%, and lessen the severity of illness in the person who does get the flu. According to the Centers for Disease Control (CDC), everyone 6 months or order should get a yearly flu vaccine. The following people are at high risk for complications of flu and are especially urged to get vaccinated: Individuals with chronic heart or lung problems that have required regular medical follow-up or hospitalization during the last year. -

Bronchiolitis
Bronchiolitis What is bronchiolitis? Bronchiolitis is a viral infection of the lungs that usually affects infants. There is swelling in the smaller airways or bronchioles of the lung, which causes coughing and wheezing. Bronchiolitis is the most common reason for children under 1 year old to be admitted to the hospital. What are the symptoms of bronchiolitis? The following are the most common symptoms of bronchiolitis. However, each child may experience symptoms differently. Symptoms may include: Runny nose or nasal congestion Fever Cough Changes in breathing patterns (wheezing and breathing faster or harder are common) Decreased appetite Fussiness Vomiting What causes bronchiolitis? Bronchiolitis is a common illness caused by different viruses. The most common virus causing this infection is Respiratory Syncytial Virus (RSV). However, many other viruses can cause bronchiolitis including: Influenza, Parainfluenza, Rhinovirus, Adenovirus, and Human metapneumovirus. Initially, the virus causes an infection in the upper airways, and then spreads downward into the lower airways of the lungs. The virus causes swelling of the airways. Mucus is also produced in the airways. This narrowing of the airways can make it difficult for your child to breath, eat, or nurse. How is bronchiolitis diagnosed? Bronchiolitis is usually diagnosed on the history and physical examination of the child. Antibiotics are not helpful in treating viruses and are not needed to treat bronchiolitis. Because there is no cure for the disease, the goal of treatment is to make your child comfortable and to support their symptoms. This treatment may include suctioning to keep the airways clear, extra oxygen if the blood oxygen levels are low, or hydration if your child is not able to feed well. -

Surgical Management of Polyps in the Treatment of Nasal Airway
Surgical Management of Polyps in the TreatmentofNasal Airway Obstruction Samuel S. Becker, MD KEYWORDS FESS Nasal polyps Sinonasal polyps Polyp treatment Nasal obstruction In addition to their role in chronic rhinosinusitis and nasal congestion, sinonasal polyps are associated with significant nasal obstruction. Via a purely mechanical effect (ie, obstruction at its simplest level), polyps alter and otherwise block the normal flow of air through the nose. Similarly, by blocking the drainage pathways of the paranasal sinuses, sinus inflammation and its associated symptom of congestion occur. Because the pathway that leads to the formation of sinonasal polyps has not been completely elucidated, effective long-term treatments remain difficult to pinpoint. Management of these polyps, therefore, is a difficult challenge for the contemporary otolaryngologist. Some of the more common medical treatment options include: topical and oral steroids; macrolide antibiotics; diuretic nasal washes; and intrapolyp steroid injection. Surgical options include polypectomy and functional endoscopic sinus surgery (FESS). In addition, novel treatments for polyps are introduced with some frequency. This article presents an overview of management options for sino- nasal polyps, focusing on the indications, efficacy, and complications of the more common interventions. DIAGNOSIS AND PREVALENCE OF SINONASAL POLYPS Diagnosis of sinonasal polyps relies primarily on nasal endoscopy, with computed tomography (CT) to evaluate the extent of disease. Although unilateral -
Frequently Asked Questions About Sinusitis Table of Contents
FREQUENTLY ASKED QUESTIONS ABOUT SINUSITIS TABLE OF CONTENTS Chapter 1: Do I have acute sinusitis or chronic sinusitis? 3 Chapter 2: Do I need antibiotics for my acute sinusitis? 4 Chapter 3: What kind of chronic sinusitis do I have? 5 Chapter 4: Why do I have chronic sinusitis? 7 Chapter 5: What are my treatment options for chronic sinusitis? 9 Chapter 6: When should I consider surgery? 11 Chapter 7: Are my allergies causing my chronic sinusitis? 12 Chapter 8: Is there a connection between chronic sinusitis and asthma? 13 Chapter 9: What can I do to keep my chronic sinusitis under control? 14 Chapter 10: About Metropolitan ENT & Facial Plastic Surgery 15 DISCLAIMER: This information is for educational and informational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this e-book. While all attempts have been made to verify information provided in this publication, the Publisher assumes no responsibility for errors, omissions, or contrary interpretation of the subject matter herein. The content of this e-book was developed and published by eos Healthcare Partners, LLC. Accordingly the information and material in this book is copyright, 2015 © eos Healthcare Partners, LLC.Therefore no part of this book may in any form be reproduced, stored, broadcast, sold or transmitted without the prior permission of the publisher, eos Healthcare Partners, LLC. -

Statistical Analysis Plan
Non-Interventional Study Protocol Study Code << DXXXRXXX >> Version V1.4 Date 14 July 2017 Decline In lung-function Among Patients with chronic obstructive Lung disease On maintenance therapy (DIAPLO) An observational study evaluating the benefits of early intervention with maintenance therapies to prevent or slow down rapid lung function decline in patients who are at high risk at the time of COPD diagnosis in the combined Optimum Patient Care Research Database and Clinical Practice Research Datalink databases TITLE PAGE Non-Interventional Study Protocol Study Code << DXXXRXXX >> Version 14 July 2017 Date 14 July 2017 TABLE OF CONTENTS PAGE TITLE PAGE ........................................................................................................... 1 TABLE OF CONTENTS ......................................................................................... 2 LIST OF ABBREVIATIONS .................................................................................. 5 RESPONSIBLE PARTIES ...................................................................................... 6 PROTOCOL SYNOPSIS DIAPLO STUDY ........................................................... 7 AMENDMENT HISTORY ................................................................................... 12 MILESTONES ....................................................................................................... 13 1. BACKGROUND AND RATIONALE .................................................................. 14 1.1 Background ........................................................................................................... -
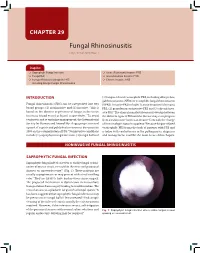
Fungal Rhinosinusitis Eng Cern Gan, Amin R Javer
CHAPTER 29 Fungal Rhinosinusitis Eng Cern Gan, Amin R Javer Snapshot Saprophytic Fungal Infection Acute (Fulminant) Invasive FRS Fungal Ball Granulomatous Invasive FRS Fungus-Related Eosinophilic FRS Chronic Invasive FRS Including Allergic Fungal Rhinosinusitis INTRODUCTION (3) fungus-related eosinophilic FRS, including allergic fun- gal rhinosinusitis (AFRS) or eosinphilic fungal rhinosinusitis Fungal rhinosinusitis (FRS) can be categorized into two (EFRS). Invasive FRS include (1) acute invasive (fulminant) 1 broad groups: (1) noninvasive and (2) invasive. This is FRS, (2) granulomatous invasive FRS and (3) chronic inva- based on the absence or presence of fungus in the tissue sive FRS.3 The clinical manifestations may overlap between (mucosa, blood vessel or bone) respectively.2 To avoid the different types of FRS and the disease may even progress confusion and to optimize management, the International from a noninvasive form to an invasive form with the change Society for Human and Animal Mycology group convened of immunologic status in a patient.4 Because fungus-related a panel of experts and published a consensus document in eosinophilic FRS forms the bulk of patients with FRS and 2009 on the categorization of FRS.3 Noninvasive conditions is laden with controversies in the pathogenesis, diagnosis include (1) saprophytic fungal infection, (2) fungal ball and and management, it will be the main focus of this chapter. NONINVASIVE FUNGAL RHINOSINUSITIS SAPROPHYTIC FUNGAL INFECTION Saprophytic fungal infection refers to visible fungal coloni- zation of mucus crusts seen within the nose and paranasal sinuses on nasoendoscopy3,4 (Fig. 1). These patients are usually asymptomatic or may present with a foul smelling odor.2 They are likely to have had previous sinus surgery.