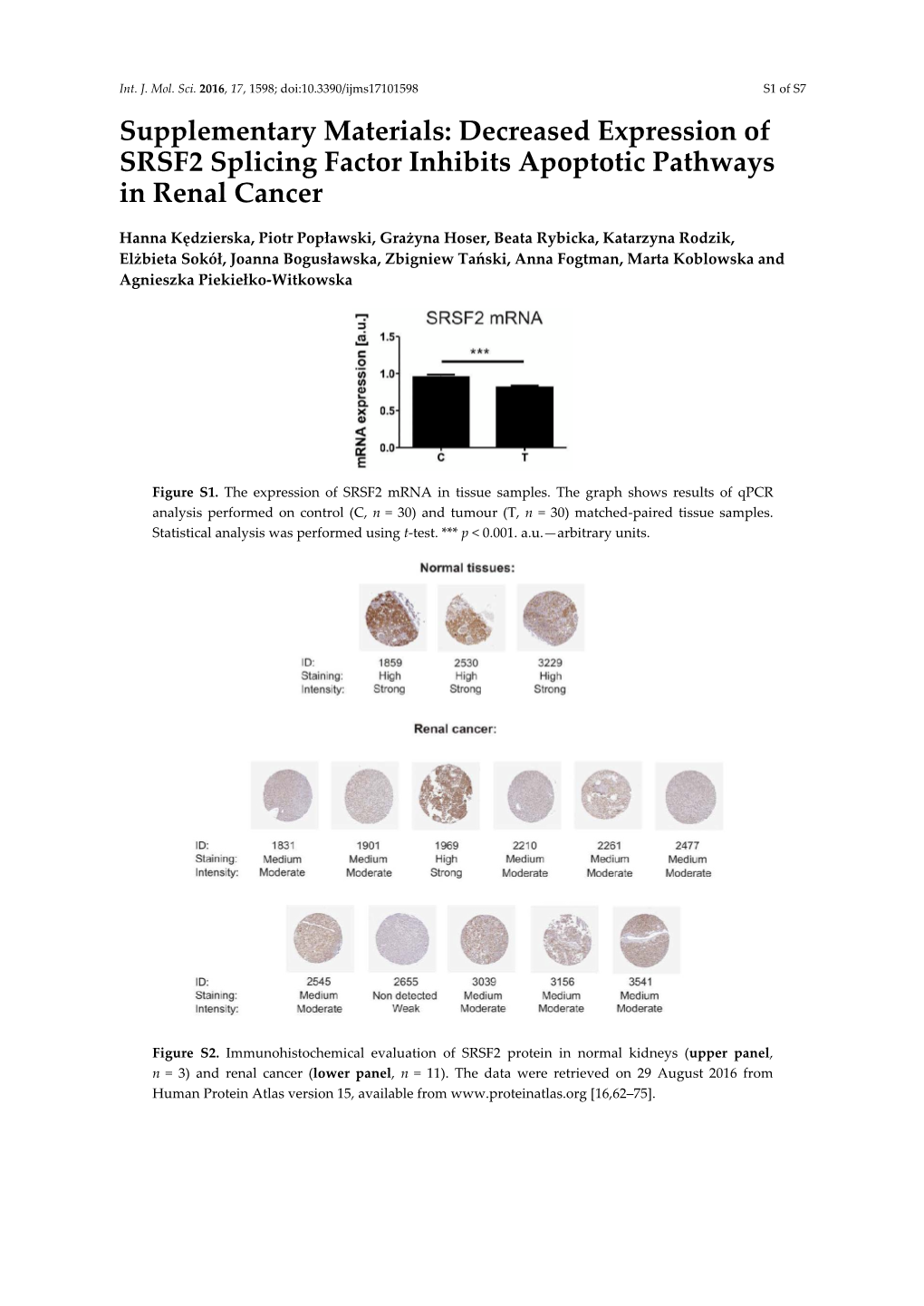
Decreased Expression of SRSF2 Splicing Factor Inhibits Apoptotic Pathways in Renal Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epigenetic Reprogramming Sensitizes CML Stem Cells to Combined EZH2 and Tyrosine
Published OnlineFirst September 14, 2016; DOI: 10.1158/2159-8290.CD-16-0263 RESEARCH BRIEF Epigenetic Reprogramming Sensitizes CML Stem Cells to Combined EZH2 and Tyrosine Kinase Inhibition Mary T. Scott 1 , 2 , Koorosh Korfi 1 , 2 , Peter Saffrey 1 , Lisa E.M. Hopcroft 2 , Ross Kinstrie 1 , Francesca Pellicano 2 , Carla Guenther 1 , 2 , Paolo Gallipoli 2 , Michelle Cruz 1 , Karen Dunn 2 , Heather G. Jorgensen 2 , Jennifer E. Cassels 2 , Ashley Hamilton 2 , Andrew Crossan 1 , Amy Sinclair 2 , Tessa L. Holyoake 2 , and David Vetrie 1 ABSTRACT A major obstacle to curing chronic myeloid leukemia (CML) is residual disease main- tained by tyrosine kinase inhibitor (TKI)–persistent leukemic stem cells (LSC). These are BCR–ABL1 kinase independent, refractory to apoptosis, and serve as a reservoir to drive relapse or TKI resistance. We demonstrate that Polycomb Repressive Complex 2 is misregulated in chronic phase CML LSCs. This is associated with extensive reprogramming of H3K27me3 targets in LSCs, thus sensi- tizing them to apoptosis upon treatment with an EZH2-specifi c inhibitor (EZH2i). EZH2i does not impair normal hematopoietic stem cell survival. Strikingly, treatment of primary CML cells with either EZH2i or TKI alone caused signifi cant upregulation of H3K27me3 targets, and combined treatment further potentiated these effects and resulted in signifi cant loss of LSCs compared to TKI alone, in vitro , and in long-term bone marrow murine xenografts. Our fi ndings point to a promising epigenetic-based thera- peutic strategy to more effectively target LSCs in patients with CML receiving TKIs. SIGNIFICANCE: In CML, TKI-persistent LSCs remain an obstacle to cure, and approaches to eradicate them remain a signifi cant unmet clinical need. -

Signaling TNF-Like Ligand 1A/Death Receptor 3 the Adaptor Protein
The Adaptor Protein TRADD Is Essential for TNF-Like Ligand 1A/Death Receptor 3 Signaling This information is current as Yelena L. Pobezinskaya, Swati Choksi, Michael J. Morgan, of September 27, 2021. Xiumei Cao and Zheng-gang Liu J Immunol 2011; 186:5212-5216; Prepublished online 18 March 2011; doi: 10.4049/jimmunol.1002374 http://www.jimmunol.org/content/186/9/5212 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2011/03/18/jimmunol.100237 Material 4.DC1 http://www.jimmunol.org/ References This article cites 29 articles, 13 of which you can access for free at: http://www.jimmunol.org/content/186/9/5212.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 27, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology The Adaptor Protein TRADD Is Essential for TNF-Like Ligand 1A/Death Receptor 3 Signaling Yelena L. Pobezinskaya, Swati Choksi, Michael J. Morgan, Xiumei Cao, and Zheng-gang Liu TNFR-associated death domain protein (TRADD) is a key effector protein of TNFR1 signaling. -

Gene Essentiality Landscape and Druggable Oncogenic Dependencies in Herpesviral Primary Effusion Lymphoma
ARTICLE DOI: 10.1038/s41467-018-05506-9 OPEN Gene essentiality landscape and druggable oncogenic dependencies in herpesviral primary effusion lymphoma Mark Manzano1, Ajinkya Patil1, Alexander Waldrop2, Sandeep S. Dave2, Amir Behdad3 & Eva Gottwein1 Primary effusion lymphoma (PEL) is caused by Kaposi’s sarcoma-associated herpesvirus. Our understanding of PEL is poor and therefore treatment strategies are lacking. To address this 1234567890():,; need, we conducted genome-wide CRISPR/Cas9 knockout screens in eight PEL cell lines. Integration with data from unrelated cancers identifies 210 genes as PEL-specific oncogenic dependencies. Genetic requirements of PEL cell lines are largely independent of Epstein-Barr virus co-infection. Genes of the NF-κB pathway are individually non-essential. Instead, we demonstrate requirements for IRF4 and MDM2. PEL cell lines depend on cellular cyclin D2 and c-FLIP despite expression of viral homologs. Moreover, PEL cell lines are addicted to high levels of MCL1 expression, which are also evident in PEL tumors. Strong dependencies on cyclin D2 and MCL1 render PEL cell lines highly sensitive to palbociclib and S63845. In summary, this work comprehensively identifies genetic dependencies in PEL cell lines and identifies novel strategies for therapeutic intervention. 1 Department of Microbiology-Immunology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA. 2 Duke Cancer Institute and Center for Genomic and Computational Biology, Duke University, Durham, NC 27708, USA. 3 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA. Correspondence and requests for materials should be addressed to E.G. (email: [email protected]) NATURE COMMUNICATIONS | (2018) 9:3263 | DOI: 10.1038/s41467-018-05506-9 | www.nature.com/naturecommunications 1 ARTICLE NATURE COMMUNICATIONS | DOI: 10.1038/s41467-018-05506-9 he human oncogenic γ-herpesvirus Kaposi’s sarcoma- (IRF4), a critical oncogene in multiple myeloma33. -

The TNF and TNF Receptor Review Superfamilies: Integrating Mammalian Biology
Cell, Vol. 104, 487±501, February 23, 2001, Copyright 2001 by Cell Press The TNF and TNF Receptor Review Superfamilies: Integrating Mammalian Biology Richard M. Locksley,*²³k Nigel Killeen,²k The receptors and ligands in this superfamily have and Michael J. Lenardo§k unique structural attributes that couple them directly to *Department of Medicine signaling pathways for cell proliferation, survival, and ² Department of Microbiology and Immunology differentiation. Thus, they have assumed prominent ³ Howard Hughes Medical Institute roles in the generation of tissues and transient microen- University of California, San Francisco vironments. Most TNF/TNFR SFPs are expressed in the San Francisco, California 94143 immune system, where their rapid and potent signaling § Laboratory of Immunology capabilities are crucial in coordinating the proliferation National Institute of Allergy and Infectious Diseases and protective functions of pathogen-reactive cells. National Institutes of Health Here, we review the organization of the TNF/TNFR SF Bethesda, Maryland 20892 and how these proteins have been adapted for pro- cesses as seemingly disparate as host defense and or- ganogenesis. In interpreting this large and highly active Introduction area of research, we have focused on common themes that unite the actions of these genes in different tissues. Three decades ago, lymphotoxin (LT) and tumor necro- We also discuss the evolutionary success of this super- sis factor (TNF) were identified as products of lympho- familyÐsuccess that we infer from its expansion across cytes and macrophages that caused the lysis of certain the mammalian genome and from its many indispens- types of cells, especially tumor cells (Granger et al., able roles in mammalian biology. -
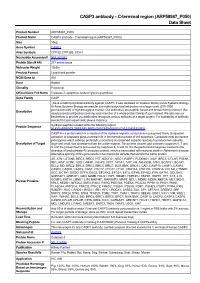
C-Terminal Region (ARP58987 P050) Data Sheet
CASP3 antibody - C-terminal region (ARP58987_P050) Data Sheet Product Number ARP58987_P050 Product Name CASP3 antibody - C-terminal region (ARP58987_P050) Size 50ug Gene Symbol CASP3 Alias Symbols CPP32; CPP32B; SCA-1 Nucleotide Accession# NM_032991 Protein Size (# AA) 277 amino acids Molecular Weight 12kDa Product Format Lyophilized powder NCBI Gene Id 836 Host Rabbit Clonality Polyclonal Official Gene Full Name Caspase 3, apoptosis-related cysteine peptidase Gene Family CASP This is a rabbit polyclonal antibody against CASP3. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Peptide Sequence Synthetic peptide located within the following region: NLKYEVRNKNDLTREEIVELMRDVSKEDHSKRSSFVCVLLSHGEEGIIFG CASP3 is a protein which is a member of the cysteine-aspartic acid protease (caspase) family. Sequential activation of caspases plays a central role in the execution-phase of cell apoptosis. Caspases exist as inactive proenzymes which undergo proteolytic processing at conserved aspartic residues to produce two subunits, Description of Target large and small, that dimerize to form the active enzyme. This protein cleaves and activates caspases 6, 7 and 9, and the protein itself is processed by caspases 8, 9 and 10. It is the predominant caspase involved in the cleavage of amyloid-beta 4A precursor protein, which is associated with neuronal death in Alzheimer's disease. -

Role of ADAM10 and ADAM17 in Regulating CD137 Function
International Journal of Molecular Sciences Article Role of ADAM10 and ADAM17 in Regulating CD137 Function Jana Seidel 1, Sinje Leitzke 1, Björn Ahrens 1, Maria Sperrhacke 1, Sucharit Bhakdi 2 and Karina Reiss 1,* 1 Department of Dermatology, University of Kiel, 24105 Kiel, Germany; [email protected] (J.S.); [email protected] (S.L.); [email protected] (B.A.); [email protected] (M.S.) 2 Independent Researcher, 24105 Kiel, Germany; [email protected] * Correspondence: [email protected] Abstract: Human CD137 (4-1BB), a member of the TNF receptor family, and its ligand CD137L (4-1BBL), are expressed on immune cells and tumor cells. CD137/CD137L interaction mediates bidirectional cellular responses of potential relevance in inflammatory diseases, autoimmunity and oncology. A soluble form of CD137 exists, elevated levels of which have been reported in patients with rheumatoid arthritis and various malignancies. Soluble CD137 (sCD137) is considered to represent a splice variant of CD137. In this report, however, evidence is presented that A Disintegrin and Metalloproteinase (ADAM)10 and potentially also ADAM17 are centrally involved in its generation. Release of sCD137 by transfected cell lines and primary T cells was uniformly inhibitable by ADAM10 inhibition. The shedding function of ADAM10 can be blocked through inhibition of its interaction with surface exposed phosphatidylserine (PS), and this effectively inhibited sCD137 generation. The phospholipid scramblase Anoctamin-6 (ANO6) traffics PS to the outer membrane and thus modifies ADAM10 function. Overexpression of ANO6 increased stimulated shedding, and hyperactive ANO6 led to maximal constitutive shedding of CD137. -

Supplementary Material and Methods
Supplementary material and methods Generation of cultured human epidermal sheets Normal human epidermal keratinocytes were isolated from human breast skin. Keratinocytes were grown on a feeder layer of irradiated human fibroblasts pre-seeded at 4000 cells /cm² in keratinocyte culture medium (KCM) containing a mix of 3:1 DMEM and HAM’s F12 (Invitrogen, Carlsbad, USA), supplemented with 10% FCS, 10ng/ml epidermal growth factor (EGF; R&D systems, Minneapolis, MN, USA), 0.12 IU/ml insulin (Lilly, Saint- Cloud, France), 0.4 mg/ml hydrocortisone (UpJohn, St Quentin en Yvelelines, France) , 5 mg/ml triiodo-L- thyronine (Sigma, St Quentin Fallavier, France), 24.3 mg/ml adenine (Sigma), isoproterenol (Isuprel, Hospira France, Meudon, France) and antibiotics (20 mg/ml gentamicin (Phanpharma, Fougères, France), 100 IU/ml penicillin (Phanpharma), and 1 mg/ml amphotericin B (Phanpharma)). The medium was changed every two days. NHEK were then cultured over a period of 13 days according to the protocol currently used at the Bank of Tissues and Cells for the generation of clinical grade epidermal sheets used for the treatment of severe extended burns (Ref). When needed, cells were harvested with trypsin-EDTA 0.05% (Thermo Fisher Scientific, Waltham, MA, USA) and collected for analysis. Clonogenic assay Keratinocytes were seeded on a feeder layer of irradiated fibroblasts, at a clonal density of 10-20 cells/cm² and cultivated for 10 to 14 days. Three flasks per tested condition were fixed and colored in a single 30 mns step using rhodamine B (Sigma) diluted at 0.01 g/ml in 4% paraformaldehyde. In each tested condition, cells from 3 other flasks were numerated after detachment by trypsin treatment. -

The Human Cytomegalovirus–Encoded Chemokine Receptor US28 Promotes Angiogenesis and Tumor Formation Via Cyclooxygenase-2
Published OnlineFirst March 24, 2009; DOI: 10.1158/0008-5472.CAN-08-2487 Research Article The Human Cytomegalovirus–Encoded Chemokine Receptor US28 Promotes Angiogenesis and Tumor Formation via Cyclooxygenase-2 David Maussang,1 Ellen Langemeijer,1 Carlos P. Fitzsimons,1 Marijke Stigter-van Walsum,2 Remco Dijkman,3 Martin K. Borg,3 Erik Slinger,1 Andreas Schreiber,4 Detlef Michel,4 Cornelis P. Tensen,3 Guus A.M.S. van Dongen,2 Rob Leurs,1 and Martine J. Smit1 1Leiden/Amsterdam Center for Drug Research, Division of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit Amsterdam; 2Department of Otolaryngology/Head and Neck Surgery, Vrije Universiteit Medical Center, Amsterdam, the Netherlands; 3Department of Dermatology, Leiden University Medical Center, Leiden, the Netherlands; and 4Institute of Virology, University Clinic Ulm, Ulm, Germany Abstract considered an oncogenic herpesvirus (5), but it has been suggested The human cytomegalovirus (HCMV), potentially associated to act as an oncomodulator (6). The presence of HCMV proteins with the development of malignancies, encodes the constitu- has been detected in several malignancies, such as colon cancer (7), tively active chemokine receptor US28. Previously, we have malignant glioblastoma (8), and breast cancer (9). Importantly, shown that US28 expression induces an oncogenic phenotype HCMV preferably infects tumor cells, leading to enhanced cell both in vitro and in vivo. Microarray analysis revealed proliferation, angiogenesis, and resistance to apoptosis (6, 10). differential expression of genes involved in oncogenic signal- Of interest, most herpesviruses contain one or more genes that ing in US28-expressing NIH-3T3 cells. In particular, the encode for constitutively active G-protein coupled receptors (1). -

MIND Bomb 2 Prevents RIPK1 Kinase Activity-Dependent and -Independent Apoptosis Through Ubiquitylation of Cflipl
ARTICLE https://doi.org/10.1038/s42003-020-01603-y OPEN MIND bomb 2 prevents RIPK1 kinase activity-dependent and -independent apoptosis through ubiquitylation of cFLIPL Osamu Nakabayashi 1, Hirotaka Takahashi2, Kenta Moriwaki1, Sachiko Komazawa-Sakon1, Fumiaki Ohtake3, 1234567890():,; Shin Murai 1, Yuichi Tsuchiya1, Yuki Koyahara1, Yasushi Saeki 4, Yukiko Yoshida4, Soh Yamazaki1, ✉ Fuminori Tokunaga 5, Tatsuya Sawasaki 2 & Hiroyasu Nakano 1 Mind bomb 2 (MIB2) is an E3 ligase involved in Notch signalling and attenuates TNF-induced apoptosis through ubiquitylation of receptor-interacting protein kinase 1 (RIPK1) and cylin- dromatosis. Here we show that MIB2 bound and conjugated K48– and K63–linked poly- ubiquitin chains to a long-form of cellular FLICE-inhibitory protein (cFLIPL), a catalytically inactive homologue of caspase 8. Deletion of MIB2 did not impair the TNF-induced complex I formation that mediates NF-κB activation but significantly enhanced formation of cytosolic death-inducing signalling complex II. TNF-induced RIPK1 Ser166 phosphorylation, a hallmark of RIPK1 death-inducing activity, was enhanced in MIB2 knockout cells, as was RIPK1 kinase activity-dependent and -independent apoptosis. Moreover, RIPK1 kinase activity-independent apoptosis was induced in cells expressing cFLIPL mutants lacking MIB2-dependent ubiqui- tylation. Together, these results suggest that MIB2 suppresses both RIPK1 kinase activity- dependent and -independent apoptosis, through suppression of RIPK1 kinase activity and ubiquitylation of cFLIPL, respectively. 1 Department of Biochemistry, Toho University School of Medicine, 5-21-16 Omori-Nishi, Ota-ku, Tokyo 143-8540, Japan. 2 Division of Cell-Free Sciences, Proteo-Science Center (PROS), 3 Bunkyo-cho, Matsuyama, Ehime 790-8577, Japan. -

TNFR2 Signaling Regulates the Immunomodulatory Function of Oligodendrocyte Precursor Cells
cells Article TNFR2 Signaling Regulates the Immunomodulatory Function of Oligodendrocyte Precursor Cells Haritha L. Desu 1, Placido Illiano 1, James S. Choi 1, Maureen C. Ascona 1, Han Gao 1,2, Jae K. Lee 1 and Roberta Brambilla 1,3,4,* 1 The Miami Project to Cure Paralysis, Department of Neurological Surgery, University of Miami Miller School of Medicine, Miami, FL 33136, USA; [email protected] (H.L.D.); [email protected] (P.I.); [email protected] (J.S.C.); [email protected] (M.C.A.); [email protected] (H.G.); [email protected] (J.K.L.) 2 Department of Spine Surgery, The Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou 510630, China 3 Department of Neurobiology Research, Institute of Molecular Medicine, and BRIDGE—Brain Research Inter Disciplinary Guided Excellence, 5000 Odense, Denmark 4 Department of Clinical Research, University of Southern Denmark, 5000 Odense, Denmark * Correspondence: [email protected]; Tel.: +305-243-3567 Abstract: Multiple sclerosis (MS) is a neuroimmune disorder characterized by inflammation, CNS demyelination, and progressive neurodegeneration. Chronic MS patients exhibit impaired remyeli- nation capacity, partly due to the changes that oligodendrocyte precursor cells (OPCs) undergo in response to the MS lesion environment. The cytokine tumor necrosis factor (TNF) is present in the MS-affected CNS and has been implicated in disease pathophysiology. Of the two active forms of TNF, transmembrane (tmTNF) and soluble (solTNF), tmTNF signals via TNFR2 mediating protective and reparative effects, including remyelination, whereas solTNF signals predominantly via TNFR1 Citation: Desu, H.L.; Illiano, P.; Choi, promoting neurotoxicity. -

Human Colon Cancer Primer Library
Human Colon Cancer Primer Library Catalog No: HCCR-1 Supplier: RealTimePrimers Lot No: XXXXX Supplied as: solid Stability: store at -20°C Description Contains 88 primer sets directed against cytokine and chemokine receptor genes and 8 housekeeping gene primer sets. Provided in a 96-well microplate (20 ul - 10 uM). Perform up to 100 PCR arrays (based on 20 ul assay volume per reaction). Just add cDNA template and SYBR green master mix. Gene List: • CCR1 chemokine (C-C motif) receptor 1 • IL11RA interleukin 11 receptor, alpha • CCR2 chemokine (C-C motif) receptor 2 • IL11RB interleukin 11 receptor, beta • CCR3 chemokine (C-C motif) receptor 3 • IL12RB1 interleukin 12 receptor, beta 1 • CCR4 chemokine (C-C motif) receptor 4 • IL12RB2 interleukin 12 receptor, beta 2 • CCR5 chemokine (C-C motif) receptor 5 • IL13RA1 interleukin 13 receptor, alpha 1 • CCR6 chemokine (C-C motif) receptor 6 • IL13RA2 interleukin 13 receptor, alpha 2 • CCR7 chemokine (C-C motif) receptor 7 • IL15RA interleukin 15 receptor, alpha • CCR8 chemokine (C-C motif) receptor 8 • IL15RB interleukin 15 receptor, beta • CCR9 chemokine (C-C motif) receptor 9 • IL17RA interleukin 17 receptor A • CCR10 chemokine (C-C motif) receptor 10 • IL17RB interleukin 17 receptor B • CX3CR1 chemokine (C-X3-C motif) receptor 1 • IL17RC interleukin 17 receptor C • CXCR1 chemokine (C-X-C motif) receptor 1 • IL17RD interleukin 17 receptor D • CXCR2 chemokine (C-X-C motif) receptor 2 • IL17RE interleukin 17 receptor E • CXCR3 chemokine (C-X-C motif) receptor 3 • IL18R1 interleukin 18 receptor -

TNF Receptor Superfamily Members RANK, RANKL, OPG Pathway As
RESEARCH ARTICLE TNF Receptor Superfamily Members RANK, RANKL, OPG Pathway as Osteoimmunological Biomarker of Bone Healing after Orthognathic Surgery İhsan O Osar1, Yavuz Fındık2, Orhan Akpinar3 ABSTRACT Tumor necrosis factor (TNF) receptor superfamily member receptor activator of nuclear factor-κB (RANK), RANK-ligand (RANKL), and osteoprotegerin (OPG) pathway as osteoimmunological biomarker of bone healing after surgery. These biomarkers play an important role in the bone repair and healing after orthognathic surgery. The aim of our study was to evaluate levels of the RANKL–RANK–OPG cytokine system as osteoimmunological biomarker of bone healing after orthognathic surgery. Receptor activator of nuclear factor-κB, RANKL, and OPG were evaluated in 25 patients who is undergoing orthognathic surgery. Blood samples were collected before the operation, after 1st day, and 10th day of the operation. Differences among OPG, RANK, and RANKL averages were not statistically significant in all time levels and operation types. In this study, we concluded that RANKL/OPG ratio and blood serum RANK levels may show bone remodeling activity and bone remodeling activity after orthognathic surgery, although there is a need for further extensive studies. Keywords: Biomarker, General anesthesia, Orthognathic surgery. International Journal of Experimental Dental Science (2020): 10.5005/jp-journals-10029-1201 INTRODUCTION 1–3Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Orthognathic surgery is the main procedure for the correction Süleyman Demirel University, Isparta, Turkey of jaw function and esthetics of the face. Orthognathic surgery Corresponding Author: Yavuz Fındık, Department of Oral and is performed on the surgeon’s bone, but the processes on the Maxillofacial Surgery, Faculty of Dentistry, Süleyman Demirel University, bone activate the bone formation and destruction events on this Isparta, Turkey, Phone: +902462113251, e-mail: yavuzfindik32@ tissue.