NIH Public Access Author Manuscript Biochem Pharmacol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Marijuana: Drug of Abuse Or Therapeutic Option? Learning Objectives
Handout for the Neuroscience Education Institute (NEI) online activity: Marijuana: Drug of Abuse or Therapeutic Option? Learning Objectives • Explain how cannabinoids affect the body and the brain • Educate patients about: – Evidence of efficacy for mental health and other conditions – Potential risks of cannabis use Timeline 1989? 90?: Discovery of ~2000 BC: binding site 2015: Elimination of Chinese 1943: Marijuana for THC— 1992: US Public Health emperors removed from CB1 Endogenous Service oversight cannabinoid recommend listing as a 1963: 1964: THC receptor for obtaining anandamide marijuana as medication in US Cannabidiol isolated marijuana for discovered medicine Pharmacopeia isolated research purposes 1995: 1851: Marijuana 1961: United 1970: Marijuana is Endogenous Aug 11 2016: listed as a Nations Single labeled Schedule I cannabinoid 2-AG DEA declines to medication in US Convention on by the US discovered reschedule Pharmacopeia Narcotic Drugs: Substance Abuse marijuana marijuana said to Act; this restricts be dangerous with both personal use no medical value and access for research purposes THE INTERSECTION OF THE HEALTHCARE AND CANNABIS INDUSTRIES What is Cannabis? 500 chemicals 100 cannabinoids Best understood: THC and CBD Scheduling of Controlled Substances No medicinal value, high Moderate to Lower High potential Low potential potential for low potential potential for for abuse for abuse abuse for abuse abuse Schedule I Schedule II Schedule III Schedule IV Schedule V Marijuana Cocaine Tylenol w/ Tramadol Robitussin AC Heroin -

Extracts and Tinctures of Cannabis
WHO Expert Committee on Drug Dependence Critical Review …………….. Extracts and tinctures of cannabis This report contains the views of an international group of experts, and does not necessarily represent the decisions or the stated policy of the World Health Organization © World Health Organization 2018 All rights reserved. This is an advance copy distributed to the participants of the 41st Expert Committee on Drug Dependence, before it has been formally published by the World Health Organization. The document may not be reviewed, abstracted, quoted, reproduced, transmitted, distributed, translated or adapted, in part or in whole, in any form or by any means without the permission of the World Health Organization. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. The World Health Organization does not warrant that the information contained in this publication is complete and correct and shall not be liable for any damages incurred as a result of its use. -

Cannabinoid Receptor and Inflammation
Cannabinoid Receptor and Inflammation Newman Osafo1, Oduro Yeboah1, Aaron Antwi1, and George Ainooson1 1Kwame Nkrumah University of Science and Technology September 11, 2020 Abstract The eventual discovery of endogenous cannabinoid receptors CB1 and CB2 and their endogenous ligands has generated interest with regards to finally understanding the endocannabinoid system. Its role in the normal physiology of the body and its implication in pathological states such as cardiovascular diseases, neoplasm, depression and pain have been subjects of scientific interest. In this review the authors focus on the endogenous cannabinoid pathway, the critical role of cannabinoid receptors in signaling and mediation of neurodegeneration and other inflammatory responses as well as its potential as a drug target in the amelioration of some inflammatory conditions. Though the exact role of the endocannabinoid system is not fully understood, the evidence found leans heavily towards a great potential in exploiting both its central and peripheral pathways in disease management. Cannabinoid therapy has already shown great promise in several preclinical and clinical trials. 1.0 Introduction Ethnopharmacological studies have shown the use of Cannabis sativa in traditional medicine for over a thousand years, with its widespread use promoted by its psychotropic effects (McCoy, 2016; Turcotte et al., 2016). The discovery of a receptor within human body, that is selectively activated by cannabinoids suggested the presence of at least one endogenous ligand for this receptor. This is confirmed by the discovery of two endogenously synthesized lipid mediators, 2-arachidonoyl-glycerol and arachidonoylethanolamide, which function as high-affinity ligands for a subfamily of cannabinoid receptors ubiquitously distributed in the central nervous system, known as the CB1 receptors (Turcotte et al., 2016). -

) (51) International Patent Classification: Columbia V5G 1G3
) ( (51) International Patent Classification: Columbia V5G 1G3 (CA). PANDEY, Nihar R.; 10209 A 61K 31/4525 (2006.01) C07C 39/23 (2006.01) 128A St, Surrey, British Columbia V3T 3E7 (CA). A61K 31/05 (2006.01) C07D 405/06 (2006.01) (74) Agent: ZIESCHE, Sonia et al.; Gowling WLG (Canada) A61P25/22 (2006.01) LLP, 2300 - 550 Burrard Street, Vancouver, British Colum¬ (21) International Application Number: bia V6C 2B5 (CA). PCT/CA2020/050165 (81) Designated States (unless otherwise indicated, for every (22) International Filing Date: kind of national protection av ailable) . AE, AG, AL, AM, 07 February 2020 (07.02.2020) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (25) Filing Language: English DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, (26) Publication Language: English HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (30) Priority Data: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 16/270,389 07 February 2019 (07.02.2019) US OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (63) Related by continuation (CON) or continuation-in-part SC, SD, SE, SG, SK, SL, ST, SV, SY, TH, TJ, TM, TN, TR, (CIP) to earlier application: TT, TZ, UA, UG, US, UZ, VC, VN, WS, ZA, ZM, ZW. US 16/270,389 (CON) (84) Designated States (unless otherwise indicated, for every Filed on 07 Februaiy 2019 (07.02.2019) kind of regional protection available) . -

The Entourage Effect of Whole-Plant Medicine
CANN BIS THE ENTOURAGE EFFECT OF Whole-Plant, WHOLE-PLANT MEDICINE Whole Medicine BY DEBORAH PARKER WONG ithin the last decade, scientists have dis- as well as the less-known such as CBDV, a proven covered hundreds of biologically active anti-epileptic. W nutrients called phytochemicals, which are Food and health researchers have long concluded found in whole, unprocessed foods. There’s pteros- that while our bodies readily absorb these kinds of tilbene, a powerful antioxidant found in almonds, nutrients from whole foods, our ability to absorb syn- blueberries and Pinot Noir grapes that enables cells thetic, isolated supplements is limited at best. That’s exactly what cannabis researchers at the Hebrew University of Jerusalem discovered when comparing the efficacy of whole-plant cannabinoid (CBD) ex- tracts with synthetic, single-molecule CBDs. As the pharmaceutical industry rushes to market synthetic CBDs, research points to what’s called the “Entourage Effect,” wherein compounds work- ing together synergistically in whole-plant medi- cines amplify the overall effects and benefits of the medicine. When comparing synthetic CBDs with whole-plant extract, the Israeli researchers ob- served a narrow therapeutic window that limits the to break down fat and cholesterol; compounds like usefulness of the synthetic form and a far greater lycopene, which colors tomatoes red, and antho- range of effectiveness for CBD-rich, whole-plant cycanin, which gives berries of all kinds their deep extract. This, combined with the Entourage Effect, hues of blue. And of course, there’s the exciting makes whole-plant CBD extracts more effective at world of phytocannabinoids, cannabis-derived com- lower doses, with fewer adverse side effects, mak- pounds including the famously psychoactive THC, ing it ideal for clinical use. -

Cannabinoid Interventions for PTSD: Where to Next?
Accepted Manuscript Cannabinoid interventions for PTSD: Where to next? Luke Ney, Allison Matthews, Raimondo Bruno, Kim Felmingham PII: S0278-5846(19)30034-X DOI: https://doi.org/10.1016/j.pnpbp.2019.03.017 Reference: PNP 9622 To appear in: Progress in Neuropsychopharmacology & Biological Psychiatry Received date: 14 January 2019 Revised date: 20 March 2019 Accepted date: 29 March 2019 Please cite this article as: L. Ney, A. Matthews, R. Bruno, et al., Cannabinoid interventions for PTSD: Where to next?, Progress in Neuropsychopharmacology & Biological Psychiatry, https://doi.org/10.1016/j.pnpbp.2019.03.017 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT 1 Cannabinoid interventions for PTSD: Where to next? Luke Ney1, Allison Matthews1, Raimondo Bruno1 and Kim Felmingham2 1School of Psychology, University of Tasmania, Australia 2School of Psychological Sciences, University of Melbourne, Australia ACCEPTED MANUSCRIPT ACCEPTED MANUSCRIPT 2 Abstract Cannabinoids are a promising method for pharmacological treatment of post- traumatic stress disorder (PTSD). Despite considerable research devoted to the effect of cannabinoid modulation on PTSD symptomology, there is not a currently agreed way by which the cannabinoid system should be targeted in humans. In this review, we present an overview of recent research identifying neurological pathways by which different cannabinoid-based treatments may exert their effects on PTSD symptomology. -
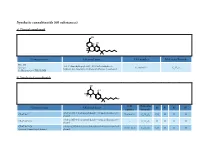
Synthetic Cannabinoids (60 Substances) A) Classical Cannabinoid
Synthetic cannabinoids (60 substances) a) Classical cannabinoid OH H OH H O Common name Chemical name CAS number Molecular Formula HU-210 3-(1,1’-dimethylheptyl)-6aR,7,10,10aR-tetrahydro-1- Synonym: 112830-95-2 C H O hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol 25 38 3 11-Hydroxy-Δ-8-THC-DMH b) Nonclassical cannabinoids OH OH R2 R3 R4 R1 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyloctan- 2- yl) CP-47,497 70434-82-1 C H O CH H H H phenol 21 34 2 3 rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylheptan- 2- yl) CP-47,497-C6 - C H O H H H H phenol 20 32 2 CP-47,497-C8 rel-2- [(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylnonan- 2- yl) 70434-92-3 C H O C H H H H Synonym: Cannabicyclohexanol phenol 22 36 2 2 5 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyldecan- 2- yl) CP-47,497-C9 - C H O C H H H H phenol 23 38 2 3 7 rel-2- ((1 R,2 R,5 R)-5- hydroxy- 2- (3- hydroxypropyl)cyclohexyl)- 3-hydroxy CP-55,940 83003-12-7 C H O CH H H 5-(2- methyloctan- 2- yl)phenol 24 40 3 3 propyl rel-2- [(1 S,3 R)-3- hydroxy-5,5-dimethylcyclohexyl]- 5- (2- Dimethyl CP-47,497-C8 - C H O C H CH CH H methylnonan-2- yl)phenol 24 40 2 2 5 3 3 c) Aminoalkylindoles i) Naphthoylindoles 1' R R3' R2' O N CAS Molecular Common name Chemical name R1’ R2’ R3’ number Formula [1-[(1- methyl- 2- piperidinyl)methyl]- 1 H-indol- 3- yl]- 1- 1-methyl-2- AM-1220 137642-54-7 C H N O H H naphthalenyl-methanone 26 26 2 piperidinyl -

Harnessing the Endocannabinoid 2-Arachidonoylglycerol to Lower Intraocular Pressure in a Murine Model
Glaucoma Harnessing the Endocannabinoid 2-Arachidonoylglycerol to Lower Intraocular Pressure in a Murine Model Sally Miller,1 Emma Leishman,1 Sherry Shujung Hu,2 Alhasan Elghouche,1 Laura Daily,1 Natalia Murataeva,1 Heather Bradshaw,1 and Alex Straiker1 1Department of Psychological and Brain Sciences, Indiana University, Bloomington, Indiana, United States 2Department of Psychology, National Cheng Kung University, Tainan, Taiwan Correspondence: Alex Straiker, De- PURPOSE. Cannabinoids, such as D9-THC, act through an endogenous signaling system in the partment of Psychological and Brain vertebrate eye that reduces IOP via CB1 receptors. Endogenous cannabinoid (eCB) ligand, 2- Sciences, Indiana University, Bloom- arachidonoyl glycerol (2-AG), likewise activates CB1 and is metabolized by monoacylglycerol ington, IN 47405, USA; lipase (MAGL). We investigated ocular 2-AG and its regulation by MAGL and the therapeutic [email protected]. potential of harnessing eCBs to lower IOP. Submitted: February 16, 2016 Accepted: May 16, 2016 METHODS. We tested the effect of topical application of 2-AG and MAGL blockers in normotensive mice and examined changes in eCB-related lipid species in the eyes and spinal Citation: Miller S, Leishman E, Hu SS, cord of MAGL knockout (MAGLÀ/À) mice using high performance liquid chromatography/ et al. Harnessing the endocannabinoid tandem mass spectrometry (HPLC/MS/MS). We also examined the protein distribution of 2-arachidonoylglycerol to lower intra- ocular pressure in a murine model. MAGL in the mouse anterior chamber. Invest Ophthalmol Vis Sci. RESULTS. 2-Arachidonoyl glycerol reliably lowered IOP in a CB1- and concentration-dependent 2016;57:3287–3296. DOI:10.1167/ manner. Monoacylglycerol lipase is expressed prominently in nonpigmented ciliary iovs.16-19356 epithelium. -

Cannabis, the Endocannabinoid System and Immunity—The Journey from the Bedside to the Bench and Back
International Journal of Molecular Sciences Review Cannabis, the Endocannabinoid System and Immunity—The Journey from the Bedside to the Bench and Back Osnat Almogi-Hazan * and Reuven Or Laboratory of Immunotherapy and Bone Marrow Transplantation, Hadassah Medical Center, The Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem 91120, Israel; [email protected] * Correspondence: [email protected] Received: 21 May 2020; Accepted: 19 June 2020; Published: 23 June 2020 Abstract: The Cannabis plant contains numerous components, including cannabinoids and other active molecules. The phyto-cannabinoid activity is mediated by the endocannabinoid system. Cannabinoids affect the nervous system and play significant roles in the regulation of the immune system. While Cannabis is not yet registered as a drug, the potential of cannabinoid-based medicines for the treatment of various conditions has led many countries to authorize their clinical use. However, the data from basic and medical research dedicated to medical Cannabis is currently limited. A variety of pathological conditions involve dysregulation of the immune system. For example, in cancer, immune surveillance and cancer immuno-editing result in immune tolerance. On the other hand, in autoimmune diseases increased immune activity causes tissue damage. Immuno-modulating therapies can regulate the immune system and therefore the immune-regulatory properties of cannabinoids, suggest their use in the therapy of immune related disorders. In this contemporary review, we discuss the roles of the endocannabinoid system in immunity and explore the emerging data about the effects of cannabinoids on the immune response in different pathologies. In addition, we discuss the complexities of using cannabinoid-based treatments in each of these conditions. -
Effects of Cannabinoids on the Development of Chick Embryos In
www.nature.com/scientificreports OPEN Efects of cannabinoids on the development of chick embryos in ovo Received: 16 April 2019 Sofa B. Gustafsson & Stig O. P. Jacobsson Accepted: 3 September 2019 We have examined the efects of the synthetic cannabinoids HU 210 and HU 211, the plant-derived Published online: 17 September 2019 cannabidiol and the endogenous cannabinoid anandamide on the viability and development of chick embryos. Fertilized White Leghorn chicken eggs were injected with the test compounds or carrier vehicle, via a drilled small hole in the egg, directly into the egg yolk. After nine days of exposure, the embryonal viability, length and wet weight of embryos, and wet weight of brains were measured, and the development stages were assessed according to the Hamburger and Hamilton (HH) scale. The potent synthetic cannabinoid receptor agonist HU 210 and the non-psychotropic cannabidiol were embryotoxic at the highest concentrations examined (10 µM and 50 µM, respectively), with no viable embryos after the HU 210 injection, and 20% viability after the cannabidiol injections. The efects of HU 210 on the chick embryo were attenuated by α-tocopherol and the cannabinoid receptor antagonist AM251, whereas only α-tocopherol gave a statistically signifcant protection against the embryotoxic efects of cannabidiol. This study shows that exposure to plant-derived or synthetic cannabinoids during early embryonal development decreases embryonal viability. Extrapolation of data across species is of course difcult, but the data would argue against the use of cannabinoids, be it recreationally or therapeutically, during pregnancy. Cannabis has a long history of medical and therapeutic use, and the discovery of the cannabinoid (CB) signalling system, comprising CB receptors, endogenous ligands and enzymes for ligand biosynthesis and inactivation, has led to an enormous expansion of the CB research feld and in turn to the identifcation of new targets for therapeutic drugs1–3. -
Synthetic Cannabinoids, Forensic & Legal Aspects
Synthetic Cannabinoids, Forensic & Legal Aspects Marilyn A. Huestis, PhD Chief, Chemistry & Drug Metabolism National Institute on Drug Abuse, National Institutes of Health Council of Forensic Medicine Istanbul, Turkey August 18, 2011 Synthetic Cannabinoid Overview Cannabinoid pharmacology Chemistry of synthetic cannabinoids Metabolism of synthetic cannabinoids Controlled drug administration studies Analytical methods for the identification of synthetic cannabinoids in biological & non-biological matrices Current legal status of synthetic cannabinoids Cannabis Mechanisms of Action THC binds to cannabinoid receptors & modulates endogenous cannabinoid & other neurotransmitter systems CB-1 receptors primarily in central nervous & cardiovascular systems CB-2 receptors primarily in immune system Non-CB1, non-CB2 receptors G-protein receptors discovered & cloned in late 1980’s Endogenous cannabinoids include anandamide, 2-AG, virodhamine, N-arachidonyl dopamine (NADA), oleamide, 2-arachidonyl glyceryl ether (noladin ether) & others High CB1 Receptor Density Hypothalamus Appetite, Hormones & Sexual behavior Neocortex High cognitive function & Sensory data Basal Ganglia integration Motor control & planning Hippocampus Memory & Learning Amygdala Anxiety, Emotion & Fear Cerebellum Brain Stem Motor control & Spinal Cord & coordination Vomiting reflex & Pain sensation Cannabinoid Mechanisms of Action Receptor distribution in brain correlates with areas involved in physiological, psychomotor & cognitive effects High density in caudate -

Cannabis Indica
Basic Information of Cannabis Chatchada Bodhibukkana, Ph.D. R&D Institute, GPO Plant Type sativa indica ruderalis Ref : https://smoke.io/strains/@jwolf/the-clear-difference-between-cannabis-sativa-indica-and-ruderalis-or-simple-photos2 Plant Type - Origin Sativa Indica Ruderalis Tropical zone, which is The dry regions with little rainfall; The Asian parts of Russia. characterized by its warm and Afghanistan, Lebanon, and the Difference in daylengths. humid climate. Hindu Kush. (approx. 19 hours of daylight in It is located 23.5 degrees above Central Asia summer & 10.5 hours of daylight and below the equator. in winter) Small difference in daylengths. (approx. 13.5 hours of daylight in Short vegetative phase (growth summer & 10.5 hours of daylight phase). in winter) Automatically switches to the flowering phase (floral phase) regardless of the season. Ref : https://www.mallorca-seeds.com/difference-sativa-indica-ruderalis/ 3 Plant Type - Origin สายพันธ์ไทย-> sativa Ref : https://smoke.io/strains/@jwolf/the-clear-difference-between-cannabis-sativa-indica-and-ruderalis-or-simple-photos4 Sativa Vs Indica Ref: https://wisetoast.com/types-of-marijuana-and-effects Ref : https://www.cannaconnection.com/blog/11392-difference-indica-sativa-ruderalis-hybrid-plants 5 Ref : https://www.amazon.com/Periodic-Table-Cannabis-Poster-Print/dp/B00MBI4HVM Cannabis Plant Anatomy Sinsemilla “without seeds” Trichomes Ref : https://herbology.org/2019/08/14/cannabis-anatomy-the-parts-of-the-plant/ Male Female Hermaphroditic Pollen sac Stigma Pollen sac + Stigma Ref : https://www.amsterdamgenetics.com/spot-male-female-hermaphrodite-cannabis/ Non cannabinoids • Terpenes • Sugars • Flavonoids • Fats • Chlorophyll • Lignin • Pigments • Starches • Waxes • Celluloses • Pectins • Etc.