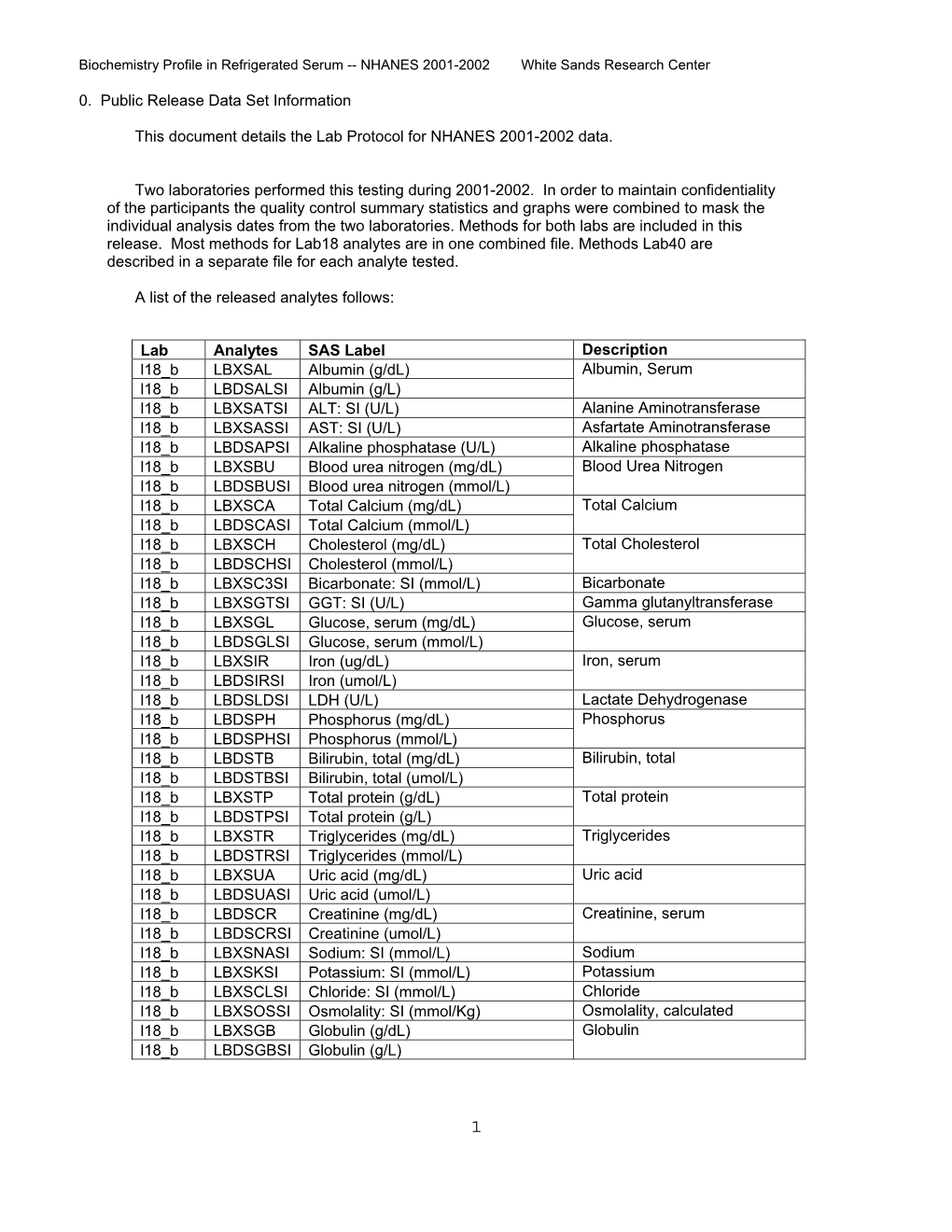
Lab 18 Biochemistry Profile
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thermodynamics and Reaction Mechanism of Urea Decomposition† Cite This: Phys
PCCP View Article Online PAPER View Journal | View Issue Thermodynamics and reaction mechanism of urea decomposition† Cite this: Phys. Chem. Chem. Phys., 2019, 21,16785 a b b b Steffen Tischer, * Marion Bo¨rnhorst, Jonas Amsler, Gu¨nter Schoch and Olaf Deutschmann ab The selective catalytic reduction technique for automotive applications depends on ammonia production from a urea–water solution via thermolysis and hydrolysis. In this process, undesired liquid and solid by-products are formed in the exhaust pipe. The formation and decomposition of these Received 18th March 2019, by-products have been studied by thermogravimetric analysis and differential scanning calorimetry. Accepted 5th July 2019 A new reaction scheme is proposed that emphasizes the role of thermodynamic equilibrium of the DOI: 10.1039/c9cp01529a reactants in liquid and solid phases. Thermodynamic data for triuret have been refined. The observed phenomenon of liquefaction and re-solidification of biuret in the temperature range of 193–230 1Cis rsc.li/pccp explained by formation of a eutectic mixture with urea. Creative Commons Attribution-NonCommercial 3.0 Unported Licence. 1 Introduction and ammonium ISE (ion-selective electrode) measurements. Concluding from experimental results and literature data, 23 Air pollution by nitrogen oxides from Diesel engines is a major possible reactions including urea and its by-products biuret, problem concerning the environment and society. Therefore, cyanuric acid, ammelide, ammeline and melamine are presented. governments follow the need to regulate emissions by law (e.g., Further, cyanate and cyanurate salts and cyanamide are 715/2007/EG, ‘‘Euro 5 and Euro 6’’).1 The favored method to proposed as possible intermediates of high temperature urea reduce nitrogen oxides is selective catalytic reduction (SCR) decomposition. -

United States Patent Office E
Unitede States- Patent- Office 3,845,059E. 1. 2 The reaction of biuret with diethanolamine to form PREPARATION OF N,N'-DIETHANOL3,845,059 PIPERAZINE N,N'-diethanol piperazine can be illustrated as follows: Alvin F. Beale, Jr., Lake Jackson, Tex., assignor to The Dow Chemical Company, Midland, Mich. 2(HOCH)NH -- NH2CONHCONH --> No Drawing. Filed June 19, 1972, Ser. No. 264,704 5 CHO Int, C. C07d51/70 U.S. C. 260-268. SY 8 Claims /N al-woman-mamm CH, CH, ABSTRACT OF THE DISCLOSURE + 2CO. 1 + 8NHat Diethanolamine is reacted with urea or a urea pyrol- lo Y yzate (e.g. biuret, triuret, or cyanuric acid) to form N,N'-diethanol piperazine. The following chart illustrates the balanced stoichiom BACKGROUND OF THE INVENTION la etry for reacting diethanolamine with urea, biuret, triuret, N,N'-diethanol piperazine has been previously prepared and cyanuric acid. Reaction products Moles of Empirical Moles N,N'- Moles of formula of of diethanol Moles Moles (HOCH)NH Name of reactant reactant reactant piperazine of Co2 of NH3 2---------------------- Urea------------------------ CHNO 2 2 4. 2- ---. Biuret---. C2HNO2 2 3 6-- --- Triuret.----- ... C3HNO3 2 3. 6 8 6.----- ... Cyanuric aci - C3H3NO3 2 3. 6 6 by the condensation of piperazine with ethylene chloro- The reaction has been found to be specific for dieth hydrin as reported in J. Am. Chem. Soc., Vol. 55, p. 3823 anolamine since analogous dialkanolamines do not give (1933). The compound has been reported to have phar- corresponding dialkanol-substituted cyclic structures con macological properties as an anesthetic or sedative in 30 taining nitrogens within a carbon ring. -

Asian Journal of Chemistry Asian Journal of Chemistry
Asian Journal of Chemistry; Vol. 27, No. 9 (2015), 3149-3151 ASIAN JOURNAL OF CHEMISTRY http://dx.doi.org/10.14233/ajchem.2015.16726 Synthesis and Antimicrobial Activities of 2-S-Hepta-O-benzoyl lactosyl-1-aryl-5-hepta-O-benzoyl-β-lactosyl-2-isothiobiurets * REENA J. DESHMUKH and SHIRISH P. D ESHMUKH P.G. Department of Chemistry, Shri Shivaji College, Akola-444 001, India *Corresponding author: E-mail: [email protected] Received: 20 April 2014; Accepted: 14 March 2015; Published online: 26 May 2015; AJC-17213 A series of novel 2-S-hepta-O-benzoyl lactosyl-1-aryl-5-hepta-O-benzoyl-β-lactosyl-2-isothiobiurets have been synthesized by the interaction of S-hepta-O-benzoyl lactosyl-1-arylisothiocarbamides and hepta-O-benzoyl-β-D-lactosyl isocyanate. These compounds were screened for their antibacterial and antifungal activities against Escherichia coli, Proteus vulgaris, Salmonella typhimurium, Staphylococcus aureus, Pseudomonas aeruginosa and Aspergillus niger. The newly synthesized compounds have been characterized by analytical and IR, 1H NMR and mass spectral studies. Keywords: Arylisothiocarbamides, Lactosyl thiocyanate, Isothiobiurets. INTRODUCTION an efficient synthetic route to novel lactosyl isothiourea derivatives and their antimicrobial activities are reported. A number of thiourea derivatives have been reported to 1 2 exhibit antibacterial , herbicidal and fungicidal activities. EXPERIMENTAL Sugar thioureas3 has synthetic applications in neoglycocon- jugate synthetic strategies4, including neoglycoproteins5, Melting points determined are uncorrected. IR Spectra glycodendrimers6, glycoclusters7 and pseudooligosaccharides8. were recorded on Perkin-Elmer spectrum RXI FTIR spectro- Thiobiurets (mono and di) are also important derivatives meter. 1H NMR was obtained on Bruker DRX-300 MHz NMR of (thio) urea which may increase the biological activity of Spectrometer. -

Spray Foam Event 2013, Session a Presentations Contents List
Spray Foam Event 2013, Session A Presentations Contents List 1. Introduction to Spray Polyurethane Foam (Click to go to PDF Page 2) 2. OSHA’s Isocyanates National Emphasis Program (Click to go to PDF Page 58) 3. EOLWD On-site Consultation Program (Click to go to PDF Page 76) 4. Essential Resources and Training, American Chemistry Council (Click to go to PDF Page 109) 5. Safe Spray Foam (Click to go to PDF Page 126) 6. EPA Safe Use of Polyurethane Products (Click to go to PDF Page 137) Return to Contents List Introduction to Spray Polyurethane Foam This presentation will provide important background information on SPF, including history, product categories and delivery methods and applications. It will also address chemical concerns and include tips for a quality installation, and briefly cover environmental impacts of the product COPYRIGHTED MATERIALS This presentation is protected by US and International copyright laws. Reproduction, distribution, display and use of any part of this presentation without written permission of the speaker is prohibited. © 2013 Spray Polyurethane Foam Alliance Presentation Content 1. History 2. Product Categories 3. Basic Chemistry 4. Delivery Methods 5. Chemical Concerns 6. Environmental Impact 7. Quality Installation 8. Summary History of SPF in Buildings in construction for 50 years • Late 60’s ‐ Medium Density (agricultural and industrial) • Mid 70’s ‐Roofing ‐ Medium Density (general const.) ‐ Sealants • Mid 90’s ‐ Low Density (residential) Product Category Four general categories of SPF Spray Foam -
Biuret Applications in Beef and Dairy Rations
The Technical Edge Biuret has Practical Applications in Beef and Dairy Rations Feed grade biuret, an economical source of non-protein nitro- gen (NPN), is an ADM Alliance Nutrition® exclusive. It can be Table 1 Nutrient Composition of Biuret used in ruminant diets and is approved for use in dairy lactation Item % AF % DM diets. Prior to May 2003, biuret was not approved for use in dairy DM, % 99 — rations. ADM was instrumental in getting biuret approved for use in dairy rations. Numerous research articles were reviewed and Protein, % 246 248.5 summarized. On May 27, 2003, ADM received an approval letter RDP, % CP 100 100 from the Food and Drug Administration (FDA) allowing biuret to 1 be formulated into dairy rations. SIP , % CP 100 100 Biuret is formed by the controlled decomposition of urea, con- NPN, % SIP 100 100 densing two molecules of urea into a single molecule of biuret, NRC, 2001 A Protein, % CP 100 100 which retains three of the nitrogen atoms (see Figure 1). Feed- 1 grade biuret is a mixture containing biuret and urea (maximum of For use in formulation; biuret is slowly soluble. 14%) with small amounts of triuret and cyanuric acid. Typically, biuret contains a minimum of 35% nitrogen with a crude protein fed in confinement. The slower degradation and physical proper- value of 246% (See Table 1). ties assist in forming a high-quality, self-fed supplement. Biuret Biuret is less soluble than urea. The combination of structural is at least 7.3 times less toxic than urea, making it ideal when and physical characteristics slows the rumen digestion of biuret. -

Attachment A
Attachment A Proposed 15-Day Modifications California Code of Regulations, Title 17, Division 3, Chapter 1, Subchapter 7.7, Article 1 Note: This document shows proposed modifications to the originally proposed amendments to the Regulation for the Reporting of Criteria Air Pollutants and Toxic Air Contaminants, as presented during the November 19, 2020, meeting of the California Air Resources Board. At that meeting, the Board directed staff to make modifications to the proposed amendments based on public comments received, and to provide these updates for public comment for a period of at least 15 days. The pre-existing regulation text is set forth below in normal type. The original proposed amendments are shown in underline formatting to indicate additions and strikeout to indicate deletions. The additional proposed modifications made available with the notice of public availability of modified text dated March XY, 2021, are shown in double- underline to indicate additions and double-strikethrough to indicate deletions. The symbol “***” means that intervening text not proposed for amendment is not shown. Proposed Amendments to the Regulation for the Reporting of Criteria Air Pollutants and Toxic Air Contaminants California Code of Regulations, Title 17, Division 3, Chapter 1, Subchapter 7.7, Articles 1 and 2 Amend Subchapter 7.7, Article 1, and sections 93400, 93401, 93402, 93403, 93404, 93405, 93406, 93407, 93408, 93409, 93410, title 17, California Code of Regulations, and adopt new Subchapter 7.7, Article 2, sections 93420, 93421, and new Subchapter 7.7, Article 2, Appendices A and B to title 17, California Code of Regulations, to read as follows: Subchapter 7.7: Regulation for the Reporting of Criteria Air Pollutants and Toxic Air Contaminants Article 1. -

United States Patent Office Patented Feb
3,367,956 United States Patent Office Patented Feb. 6, 1968 1 2 3,367,956 or cycloaliphatic hydrocarbons. When following the pro PREPARATION OF BIURET POLYISOCYANATES cedure of the present invention, it is critical to elevate Hans Joachim Hennig, Cologne-Starnmheim, and Otto the temperature at least in the later stage of the reaction Bayer, Erwin Windemuth, and Wilhelm Bunge, Lever ' to about ISO-250° C. to bring about formation of mono kusen, Germany, assignors to Farhenfabriken Bayer isocyanate which must be continuously removed substan Aktiengesellschaft, Leverkusen, Germany, a German corporation tially as soon as it is formed, preferably by operating at N0 Drawing. Filed Apr. 1, 1964, Ser. No. 356,650 the elevated temperature at a reduced pressure or by Claims priority, application Germany, Apr. 13, 1963, using a carrier gas to remove the organic monoisocyanate F 39,482 from the reaction mixture substantially as soon as it is 6 Claims. (Cl. 260—453) formed. Then the well-de?ned biuret polyisocyanates of the invention are formed instead of high molecular weight This invention relates to organic polyisocyanates and condensation products. Thus, it is an essential feature of more particularly to a process for the preparation of this invention to carry out the process under such tem biuret polyisocyanates. Moreover, this invention provides perature conditions that a monoisocyanate is split off and a new and unexpected way of preparing biuret polyiso the reactants may recombine to form a biuret polyiso cyanates which may also contain carbamyl groups with cyanate. Instead of high molecular weight condensation out the formation of undesirable by-products. -

Risk-Based Closure Guide Draft
Risk-based Closure Guide July 1, 2021 Office of Land Quality Indiana Department of Environmental Management Disclaimer This Nonrule Policy Document (NPD) is being established by the Indiana Department of Environmental Management (IDEM) consistent with its authority under IC 13-14-1-11.5. It is intended solely as guidance and shall be used in conjunction with applicable rules or laws. It does not replace applicable rules or laws, and if it conflicts with these rules or laws, the rules or laws shall control. Pursuant to IC 13-14-1-11.5, this NPD will be available for public inspection for at least forty-five (45) days prior to presentation to the appropriate State Environmental Board, and may be put into effect by IDEM thirty (30) days afterward. If the NPD is presented to more than one board, it will be effective thirty (30) days after presentation to the last State Environmental Board. IDEM also will submit the NPD to the Indiana Register for publication. 2 Table of Contents 1 Introduction ..................................................................................................................................... 7 1.1 Applicability .............................................................................................................................. 8 1.2 Types of Closure ...................................................................................................................... 9 1.3 Process Overview ................................................................................................................... -

NMR Analysis to Identify Biuret Groups in Common Polyureas
Chinese Journal of POLYMER SCIENCE ARTICLE https://doi.org/10.1007/s10118-018-2130-y Chinese J. Polym. Sci. 2018, 36, 1150–1156 NMR Analysis to Identify Biuret Groups in Common Polyureas Wei-Guang Qiu, Fei-Long Zhang, Xu-Bao Jiang*, and Xiang-Zheng Kong* College of Chemistry and Chemical Engineering, University of Jinan, Jinan 250022, China Abstract Polyureas (PU) are well known as a class of high impact engineering materials, and widely used also in emerging advanced applications. As a general observation, most of them are only soluble in a very limited number of highly protonic solvents, which makes their chemical structure analysis a great challenge. Besides the presence of abundant hydrogen bonding, the poor solubility of PU in common organic solvents is often ascribed to the formation of biuret crosslinking in their molecular chains. To clarify the presence of biuret groups in PU has been of great interest. To this end, two samples, based on hexamethylene diisocyanate (HDI) and toluene diisocyanate (TDI) respectively, were synthesized by precipitation polymerization of each of these diisocyanates in water-acetone at 30 °C. Their chemical structures were analyzed by high resolution magic angle spinning (HR-MAS) NMR, and through comparison of their NMR spectra with those of specially prepared biuret-containing polyurea oligomers, it was concluded that biuret group was absent in all the PU prepared at 30 °C. In addition, this NMR analysis was also applied to a PU obtained by copolymerization of TDI with ethylene diamine (EDA) and water at 65 °C in EDA aqueous solution. It was confirmed that biuret unit was also absent in this PU and that EDA was more active than water towards TDI. -

Chemicals Subject to TSCA Section 12(B) Export Notification Requirements (January 16, 2020)
Chemicals Subject to TSCA Section 12(b) Export Notification Requirements (January 16, 2020) All of the chemical substances appearing on this list are subject to the Toxic Substances Control Act (TSCA) section 12(b) export notification requirements delineated at 40 CFR part 707, subpart D. The chemicals in the following tables are listed under three (3) sections: Substances to be reported by Notification Name; Substances to be reported by Mixture and Notification Name; and Category Tables. TSCA Regulatory Actions Triggering Section 12(b) Export Notification TSCA section 12(b) requires any person who exports or intends to export a chemical substance or mixture to notify the Environmental Protection Agency (EPA) of such exportation if any of the following actions have been taken under TSCA with respect to that chemical substance or mixture: (1) data are required under section 4 or 5(b), (2) an order has been issued under section 5, (3) a rule has been proposed or promulgated under section 5 or 6, or (4) an action is pending, or relief has been granted under section 5 or 7. Other Section 12(b) Export Notification Considerations The following additional provisions are included in the Agency's regulations implementing section 12(b) of TSCA (i.e. 40 CFR part 707, subpart D): (a) No notice of export will be required for articles, except PCB articles, unless the Agency so requires in the context of individual section 5, 6, or 7 actions. (b) Any person who exports or intends to export polychlorinated biphenyls (PCBs) or PCB articles, for any purpose other than disposal, shall notify EPA of such intent or exportation under section 12(b). -

WO 2013/109674 Al 25 July 2013 (25.07.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2013/109674 Al 25 July 2013 (25.07.2013) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C03C 17/30 (2006.01) B44C 1/00 (2006.01) kind of national protection available): AE, AG, AL, AM, C03C 21/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, (21) Number: International Application DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2013/021815 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 17 January 2013 (17.01 .2013) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, (25) Filing Language: English RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (26) Publication Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 12305068.4 19 January 2012 (19.01.2012) EP (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: CORNING INCORPORATED [US/US]; 1 GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, Riverfront Plaza, Corning, New York 1483 1 (US). -
Delineating Pmdi Model Reactions with Loblolly Pine Via Solution-State NMR Spectroscopy
Article in press - uncorrected proof Holzforschung, Vol. 65, pp. 145–154, 2011 • Copyright ᮊ by Walter de Gruyter • Berlin • New York. DOI 10.1515/HF.2011.029 Delineating pMDI model reactions with loblolly pine via solution-state NMR spectroscopy. Part 2. Non-catalyzed reactions with the wood cell wall Daniel J. Yelle1,*, John Ralph2 and Charles Introduction R. Frihart1 1 U.S. Forest Products Laboratory, U.S.D.A. Forest Service, Polymeric methylene diphenyl diisocyanate (pMDI) adhe- Madison, WI, USA sive, applied in oriented strand-board (OSB), laminated 2 Department of Biochemistry (Enzyme Institute) and strand-lumber and exterior particleboard production has been D.O.E. Great Lakes Bioenergy Research Center, touted as the only adhesive that can chemically react with University of Wisconsin-Madison, Madison, WI, USA cell wall polymers since its introduction in the early 1970s *Corresponding author. (Deppe and Ernst 1971; Deppe 1977; Frisch et al. 1983). U.S. Forest Products Laboratory, One Gifford Pinchot Indeed, isocyanate adhesives have been shown to create Drive, Madison, WI 53726, USA durable bonds with wood, thus withstanding swelling and q Phone: 1-608-231-9359 shrinkage stresses at the bondline interface (Frazier 2003). Fax: q1-608-231-9592 E-mail: [email protected] To date, however, there is a lack in understanding of why these adhesives bond well to wood while others do not. Moreover, it is not clear whether covalent bonds are neces- sary for durable wood adhesion. To better formulate an Abstract adhesive with high bondline durability, the molecular char- acteristics of the interaction between the adhesive and wood Solution-state NMR provides a powerful tool to observe the should be better understood (Yelle 2009).