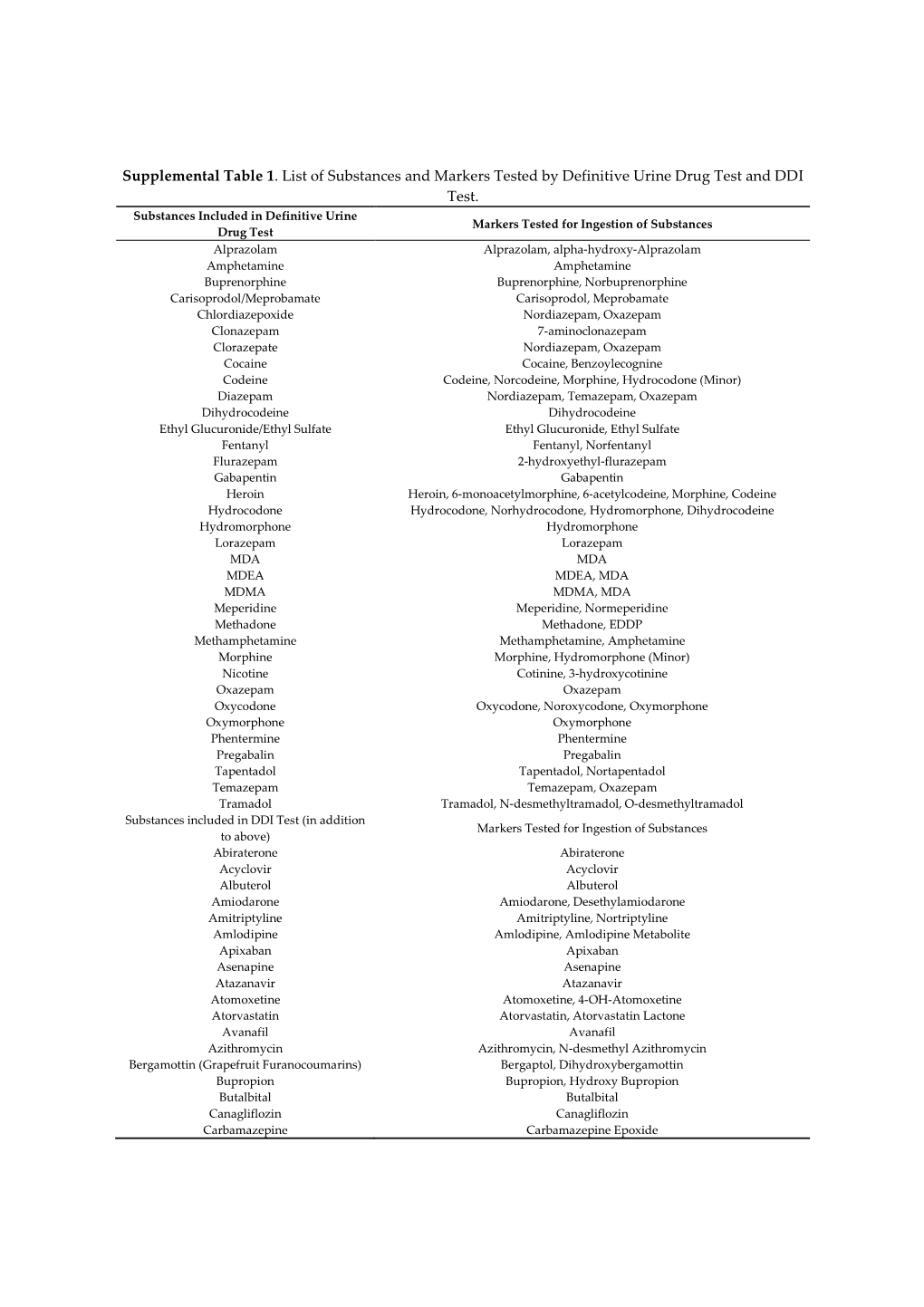
Supplemental Table 1. List of Substances and Markers Tested by Definitive Urine Drug Test and DDI Test
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Presentations September 23Rd - Rooms 1,2 and 3
Oral Presentations September 23rd - Rooms 1,2 and 3 Presentation Date Abstract Authors Presenter´s name - Theme Title Code indicated by the author 18498 Thomas Smits; Femke Gresnigt; Thomas Smits Clinical Toxicology/drugs of PERFORMANCE OF AN IMMUNOASSAY Eric Franssen; Milly Attema-de abuse METHOD FOR GAMMA-HYDROXYBUTYRIC Jonge ACID (GHB) IN PATIENTS PRESENTED AT THE EMERGENCY DEPARTMENT, A PROSPECTIVE STUDY 18499 Thomas Smits; Femke Gresnigt; Thomas Smits Clinical Toxicology/drugs of DO WE NEED POINT-OF-CARE TESTING OF Milly Attema-de Jonge; Eric abuse GAMMA-HYDROXYBUTYRIC ACID (GHB) AT Fransse THE EMERGENCY DEPARTMENT? September 23 18730 Lilian H.J. Richter; Julia Menges; Lea Wagmann Clinical Toxicology/drugs of NEW PSYCHOACTIVE SUBSTANCES: Lea Wagmann; Simon D. Brandt; abuse METABOLIC FATE, ISOZYME-MAPPING, 13:30 - 14:45 Folker Westphal; Veit Flockerzi; AND PLASMA PROTEIN BINDING OF 5-APB- ROOM 1 Markus R. Meyer NBOME, 2C-B-FLY-NB2ETO5CL, AND 2C-B- FLY-NBOME 18985 Annelies Cannaert; Marie Annelies Cannaert Clinical Toxicology/drugs of HIDE AND SEEK: OVERCOMING THE Deventer; Melissa Fogarty; abuse MASKING EFFECT OF OPIOID Amanda L.A. Mohr; Christophe P. ANTAGONISTS IN ACTIVITY-BASED Stove SCREENING TESTS 18740 Souleiman El Balkhi ; Roland Souleiman El Balkhi Clinical Toxicology/drugs of METABOLIC INTERACTIONS BETWEEN Lawson; Franck Saint-Marcoux abuse OXYCODONE, BENZODIAZEPINES OR DESIGNER BENZODIAZEPINES PLAY AN IMPORTANT ROLE IN OXYCODONE INTOXICATIONS 19050 Brenda de Winter F de Velde; MN Brenda de Winter Anti-infective drugs POPULATION -

Long Term Follow up of Mirabegron - a Real Life- Pragmatic Experience
Central Journal of Urology and Research Bringing Excellence in Open Access Research Article *Corresponding author Haitham Abdelmoteleb, Bristol Urological Institute, Southmead Hospital, Bristol, BS10 5NB, UK, Tel: 440-7884- Long Term Follow Up of 827995; Email: Submitted: 04 June 2016 Mirabegron - A Real Life- Accepted: 22 August 2016 Published: 24 August 2016 ISSN: 2379-951X Pragmatic Experience Copyright Haitham Abdelmoteleb*, Musaab Yassin, and Hashim Hashim © 2016 Abdelmoteleb et al. Bristol Urological Institute, South mead Hospital, UK OPEN ACCESS Abstract Keywords • Mirabegron Objectives: To evaluate the efficacy and tolerability of Mirabegron for the • Beta-3 agonist treatment of overactive bladder symptoms in a real life, long term follow up study • Overactive bladder syndrome conducted in a tertiary referral centre. • Long term Methods: A structured telephone questionnaire of patients was conducted in order to evaluate the efficacy and tolerability of Mirabegron. Patients who were initially prescribed and responded to Mirabegron 50mg once daily between 6/2013 and 9/2013, were interviewed to see if they were compliant with treatment, continue to respond to treatment and if they discontinued treatment. Results: Follow-up was for a mean of 11.7 months. At short-term follow-up, 20/39 patients responded to treatment. In the long term follow-up, 18/20 patients were still using Mirabegron. 2/20 patients discontinued because of lack of efficacy. Overall, the main reasons for discontinuation of Mirabegron after trying it for a mean of 5.3 months, was lack of efficacy and adverse events. The majority of AEs were mild in severity and few were serious. Other reasons include the lack of further prescription from general practitioners. -

Betmiga, INN-Mirabegron
EMA/591015/2015 EMEA/H/C/002388 EPAR summary for the public Betmiga mirabegron This is a summary of the European public assessment report (EPAR) for Betmiga. It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the medicine to reach its opinion in favour of granting a marketing authorisation and its recommendations on the conditions of use for Betmiga. What is Betmiga? Betmiga is a medicine containing the active substance mirabegron. It is available as prolonged-release tablets (25 mg, 50 mg). ‘Prolonged-release’ means that mirabegron is released slowly from the tablet over a few hours. What is Betmiga used for? Betmiga is used in adults with overactive bladder syndrome. It is used to treat certain symptoms of the condition: urgency (sudden urge to urinate), increased urinary frequency (the need to urinate frequently) and urge incontinence (involuntary leakage of urine from the bladder when a sudden strong need to urinate is felt). The medicine can only be obtained with a prescription. How is Betmiga used? The recommended dose of Betmiga is 50 mg once a day. In patients who have reduced kidney or liver function the doctor may need to prescribe a lower dose or avoid the use of Betmiga, especially in patients taking certain other medicines. For full details, see the package leaflet (also part of the EPAR). 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2015. -

Dezocine Exhibits Antihypersensitivity Activities in Neuropathy Through
www.nature.com/scientificreports OPEN Dezocine exhibits antihypersensitivity activities in neuropathy through spinal Received: 09 November 2016 Accepted: 19 January 2017 μ-opioid receptor activation and Published: 23 February 2017 norepinephrine reuptake inhibition Yong-Xiang Wang1, Xiao-Fang Mao1, Teng-Fei Li1, Nian Gong1 & Ma-Zhong Zhang2 Dezocine is the number one opioid painkiller prescribed and sold in China, occupying 44% of the nation’s opioid analgesics market today and far ahead of the gold-standard morphine. We discovered the mechanisms underlying dezocine antihypersensitivity activity and assessed their implications to antihypersensitivity tolerance. Dezocine, given subcutaneously in spinal nerve-ligated neuropathic rats, time- and dose-dependently produced mechanical antiallodynia and thermal antihyperalgesia, significantly increased ipsilateral spinal norepinephrine and serotonin levels, and induced less antiallodynic tolerance than morphine. Its mechanical antiallodynia was partially (40% or 60%) and completely (100%) attenuated by spinal μ-opioid receptor (MOR) antagonism or norepinephrine depletion/α2-adrenoceptor antagonism and combined antagonism of MORs and α2-adenoceptors, respectively. In contrast, antagonism of spinal κ-opioid receptors (KORs) and δ-opioid receptors (DORs) or depletion of spinal serotonin did not significantly alter dezocine antiallodynia. In addition, dezocine- delayed antiallodynic tolerance was accelerated by spinal norepinephrine depletion/α2-adenoceptor antagonism. Thus dezocine produces antihypersensitivity activity through spinal MOR activation and norepinephrine reuptake inhibition (NRI), but apparently not through spinal KOR and DOR activation, serotonin reuptake inhibition or other mechanisms. Our findings reclassify dezocine as the first analgesic of the recently proposed MOR-NRI, and reveal its potential as an alternative to as well as concurrent use with morphine in treating pain. -

Frailty & Cognihon: Management of OAB in Elderly & Frail Pahents
Frailty & Cogni.on: Management of OAB in Elderly & Frail Pa.ents MR. RAHUL MISTRY CONSULTANT UROLOGICAL SURGEON POGP CONFERENCE NOVEMBER 2016 Topics • What are LUTS? • Symptom definiDons • The impact of OAB on paents • Management of OAB • The challenge of treang OAB • The Ancholinergic burden • Novel treatment of OAB Change of Terminology • LUTS = Lower urinary tract symptoms • LUTS instead of “prostasm” • Storage instead of “irritave” • Voiding instead of “obstrucDve” What are LUTS Post-micturion Storage symptoms Voiding symptoms symptoms DayDme frequency Slow stream Post-micturiDon Nocturia Spraying dribbling Incomplete Urgency IntermiUency emptying Urinary Hesitancy inconnence Straining Terminal dribbling Definions • Urgency - sudden compelling desire to pass urine which is difficult to defer • Urinary inconnence • any involuntary leakage of urine (urge / stress) • may need to be disDnguished from sweang or vaginal discharge • Increased dayme frequency - the complaint by the paent who considers that he/she voids too o]en by day • Nocturia - individual has to wake at night one or more Dmes to void • ICS DefiniDons, Abrams P et al. Neurourol Urodyn; 21:167-178 (2002) Defini.on of Overac.ve Bladder (OAB) (Internaonal Connence Society) 1. Abrams P et al. Neurourol Urodyn 2002;21:167-178 Mrs W. E. Terrible, your classic pa.ent? Age: 64 year old woman Occupaon: Recently reDred from an office job Symptoms: • Urinary frequency (14−15 Dmes a day) • Urge inconDnence (daily) • Nocturia (3 Dmes a night) THe impact of OAB on pa.ents How do OAB symptoms affect pa.ents? haven’t slept depressing like a baby negave lose control locked in embarrassing exhausted no control terrible so red I keep it xxx secret Quotes from a video of real-life OAB paents talking about how OAB has affected their lives. -

A Review of Unique Opioids and Their Conversions
A Review of Unique Opioids and Their Conversions Jacqueline Cleary, PharmD, BCACP Assistant Professor Albany College of Pharmacy and Health Sciences Adjunct Professor SAGE College of Nursing DISCLOSURES • Kaleo • Remitigate, LLC OBJECTIVES • Compare and contrast unique pharmacotherapy options for the treatment of chronic pain including: methadone, buprenoprhine, tapentadol, and tramadol • Select methadone, buprenorphine, tapentadol, or tramadol based on patient specific factors • Apply appropriate opioid conversion strategies to unique opioids • Understand opioid overdose risk surrounding opioid conversions and the use of unique opioids UNIQUE OPIOIDS METHADONE, BUPRENORPHINE, TRAMADOL, TAPENTADOL METHADONE My favorite drug because….? METHADONE- INDICATIONS • FDA labeled indications – (1) chronic pain (2) detoxification Oral soluble tablets for suspension NOT indicated for chronic pain treatment • Initial inpatient detoxification of opioids by a licensed trained provider with methadone and supportive care is appropriate • Methadone maintenance provider must have special credentialing and training as required by state Outpatient prescription must be for pain ONLY and say “for pain” on RX • Continuation of methadone maintenance from outside provider while patient is inpatient for another condition is appropriate http://cdn.atforum.com/wp-content/uploads/SAMHSA-2015-Guidelines-for-OTPs.pdf MECHANISM OF ACTION • Potent µ-opioid agonist • NMDA receptor antagonist • Norepinephrine reuptake inhibitor • Serotonin reuptake inhibitor ADVERSE EVENTS -

Herbal Medicines in Pregnancy and Lactation : an Evidence-Based
00 Prelims 1410 10/25/05 2:13 PM Page i Herbal Medicines in Pregnancy and Lactation An Evidence-Based Approach Edward Mills DPh MSc (Oxon) Director, Division of Clinical Epidemiology Canadian College of Naturopathic Medicine North York, Ontario, Canada Jean-Jacques Duguoa MSc (cand.) ND Naturopathic Doctor Toronto Western Hospital Assistant Professor Division of Clinical Epidemiology Canadian College of Naturopathic Medicine North York, Ontario, Canada Dan Perri BScPharm MD MSc Clinical Pharmacology Fellow University of Toronto Toronto, Ontario, Canada Gideon Koren MD FACMT FRCP Director of Motherisk Professor of Medicine, Pediatrics and Pharmacology University of Toronto Toronto, Ontario, Canada With a contribution from Paul Richard Saunders PhD ND DHANP 00 Prelims 1410 10/25/05 2:13 PM Page ii © 2006 Taylor & Francis Medical, an imprint of the Taylor & Francis Group First published in the United Kingdom in 2006 by Taylor & Francis Medical, an imprint of the Taylor & Francis Group, 2 Park Square, Milton Park, Abingdon, Oxon OX14 4RN Tel.: ϩ44 (0)20 7017 6000 Fax.: ϩ44 (0)20 7017 6699 E-mail: [email protected] Website: www.tandf.co.uk/medicine All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or trans- mitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of the publisher or in accordance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any licence permitting limited copying issued by the Copyright Licensing Agency, 90 Tottenham Court Road, London W1P 0LP. -

Drugs to Avoid in Patients with Dementia
Detail-Document #240510 -This Detail-Document accompanies the related article published in- PHARMACIST’S LETTER / PRESCRIBER’S LETTER May 2008 ~ Volume 24 ~ Number 240510 Drugs To Avoid in Patients with Dementia Elderly people with dementia often tolerate drugs less favorably than healthy older adults. Reasons include increased sensitivity to certain side effects, difficulty with adhering to drug regimens, and decreased ability to recognize and report adverse events. Elderly adults with dementia are also more prone than healthy older persons to develop drug-induced cognitive impairment.1 Medications with strong anticholinergic (AC) side effects, such as sedating antihistamines, are well- known for causing acute cognitive impairment in people with dementia.1-3 Anticholinergic-like effects, such as urinary retention and dry mouth, have also been identified in drugs not typically associated with major AC side effects (e.g., narcotics, benzodiazepines).3 These drugs are also important causes of acute confusional states. Factors that may determine whether a patient will develop cognitive impairment when exposed to ACs include: 1) total AC load (determined by number of AC drugs and dose of agents utilized), 2) baseline cognitive function, and 3) individual patient pharmacodynamic and pharmacokinetic features (e.g., renal/hepatic function).1 Evidence suggests that impairment of cholinergic transmission plays a key role in the development of Alzheimer’s dementia. Thus, the development of the cholinesterase inhibitors (CIs). When used appropriately, the CIs (donepezil [Aricept], rivastigmine [Exelon], and galantamine [Razadyne, Reminyl in Canada]) may slow the decline of cognitive and functional impairment in people with dementia. In order to achieve maximum therapeutic effect, they ideally should not be used in combination with ACs, agents known to have an opposing mechanism of action.1,2 Roe et al studied AC use in 836 elderly patients.1 Use of ACs was found to be greater in patients with probable dementia than healthy older adults (33% vs. -

Tizanidine Brands: Zanaflex®
Medication Information Sheet Tizanidine brands: Zanaflex® Medications are only ONE part of a successful treatment plan. They are appropriate when they provide benefit, improve function and have either no or mild, manageable side effects. Importantly, medications (even if natural) are chemical substances not expected in the body, and as such have side effects. Some of the side effects might be unknown. The use of medications/drugs for any purpose requires patient consent. This practice does NOT require a patient to use any medication. Information & potential benefits Tizanidine is a medication that helps with muscle spasms and musculoskeletal pain syndromes; there is evidence that it helps neuropathic and musculoskeletal pain through alpha‐2‐receptor activity. Studies have shown Zanaflex helpful for neuropathic pain and some types of headache. It is currently FDA approved for muscle spasticity. Potential risks and side effects Tizanidine should be used carefully in cases of liver or kidney disease, low blood pressure, or heart conduction problems (QT interval problems). It should not be used with Luvox or with the antibiotic Cipro (ciprofloxacin). There are many other drugs that can interact with Tizanadine. In addition to the standard side effects listed in the disclaimer, common side effects or Zanaflex include dry mouth, sleepiness, dizziness, asthenia, infection, constipation, urinary frequency, flu‐like feeling, low blood pressure, more spasms, sore throat and runny nose. More serious side effects include liver damage, severe slowing of the heart beat and hallucinations. Tizanidine occasionally causes liver injury. In controlled clinical studies, approximately 5% of patients treated with tizanidine had non‐serious elevations of liver function tests. -

Hydromorphone
Hydromorphone WHAT IS HYDROMORPHONE? sedation, and reduced anxiety. It may also cause Hydromorphone belongs to a class of drugs mental clouding, changes in mood, nervousness, called “opioids,” which includes morphine. It and restlessness. It works centrally (in the has an analgesic potency of two to eight times brain) to reduce pain and suppress cough. greater than that of morphine and has a rapid Hydromorphone use is associated with both onset of action. physiological and psychological dependence. WHAT IS ITS ORIGIN? What is its effect on the body? Hydromorphone is legally manufactured and Hydromorphone may cause: distributed in the United States. However, • Constipation, pupillary constriction, urinary retention, users can obtain hydromorphone from nausea, vomiting, respiratory depression, dizziness, forged prescriptions, “doctor-shopping,” impaired coordination, loss of appetite, rash, slow or theft from pharmacies, and from friends and rapid heartbeat, and changes in blood pressure acquaintances. What are its overdose effects? What are the street names? Acute overdose of hydromorphone can produce: Common street names include: Severe respiratory depression, drowsiness • D, Dillies, Dust, Footballs, Juice, and Smack progressing to stupor or coma, lack of skeletal muscle tone, cold and clammy skin, constricted What does it look like? pupils, and reduction in blood pressure and heart Hydromorphone comes in: rate • Tablets, capsules, oral solutions, and injectable Severe overdose may result in death due to formulations respiratory depression. How is it abused? Which drugs cause similar effects? Users may abuse hydromorphone tablets by Drugs that have similar effects include: ingesting them. Injectable solutions, as well as • Heroin, morphine, hydrocodone, fentanyl, and tablets that have been crushed and dissolved oxycodone in a solution may be injected as a substitute for heroin. -

Prescription Drug Management
Check out our new site: www.acllaboratories.com Prescription Drug Management Non Adherence, Drug Misuse, Increased Healthcare Costs Reports from the Centers for DiseasePrescription Control and Prevention (CDC) say Drug deaths from Managementmedication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription Nondrugs. Adherence,1 Drug Misuse, Increased Healthcare Costs The CDC analysis found that nearly 40,000 drug overdose deaths were reported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths from illegal street drugs. Abuse of painkillers like ReportsOxyContin from and the VicodinCenters forwere Disease linked Control to the and majority Prevention of the (CDC) deaths, say deaths from according to the report.1 medication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription drugs. 1 A health economics study analyzed managed care claims of more than 18 million patients, finding that patients undergoing opioid therapyThe CDCfor chronic analysis pain found who that may nearly not 40,000 be following drug overdose their prescription deaths were regimenreported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths have significantly higher overall healthcare costs. from illegal street drugs. Abuse of painkillers like OxyContin and Vicodin were linked to the majority of the deaths, according to the report.1 ACL offers drug management testing to provide information that can aid clinicians in therapy and monitoring to help improve patientA health outcomes. -
LC-MS for Pain Management Support
LC-MS for Pain Management Support Gwen McMillin, PhD, DABCC(CC,TC) University of Utah ARUP Laboratories Outline .Overview of drug testing, as a component of the therapeutic plan, in the management of chronic pain .A mini-SWOT analysis for application of LC- MS to pain management drug testing .Considerations for optimizing utility of LC-MS results Drug testing in pain management . Baseline testing, before initiating opioid therapy . Routine testing . Periodic, based on patient risk assessment . To evaluate changes . Therapeutic plan (drugs, formulations, dosing) . Clinical response (poor pain control, toxicity) . Clinical events (disease, surgery, pregnancy) . Patient behavior Objectives of drug testing Non- Detect and encourage Adherence appropriate drug use Detect and discourage Adherence inappropriate drug use Traditional approach . Immunoassay-based screen Screen . Confirm screen positive results with mass spectrometric method (GC-MS, LC-MS) Not appropriate for pain management Confirm + . Reflex testing leads to unnecessary expenses if the results are consistent with expectations, or if results are not used to make patient care decisions Confirm + . Confirmation of negative results may be more important than confirmation of positive results . Immunoassay-based screens may not be available Confirm + for specimens and drugs of interest Drugs monitored for pain management represent ~25% of “Top 200” prescriptions filled, 2011 .Analgesics .Anxiolytics, muscle . Hydrocodone (#1, 2, 14, 139) relaxants . Oxycodone (#45, 48, 121, 129, 196)