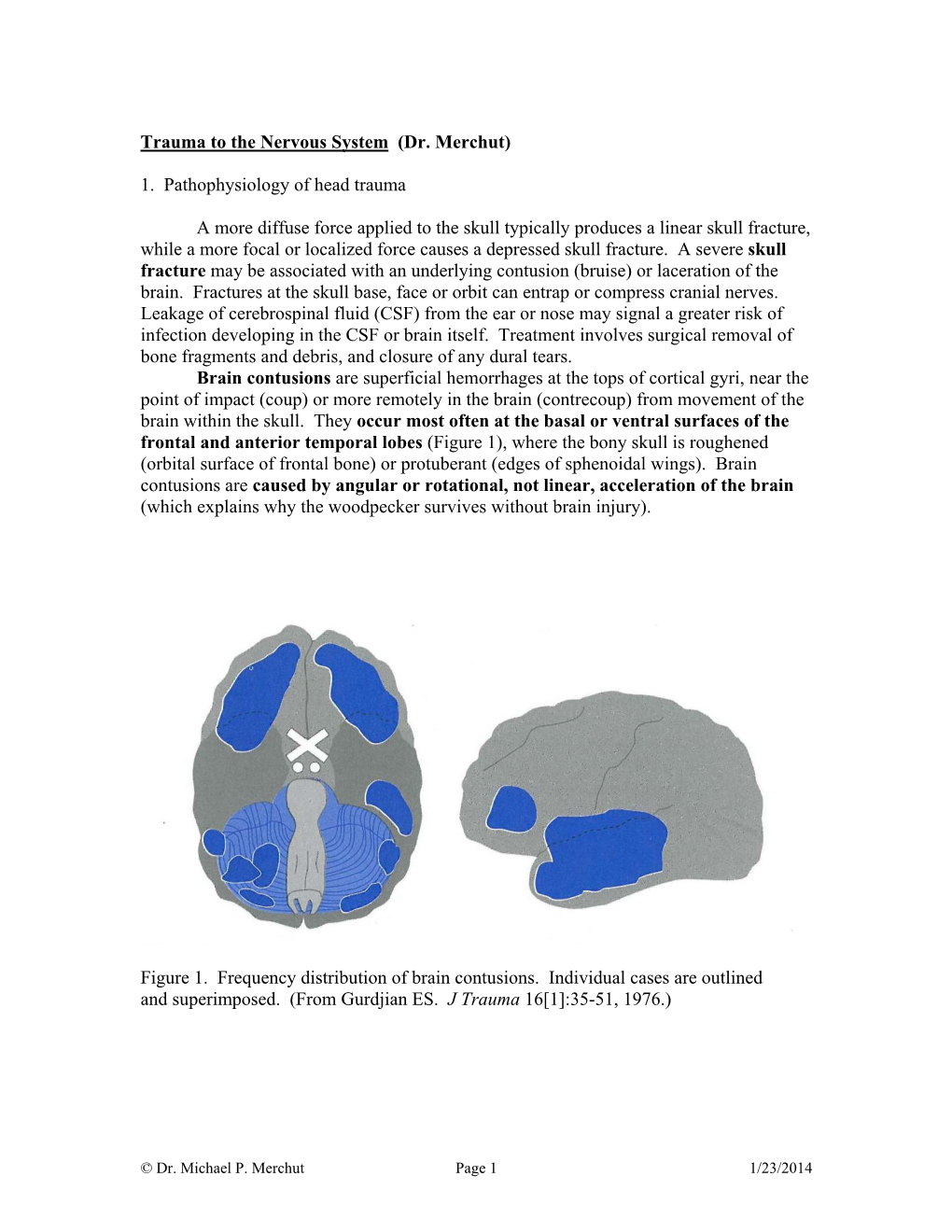
Trauma to the Nervous System (Dr. Merchut) 1. Pathophysiology Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Do Bridging Veins Rupture Into the Virtual Subdural Space?
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.47.2.121 on 1 February 1984. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1984;47:121-127 Why do bridging veins rupture into the virtual subdural space? T YAMASHIMA, RL FRIEDE From the Department ofNeuropathology, University of Gottingen, Gottingen, Federal Republic of Germany SUMMARY Electron microscopic data on human bridging veins show thin walls of variable thick- ness, circumferential arrangement of collagen fibres and a lack of outer reinforcement by arach- noid trabecules, all contributory to the subdural portion of the vein being more fragile than its subarachnoid portion. These features explain the laceration of veins and the subdural location of resultant haematomas. Most subdural haematomas due to venous bleeding walls are delicate, lacking muscle fibres, with only a have been attributed to lacerations in bridging veins. thin fibrous wall and a thin elastic lamina adjacent to These veins form short trunks passing directly from the endothelial layer. The conclusions of these two the brain to the dura mater, almost at right angles to authors, have gained wide acceptance, although guest. Protected by copyright. both. Between these two points, bridging veins take there was little evidence concerning the fragility of a straight course with no tortuosity to allow for the the vein walls. possible displacement of brain.' Trotter2 speculated The purpose of the present communication is to that subdural haematomas are invariably due to provide electron microscopic data on tissue fixed in trauma tearing large veins, an interpretation situ, which might throw some light on to the lacera- elaborated by Krauland.3 According to Leary,4 the tion mechanism of bridging veins and its relationship common sources of subdural haematomas are rup- to the development of subdural haematoma. -

Management of the Head Injury Patient
Management of the Head Injury Patient William Schecter, MD Epidemilogy • 1.6 million head injury patients in the U.S. annually • 250,000 head injury hospital admissions annually • 60,000 deaths • 70-90,000 permanent disability • Estimated cost: $100 billion per year Causes of Brain Injury • Motor Vehicle Accidents • Falls • Anoxic Encephalopathy • Penetrating Trauma • Air Embolus after blast injury • Ischemia • Intracerebral hemorrhage from Htn/aneurysm • Infection • tumor Brain Injury • Primary Brain Injury • Secondary Brain Injury Primary Brain Injury • Focal Brain Injury – Skull Fracture – Epidural Hematoma – Subdural Hematoma – Subarachnoid Hemorrhage – Intracerebral Hematorma – Cerebral Contusion • Diffuse Axonal Injury Fracture at the Base of the Skull Battle’s Sign • Periorbital Hematoma • Battle’s Sign • CSF Rhinorhea • CSF Otorrhea • Hemotympanum • Possible cranial nerve palsy http://health.allrefer.com/pictures-images/ Fracture of maxillary sinus causing CSF Rhinorrhea battles-sign-behind-the-ear.html Skull Fractures Non-depressed vs Depressed Open vs Closed Linear vs Egg Shell Linear and Depressed Normal Depressed http://www.emedicine.com/med/topic2894.htm Temporal Bone Fracture http://www.vh.org/adult/provider/anatomy/ http://www.bartleby.com/107/illus510.html AnatomicVariants/Cardiovascular/Images0300/0386.html Epidural Hematoma http://www.chestjournal.org/cgi/content/full/122/2/699 http://www.bartleby.com/107/illus769.html Epidural Hematoma • Uncommon (<1% of all head injuries, 10% of post traumatic coma patients) • Located -

Strategies to Improve Nerve Regeneration After Radical Prostatectomy: a Narrative Review
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Institutional Research Information System University of Turin Strategies to improve nerve regeneration after radical prostatectomy: a narrative review Stefano Geuna 1, 2, Luisa Muratori1, 2, Federica Fregnan 1, 2, Matteo Manfredi4 , Riccardo Bertolo 3, 4 , Francesco Porpiglia4. 1 Department of Clinical and Biological Sciences, University of Turin, Orbassano (To), 10043, Italy. 2 Neuroscience Institute Cavalieri Ottolenghi (NICO), Orbassano (To), 10043, Italy. 3 Urological and Kidney Institute, Cleveland Clinic, Cleveland, OH, US. 4 Department of Oncology, University of Turin, Orbassano (To), 10043, Italy. Abstract Peripheral nerves are complex organs that spread throughout the entire human body. They are frequently affected by lesions not only as a result of trauma but also following radical tumor resection. In fact, despite the advancement in surgical techniques, such as nerve- sparing robot assisted radical prostatectomy, some degree of nerve injury may occur resulting in erectile dysfunction with significant impairment of the quality of life. The aim of this review is to provide an overview on the mechanisms of the regeneration of injured peripheral nerves and to describe the potential strategies to improve the regeneration process and the functional recovery. Yet, the recent advances in bio- engineering strategies to promote nerve regeneration in the urological field are outlined with a view on the possible future regenerative therapies which might ameliorate the functional outcome after radical prostatectomy. 1 Introduction Radical prostatectomy is the gold standard surgical treatment for organ-confined prostate cancer. The employment of innovative surgical technique such as nerve-sparing robot assisted radical prostatectomy allowed to magnify the anatomical field leading to a three- dimensional perspective obtained through the robotic lenses and a better anatomical knowledge. -

Feigned Consensus: Usurping the Law in Shaken Baby Syndrome/ Abusive Head Trauma Prosecutions
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Michigan School of Law University of Michigan Law School University of Michigan Law School Scholarship Repository Articles Faculty Scholarship 2020 Feigned Consensus: Usurping the Law in Shaken Baby Syndrome/ Abusive Head Trauma Prosecutions Keith A. Findley University of Wisconsin Law School D. Michael Risinger Seton Hall University School of Law Patrick D. Barnes Stanford University Medical Center Julie A. Mack Pennsylvania State University Medical Center David A. Moran University of Michigan Law School, [email protected] See next page for additional authors Available at: https://repository.law.umich.edu/articles/2102 Follow this and additional works at: https://repository.law.umich.edu/articles Part of the Criminal Procedure Commons, Evidence Commons, Juvenile Law Commons, and the Medical Jurisprudence Commons Recommended Citation Findley, Keith A. "Feigned Consensus: Usurping the Law in Shaken Baby Syndrome/Abusive Head Trauma Prosecutions." Michael Risinger, Patrick Barnes, Julie Mack, David A. Moran, Barry Scheck, and Thomas Bohan, co-authors. Wis. L. Rev. 2019, no. 4 (2019): 1211-268. This Article is brought to you for free and open access by the Faculty Scholarship at University of Michigan Law School Scholarship Repository. It has been accepted for inclusion in Articles by an authorized administrator of University of Michigan Law School Scholarship Repository. For more information, please contact [email protected]. Authors Keith A. Findley, D. Michael Risinger, Patrick D. Barnes, Julie A. Mack, David A. Moran, Barry C. Scheck, and Thomas L. Bohan This article is available at University of Michigan Law School Scholarship Repository: https://repository.law.umich.edu/articles/2102 FEIGNED CONSENSUS: USURPING THE LAW IN SHAKEN BABY SYNDROME/ ABUSIVE HEAD TRAUMA PROSECUTIONS KEITH A. -
Overcoming Defense Expert Testimony in Abusive Head Trauma Cases
NATIONAL CENTER FOR PROSECUTION OF CHILD ABUSE Special Topics in Child Abuse Overcoming Defense Expert Testimony in Abusive Head Trauma Cases By Dermot Garrett Edited by Eleanor Odom, Amanda Appelbaum and David Pendle NATIONAL CENTER FOR PROSECUTION OF CHILD ABUSE Scott Burns Director , National District Attorneys Association The National District Attorneys Association is the oldest and largest professional organization representing criminal prosecutors in the world. Its members come from the offices of district attorneys, state’s attorneys, attorneys general, and county and city prosecutors with responsibility for prosecuting criminal violations in every state and territory of the United States. To accomplish this mission, NDAA serves as a nationwide, interdisciplinary resource center for training, research, technical assistance, and publications reflecting the highest standards and cutting-edge practices of the prosecutorial profession. In 1985, the National District Attorneys Association recognized the unique challenges of crimes involving child victims and established the National Center for Prosecution of Child Abuse (NCPCA). NCPCA’s mission is to reduce the number of children victimized and exploited by assisting prosecutors and allied professionals laboring on behalf of victims too small, scared or weak to protect themselves. Suzanna Tiapula Director, National Center for Prosecution of Child Abuse A program of the National District Attorneys Association www.ndaa.org 703.549.9222 This project was supported by Grants #2010-CI-FX-K008 and [new VOCA grant #] awarded by the Office of Juvenile Justice and Delinquency Prevention. The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs. Points of view in this document are those of the author and do not necessarily represent the official position or policies of the U.S. -

Why Woodpecker Can Resist the Impact
Why woodpecker can resist the impact A thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy Zhe Zhang Master of Civil Engineering, RMIT University, Melbourne, Australia School of Engineering College of Science, Engineering and Health RMIT University November 2019 II Declaration I certify that except where due acknowledgement has been made, the work is that of the author alone; the work has not been submitted previously, in whole or in part, to qualify for any other academic award; the content of the thesis is the result of work which has been carried out since the official commencement date of the approved research program; any editorial work, paid or unpaid, carried out by a third party is acknowledged; and ethics procedures and guidelines have been followed. Zhe Zhang 30 November 2019 III Acknowledgments The research in this thesis could not have been completed without significant support from many individuals and organisations. I would like to take this opportunity to express my deep gratitude to all of them. Firstly, I would like to express my sincere gratitude to my senior supervisor, Dr. Shiwei Zhou, for his wisdom in choosing this fascinating research topic for me and his constant encouragement and guidance. After the guidance of my Master graduation project, Dr. Zhou accepted me as one of the Ph.D. students and offered financial support for my first-year study at RMIT University. He has always been patient in providing guidance and offering supportive suggestions to me during my PhD candidature period. It is not an exaggeration to say that he has changed my life and his good characteristics have had a significant and positive impact on me which would be beneficial for the rest of my life. -

Neuropathology Category Code List
Neuropathology Page 1 of 27 Neuropathology Major Category Code Headings Revised 10/2018 1 General neuroanatomy, pathology, and staining 65000 2 Developmental neuropathology, NOS 65400 3 Epilepsy 66230 4 Vascular disorders 66300 5 Trauma 66600 6 Infectious/inflammatory disease 66750 7 Demyelinating diseases 67200 8 Complications of systemic disorders 67300 9 Aging and neurodegenerative diseases 68000 10 Prion diseases 68400 11 Neoplasms 68500 12 Skeletal Muscle 69500 13 Peripheral Nerve 69800 14 Ophthalmic pathology 69910 Neuropathology Page 2 of 27 Neuropathology 1 General neuroanatomy, pathology, and staining 65000 A Neuroanatomy, NOS 65010 1 Neocortex 65011 2 White matter 65012 3 Entorhinal cortex/hippocampus 65013 4 Deep (basal) nuclei 65014 5 Brain stem 65015 6 Cerebellum 65016 7 Spinal cord 65017 8 Pituitary 65018 9 Pineal 65019 10 Tracts 65020 11 Vascular supply 65021 12 Notochord 65022 B Cell types 65030 1 Neurons 65031 2 Astrocytes 65032 3 Oligodendroglia 65033 4 Ependyma 65034 5 Microglia and mononuclear cells 65035 6 Choroid plexus 65036 7 Meninges 65037 8 Blood vessels 65038 C Cerebrospinal fluid 65045 D Pathologic responses in neurons and axons 65050 1 Axonal degeneration/spheroid/reaction 65051 2 Central chromatolysis 65052 3 Tract degeneration 65053 4 Swollen/ballooned neurons 65054 5 Trans-synaptic neuronal degeneration 65055 6 Olivary hypertrophy 65056 7 Acute ischemic (hypoxic) cell change 65057 8 Apoptosis 65058 9 Protein aggregation 65059 10 Protein degradation/ubiquitin pathway 65060 E Neuronal nuclear inclusions 65100 -

383. Subdural Block and the Anaesthetist
SUBDURAL BLOCK AND THE ANAESTHETIST Anaesthesia and Intensive Care, 2010,Vol 38, No. 1 D Agarwal, M Mohta, A Tyagi, AK Sethi Department of Anaesthesiology and Critical Care, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India SUMMARY There are a number of case reports describing accidental subdural block during the performance of subarachnoid or epidural anaesthesia. However, it appears that subdural drug deposition remains a poorly understood complication of neuraxial anaesthesia. The clinical presentation may often be attributed to other causes. Subdural injection of local anaesthetic can present as high sensory block, sometimes even involving the cranial nerves due to extension of the subdural space into the cranium. The block is disproportionate to the amount of drug injected, often with sparing of sympathetic and motor fibres. On the other hand, the subdural deposition can also lead to failure of the intended block. The variable presentation can be explained by the anatomy of this space. High suspicion in the presence of predisposing factors and early detection could prevent further complications. This review aims at increasing awareness amongst anaesthetists about inadvertent subdural block. It reviews the relevant anatomy, incidence, predisposing factors, presentation, diagnosis and management of unintentional subdural block during the performance of neuraxial anaesthesia. Central neuraxial blockade is a commonly performed anaesthetic technique1. While generally being a very reliable technique, occasionally an unexpectedly high or low level of block is achieved. This could potentially be secondary to the deposition of local anaesthetic in a meningeal plane other than that desired. One such plane is the subdural space, which lies between the dura and arachnoid mater. -

Subarachnoid Trabeculae: a Comprehensive Review of Their Embryology, Histology, Morphology, and Surgical Significance Martin M
Literature Review Subarachnoid Trabeculae: A Comprehensive Review of Their Embryology, Histology, Morphology, and Surgical Significance Martin M. Mortazavi1,2, Syed A. Quadri1,2, Muhammad A. Khan1,2, Aaron Gustin3, Sajid S. Suriya1,2, Tania Hassanzadeh4, Kian M. Fahimdanesh5, Farzad H. Adl1,2, Salman A. Fard1,2, M. Asif Taqi1,2, Ian Armstrong1,2, Bryn A. Martin1,6, R. Shane Tubbs1,7 Key words - INTRODUCTION: Brain is suspended in cerebrospinal fluid (CSF)-filled sub- - Arachnoid matter arachnoid space by subarachnoid trabeculae (SAT), which are collagen- - Liliequist membrane - Microsurgical procedures reinforced columns stretching between the arachnoid and pia maters. Much - Subarachnoid trabeculae neuroanatomic research has been focused on the subarachnoid cisterns and - Subarachnoid trabecular membrane arachnoid matter but reported data on the SAT are limited. This study provides a - Trabecular cisterns comprehensive review of subarachnoid trabeculae, including their embryology, Abbreviations and Acronyms histology, morphologic variations, and surgical significance. CSDH: Chronic subdural hematoma - CSF: Cerebrospinal fluid METHODS: A literature search was conducted with no date restrictions in DBC: Dural border cell PubMed, Medline, EMBASE, Wiley Online Library, Cochrane, and Research Gate. DL: Diencephalic leaf Terms for the search included but were not limited to subarachnoid trabeculae, GAG: Glycosaminoglycan subarachnoid trabecular membrane, arachnoid mater, subarachnoid trabeculae LM: Liliequist membrane ML: Mesencephalic leaf embryology, subarachnoid trabeculae histology, and morphology. Articles with a PAC: Pia-arachnoid complex high likelihood of bias, any study published in nonpopular journals (not indexed PPAS: Potential pia-arachnoid space in PubMed or MEDLINE), and studies with conflicting data were excluded. SAH: Subarachnoid hemorrhage SAS: Subarachnoid space - RESULTS: A total of 1113 articles were retrieved. -

Spinal Meninges Neuroscience Fundamentals > Regional Neuroscience > Regional Neuroscience
Spinal Meninges Neuroscience Fundamentals > Regional Neuroscience > Regional Neuroscience SPINAL MENINGES GENERAL ANATOMY Meningeal Layers From outside to inside • Dura mater • Arachnoid mater • Pia mater Meningeal spaces From outside to inside • Epidural (above the dura) - See: epidural hematoma and spinal cord compression from epidural abscess • Subdural (below the dura) - See: subdural hematoma • Subarachnoid (below the arachnoid mater) - See: subarachnoid hemorrhage Spinal canal Key Anatomy • Vertebral body (anteriorly) • Vertebral arch (posteriorly). • Vertebral foramen within the vertebral arch. MENINGEAL LAYERS 1 / 4 • Dura mater forms a thick ring within the spinal canal. • The dural root sheath (aka dural root sleeve) is the dural investment that follows nerve roots into the intervertebral foramen. • The arachnoid mater runs underneath the dura (we lose sight of it under the dural root sheath). • The pia mater directly adheres to the spinal cord and nerve roots, and so it takes the shape of those structures. MENINGEAL SPACES • The epidural space forms external to the dura mater, internal to the vertebral foramen. • The subdural space lies between the dura and arachnoid mater layers. • The subarachnoid space lies between the arachnoid and pia mater layers. CRANIAL VS SPINAL MENINGES&NBSP; Cranial Meninges • Epidural is a potential space, so it's not a typical disease site unless in the setting of high pressure middle meningeal artery rupture or from traumatic defect. • Subdural is a potential space but bridging veins (those that pass from the subarachnoid space into the dural venous sinuses) can tear, so it is a common site of hematoma. • Subarachnoid space is an actual space and is a site of hemorrhage and infection, for example. -

OIICS Manual 2012
SECTION 2 Definitions, Rules of Selection, and Titles and Descriptions SECTION CONTENTS 2.1 Nature of Injury or Illness 2.2 Part of Body Affected 2.3 Source and Secondary Source of Injury or Illness 2.4 Event or Exposure *-Asterisks denote a summary level code not assigned to individual cases. _____________________________________________________________________________________________ 01/12 6 SECTION 2.1 Nature of Injury or Illness SECTION CONTENTS 2.1.1 Definition, Rules of Selection 2.1.2 Titles and Descriptions *-Asterisks denote a summary level code not assigned to individual cases. _____________________________________________________________________________________________ 01/12 7 2.1.1 Nature of Injury or Illness—Definition, Rules of Selection 1.0 DEFINITION The nature of injury or illness identifies the principal physical characteristic(s) of the work related injury or illness. RULES OF SELECTION: 1.1 Name the injury or illness indicated on the source document. Example: For strained back, choose Strains. 1.2 When two or more injuries or illnesses are indicated, and one is a sequela, aftereffect, complication due to medical treatment, or re-injury, choose the initial injury or illness. Example: If a laceration became infected developing into septicemia, choose Cuts, lacerations. 1.3 When two or more injuries or illnesses are indicated and one is more severe than the other(s) and is not a sequela or complication of the other injury or illness, select the more severe injury or illness. Example: For sprained finger and fractured wrist, choose Fractures. 1.3.1 When a single event or exposure produces an injury and transmits a disease simultaneously, and one is more severe than the other(s), select the more severe injury or disease. -

Intracranial Hemorrhage
Intracranial Hemorrhage MARK MOSS, M.D. INTERVENTIONAL NEURORADIOLOGY WASHINGTON REGIONAL MEDICAL CENTER Definitions Stroke Clinical syndrome of rapid onset deficits of brain function lasting more than 24 hours or leading to death Transient Ischemic attack (TIA) Clinical syndrome of rapid onset deficits of brain function which resolves within 24 hours Epidemiology Stroke is the leading cause of adult disabilities 2nd leading cause of death worldwide 3rd leading cause of death in the U.S. 800,000 strokes per year resulting in 150,000 deaths Deaths are projected to increase exponentially in the next 30 years owing to the aging population The annual cost of stroke in the U.S. is estimated at $69 billion Stroke can be divided into hemorrhagic and ischemic origins 13% hemorrhagic 87% ischemic Intracranial Hemorrhage Collective term encompassing many different conditions characterized by the extravascular accumulation of blood within different intracranial spaces. OBJECTIVES: Define types of ICH Discuss best imaging modalities Subarachnoid hemorrhage / Aneurysms Roles of endovascular surgery Intracranial hemorrhage Outside the brain (Extra-axial) hemorrhage Subdural hematoma (SDH) Epidural hematoma (EDH) Subarachnoid hematoma (SAH) Intraventricular (IVH) Inside the brain (Intra-axial) hemorrhage Intraparenchymal hematoma (basal ganglia, lobar, pontine etc.) Your heads compartments Scalp Subgaleal Space Bone (calvarium) Dura Mater thick tough membrane Arachnoid flimsy transparent membrane Pia Mater tightly hugs the