Chemotherapy of Leishmaniasis – a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review Article Use of Antimony in the Treatment of Leishmaniasis: Current Status and Future Directions
SAGE-Hindawi Access to Research Molecular Biology International Volume 2011, Article ID 571242, 23 pages doi:10.4061/2011/571242 Review Article Use of Antimony in the Treatment of Leishmaniasis: Current Status and Future Directions Arun Kumar Haldar,1 Pradip Sen,2 and Syamal Roy1 1 Division of Infectious Diseases and Immunology, Indian Institute of Chemical Biology, Council of Scientific and Industrial Research, 4 Raja S. C. Mullick Road, Kolkata West Bengal 700032, India 2 Division of Cell Biology and Immunology, Institute of Microbial Technology, Council of Scientific and Industrial Research, Chandigarh 160036, India Correspondence should be addressed to Syamal Roy, [email protected] Received 18 January 2011; Accepted 5 March 2011 Academic Editor: Hemanta K. Majumder Copyright © 2011 Arun Kumar Haldar et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In the recent past the standard treatment of kala-azar involved the use of pentavalent antimonials Sb(V). Because of progressive rise in treatment failure to Sb(V) was limited its use in the treatment program in the Indian subcontinent. Until now the mechanism of action of Sb(V) is not very clear. Recent studies indicated that both parasite and hosts contribute to the antimony efflux mechanism. Interestingly, antimonials show strong immunostimulatory abilities as evident from the upregulation of transplantation antigens and enhanced T cell stimulating ability of normal antigen presenting cells when treated with Sb(V) in vitro. Recently, it has been shown that some of the peroxovanadium compounds have Sb(V)-resistance modifying ability in experimental infection with Sb(V) resistant Leishmania donovani isolates in murine model. -

T. Cruzi Invasion Summary Leishmania Phagosome
What is happening in invasion? T. cruzi invasion- non phagocytic Phagocytosis Active invasion Yeast Trypanosoma cruzi Actin filaments Lamp-1 T. cruzi invasion summary Leishmania phagosome Treatment for kinetoplastid diseases HAT Early (these drugs cannot cross the blood/brain barrier) Suramin (1916) highly charged compound Mode of action (?) - inhibits metabolic enzymes (NAD+) Pentamidine (some resistance) Mode of action (?) - likely multiple targets Differential uptake of drug - parasite conc. mM quantites Late Melarsoprol (lipophilic) (1947) Highly toxic arsenical - up to 10% treated die Mode of action (?) - possibly energy metabolism Eflornithine (drug has similar affinity to mammalian enzyme) suicide inhibitor of ornithine decarboxylase blocking polyamine biosynthesis Treatments for HAT 1985 2005 Early Stage First-line drugs Pentamidine Pentamidine Suramin Suramin Clinical trials - DB 289 (Phase III) Pre-clinical stage - - Late-stage/CNS First-line drugs Melarsoprol Melarsoprol Eflornithine Clinical trials - Nifurtimox + Eflornithine Pre-clinical stage - - Treatment for kinetoplastid diseases Chagas Acute Nifurtimox 60-90 days Mode of action (?) ROS - then DNA damage Benznidazole 30-120 days Mode of action - thought to inhibit nucleic acid synthesis (ROS?) Chronic Virtually untreatable - just treat symptoms Treatments for Chagas 1985 2005 Acute Stage First-line drugs Benznidazole Benznidazole Nifurtimox Nifurtimox Clinical trials Allopurinal Indeterminate Stage Clinical trials - Benznidazole Chronic Stage First-line drugs - -

Topical Treatment of Cutaneous Leishmaniasis
Topical Treatment of Cutaneous Leishmaniasis Joseph EI-On, Ph.D., Rita Livshin, M.D., Zvi Even-Paz, M.D. , David Hamburger, Ph.D., and Louis Weinrauch, M. D . Department of Microbio logy and Immunology, Facult y of Hea lth Sciences, Dcn G urion University of the N cgev UE-O), Deer Sheva; Departmcnt of Dcrmatology, Hadassah Universi ty H ospital, Hebrcw University Had assa h Mcdical School (R L, ZE-P, LW), j erusalem; Teva Pharm aceutica l In dustries Ltd. (01-1 ), j erusa lem, Israel Six ty- seven patients, 19 fem :ll es and 48 m ales, 4-66 years develo pments did not affect the clinical he:ding process o ld , sufferin g fro m lesions o f cutaneous leishmaniasis which was generall y completed in a period of 10-30 d ays were treated to pica ll y with an o intme nt comprising 15% after termination of trea tment. In addition, 94% of the paro m o mycin sulfate and 12% m eth ylbenzethonium chl o treated lesio n s healed with little o r no scarring. N o adverse ride in white soft pa raffin (P-ointment, U .K . patent clinica l or laboratory side effe cts w ere observed except fo r GBll7237A). After 10 d ays of treatment, twice daily, the a burning sensation at the site of trea tment. Parasites iso_ lesio ns in 72% of the treated pati ents were free of parasites, lated fro m patients w ho failed to respond to topical treat_ 15% becam e free with in an additional 20 d ays, witho ut m ent were found to be susceptible to PR-MBC I in both further trea tment, and 13% failed to respond. -

Identification and Characterization of Novel Anti-Leishmanial Compounds
Identification and Characterization of Novel Anti-leishmanial Compounds Bilal Zulfiqar Master of Philosophy, Doctor of Pharmacy Discovery Biology Griffith Institute for Drug Discovery School of Natural Sciences Griffith University Submitted in fulfilment of the requirements of the degree of Doctor of Philosophy October 2017 ABSTRACT ABSTRACT Leishmaniasis is characterized as a parasitic disease caused by the trypanosomatid protozoan termed Leishmania. Leishmaniasis is endemic in 98 countries around the globe with increased cases of morbidity and mortality emerging each day. The mode of transmission of this disease is via the bite of a sand fly, genus Phlebotomus (Old World) and Lutzomyia (New World). The life cycle of Leishmania parasite exists between the sand fly (promastigote form) and the mammalian host (amastigote form). Leishmaniasis can be characterized as cutaneous, muco-cutaneous or visceral leishmaniasis based on clinical manifestations exhibited in infected individuals. Although leishmaniasis is treatable, it faces challenges largely due to emerging resistance and extensive toxicity for current drugs. Therapeutic efficacy varies depending upon the species, symptoms and geographical regions of the Leishmania parasite. The drug discovery pipeline for neglected trypanosomatid diseases remains sparse. In particular, the field of leishmaniasis drug discovery has had limited success in translating potential drug candidates into viable therapies. Currently there are few compounds that are clinical candidates for leishmaniasis, it is therefore essential that new compounds that are active against Leishmania are identified and evaluated for their potential to progress through the drug discovery pipeline. In order to identify new therapeutics, it is imperative that robust, biologically relevant assays be developed for the screening of anti-leishmanial compounds. -

Manual for the Diagnosis and Treatment of Leishmaniasis
Republic of the Sudan Federal Ministry of Health Communicable and Non-Communicable Diseases Control Directorate MANUAL FOR THE DIAGNOSIS AND TREATMENT OF LEISHMANIASIS November 2017 Acknowledgements The Communicable and Non-Communicable Diseases Control Directorate (CNCDCD), Federal Ministry of Health, Sudan, would like to acknowledge all the efforts spent on studying, controlling and reducing morbidity and mortality of leishmaniasis in Sudan, which culminated in the formulation of this manual in April 2004, updated in October 2014 and again in November 2017. We would like to express our thanks to all National institutions, organizations, research groups and individuals for their support, and the international organization with special thanks to WHO, MSF and UK- DFID (KalaCORE). I Preface Leishmaniasis is a major health problem in Sudan. Visceral, cutaneous and mucosal forms of leishmaniasis are endemic in various parts of the country, with serious outbreaks occurring periodically. Sudanese scientists have published many papers on the epidemiology, clinical manifestations, diagnosis and management of these complex diseases. This has resulted in a better understanding of the pathogenesis of the various forms of leishmaniasis and has led to more accurate and specific diagnostic methods and better therapy. Unfortunately, many practitioners are unaware of these developments and still rely on outdated diagnostic procedures and therapy. This document is intended to help those engaged in the diagnosis, treatment and nutrition of patients with various forms of leishmaniasis. The guidelines are based on publications and experience of Sudanese researchers and are therefore evidence based. The guidelines were agreed upon by top researchers and clinicians in workshops organized by the Leishmaniasis Control response at the Communicable and Non-Communicable Diseases Control Directorate, Federal Ministry of Health, Sudan. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Redalyc.Influence of Gentamicine on the Pharmacokinetic of A
Archivos Venezolanos de Farmacología y Terapéutica ISSN: 0798-0264 [email protected] Sociedad Venezolana de Farmacología Clínica y Terapéutica Venezuela Vásquez de Ricciardi, Laura; Scorza, José Vicente; Vicuña-Fernández, Nelson; Petit de Peña, Yaneira; Bendezú, Herminia; Vasquez, Libia; Yanez, Carlos Influence of gentamicine on the pharmacokinetic of a pentavalent antimonial compound Glucantime® Influence of gentamicine on Glucantime kinetic Archivos Venezolanos de Farmacología y Terapéutica, vol. 25, núm. 2, 2006, pp. 60-63 Sociedad Venezolana de Farmacología Clínica y Terapéutica Caracas, Venezuela Disponible en: http://www.redalyc.org/articulo.oa?id=55925204 Cómo citar el artículo Número completo Sistema de Información Científica Más información del artículo Red de Revistas Científicas de América Latina, el Caribe, España y Portugal Página de la revista en redalyc.org Proyecto académico sin fines de lucro, desarrollado bajo la iniciativa de acceso abierto Influence of gentamicine on the pharmacokinetic of a pentavalent antimonial compound Glucantime® Influence of gentamicine on Glucantime kinetic Laura Vásquez de Ricciardi 1, José Vicente Scorza 2, Nelson Vicuña-Fernández 3, Yaneira Petit de Peña 4, Herminia Bendezú 5, Libia Vasquez 6, Carlos Yanez 7 1 Doctora en Ciencias Médicas. Laboratorio de Farmacología., Facultad de Medicina Escuela de Medicina Valera. ULA. 2 Doctor en Parasitología. Centro de Investigaciones Parasitológicas ¨José W. Torrealba¨ NURR. ULA. 3 Médico Especialista en Farmacocinética. Laboratorio de Farmacología y Toxicología Facultad de Medicina ULA. Mérida, Venzuela. 4 Doctora en Química. Laboratorio de Espectroscopía Molecular. Facultad de Ciencias. La Hechicera. ULA. 5 Magister en Protozoología. Centro de Investigaciones Parasitológicas ¨José W. Torrealba¨ NURR, ULA. 6 Medico Microbiologo. Laboratorio de Microbiología. -

N-Metil Glucamine and Topical Miltefosine Association In
Received: August 28, 2006 J. Venom. Anim. Toxins incl. Trop. Dis. Accepted: April 4, 2007 V.13, n.3, p.598-606, 2007. Abstract published online: April 5, 2007 Original paper. Full paper published online: August 31, 2007 ISSN 1678-9199. INEFFICACY OF THE ASSOCIATION N-METHYL GLUCAMINE AND TOPICAL MILTEFOSINE IN THE TREATMENT OF EXPERIMENTAL CUTANEOUS LEISHMANIASIS BY Leishmania (Leishmania) amazonensis SAMPAIO R. N. R. (1), LUCAS I. C. (1), TAKAMI H. L. (1) (1) Laboratory of Dermatomycology, University of Brasília, Brazil. ABSTRACT: Pentavalent antimonial (SbV) is the first treatment for cutaneous leishmaniasis (CL). Other drugs present similar side effects and higher cost. Oral miltefosine is effective to treat kala-azar. The aim of the present study was to compare the efficacy of glucamine (SbV) plus topical miltefosine with glucamine in the treatment of CL. Eighty isogenic C57BL/6 mice were inoculated with Leishmania (Leishmania) amazonensis and divided into two groups: one group was treated with SbV associated with miltefosine, and the other group received SbV plus saline solution. Groups were evaluated according to the diameter of the inoculated foot pad, the culture, and the parasite count using the limiting dilution assay. There was not statistical difference. The efficacy of glucamine in CL treatment did not increase when associated with topical miltefosine. KEY WORDS: Cutaneous Leishmaniasis, Miltefosine, N-methyl glucamine. CONFLICTS OF INTEREST: There is no conflict. CORRESPONDENCE TO: RAIMUNDA NONATA RIBEIRO SAMPAIO, Universidade de Brasília, Campus Universitário Darcy Ribeiro, Asa Norte, Brasília, 70910-900, DF, Brasil. Phone: +55 61 307 2502. Fax: +55 61 367 3825. Email: [email protected]. -

204684Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 204684Orig1s000 MEDICAL REVIEW(S) Clinical Investigator Financial Disclosure Review Template Application Number: 204684 Submission Date(s): September 27, 2012 and April 19, 2013 Applicant: Paladin Therapeutics, Inc. Product: IMPAVIDO (miltefosine) Reviewer: Hala Shamsuddin, M.D. Date of Review: February 24, 2014 Covered Clinical Study (Name and/or Number): Study 3154 Study 3168 Study Z020a and b Study SOTO Study Z022 Dutch PK study Was a list of clinical investigators provided: Yes X No (Request list from applicant) Total number of investigators identified: Six (6) Number of investigators who are sponsor employees (including both full-time and part-time employees): None Number of investigators with disclosable financial interests/arrangements (Form FDA 3455): Six (6) If there are investigators with disclosable financial interests/arrangements, identify the number of investigators with interests/arrangements in each category (as defined in 21 CFR 54.2(a), (b), (c) and (f)): Compensation to the investigator for conducting the study where the value could be influenced by the outcome of the study: None Significant payments of other sorts: None Proprietary interest in the product tested held by investigator: None Significant equity interest held by investigator in sponsor of covered study: None Is an attachment provided with details Yes X No (Request details from of the disclosable financial applicant) interests/arrangements: Is a description of the steps taken to Yes X No (Request information minimize potential bias provided: from applicant) Number of investigators with certification of due diligence (Form FDA 3454, box 3) None Is an attachment provided with the NA No (Request explanation Reference ID: 3464181 reason: from applicant) Discuss whether the applicant has adequately disclosed financial interests/arrangements with clinical investigators as recommended in the guidance for industry Financial Disclosure by Clinical Investigators. -

Pancreatic Toxicity As an Adverse Effect Induced by Meglumine Antimoniate Therapy in a Clinical Trial for Cutaneous Leishmaniasis
Rev. Inst. Med. Trop. Sao Paulo 2016;58:68 http://dx.doi.org/10.1590/S1678-9946201658068 ORIGINAL ARTICLE PANCREATIC TOXICITY AS AN ADVERSE EFFECT INDUCED BY MEGLUMINE ANTIMONIATE THERAPY IN A CLINICAL TRIAL FOR CUTANEOUS LEISHMANIASIS Marcelo Rosandiski LYRA(1), Sonia Regina Lambert PASSOS(2,5), Maria Inês Fernandes PIMENTEL(1), Sandro Javier BEDOYA-PACHECO(1), Cláudia Maria VALETE-ROSALINO(1,3,5), Erica Camargo Ferreira VASCONCELLOS(1), Liliane Fatima ANTONIO(1), Mauricio Naoto SAHEKI(1), Mariza Mattos SALGUEIRO(1), Ginelza Peres Lima SANTOS(1), Madelon Noato RIBEIRO(1), Fatima CONCEIÇÃO-SILVA(4), Maria Fatima MADEIRA(1,5), Jorge Luiz Nunes SILVA(1), Aline FAGUNDES(1) & Armando Oliveria SCHUBACH(1,6,7) SUMMARY American tegumentary leishmaniasis is an infectious disease caused by a protozoan of the genus Leishmania. Pentavalent antimonials are the first choice drugs for cutaneous leishmaniasis (CL), although doses are controversial. In a clinical trial for CL we investigated the occurrence of pancreatic toxicity with different schedules of treatment with meglumine antimoniate (MA). Seventy- two patients were allocated in two different therapeutic groups: 20 or 5 mg of pentavalent antimony (Sb5+)/kg/day for 20 or 30 days, respectively. Looking for adverse effects, patients were asked about abdominal pain, nausea, vomiting or anorexia in each medical visit. We performed physical examinations and collected blood to evaluate serum amylase and lipase in the pre-treatment period, and every 10 days during treatment and one month post-treatment. Hyperlipasemia occurred in 54.8% and hyperamylasemia in 19.4% patients. Patients treated with MA 20 mg Sb5+ presented a higher risk of hyperlipasemia (p = 0.023). -

Lack of Clinical Pharmacokinetic Studies to Optimize the Treatment of Neglected Tropical Diseases: a Systematic Review
Clin Pharmacokinet DOI 10.1007/s40262-016-0467-3 SYSTEMATIC REVIEW Lack of Clinical Pharmacokinetic Studies to Optimize the Treatment of Neglected Tropical Diseases: A Systematic Review 1 1,2 Luka Verrest • Thomas P. C. Dorlo Ó The Author(s) 2016. This article is published with open access at Springerlink.com Abstract Methods PubMed was systematically searched for all Introduction Neglected tropical diseases (NTDs) affect clinical trials and case reports until the end of 2015 that more than one billion people, mainly living in developing described the pharmacokinetics of a drug in the context of countries. For most of these NTDs, treatment is subopti- treating any of the NTDs in patients or healthy volunteers. mal. To optimize treatment regimens, clinical pharma- Results Eighty-two pharmacokinetic studies were identi- cokinetic studies are required where they have not been fied. Most studies included small patient numbers (only previously conducted to enable the use of pharmacometric five studies included [50 subjects) and only nine (11 %) modeling and simulation techniques in their application, studies included pediatric patients. A large part of the which can provide substantial advantages. studies was not very recent; 56 % of studies were published Objectives Our aim was to provide a systematic overview before 2000. Most studies applied non-compartmental and summary of all clinical pharmacokinetic studies in analysis methods for pharmacokinetic analysis (62 %). NTDs and to assess the use of pharmacometrics in these Twelve studies used population-based compartmental studies, as well as to identify which of the NTDs or which analysis (15 %) and eight (10 %) additionally performed treatments have not been sufficiently studied. -
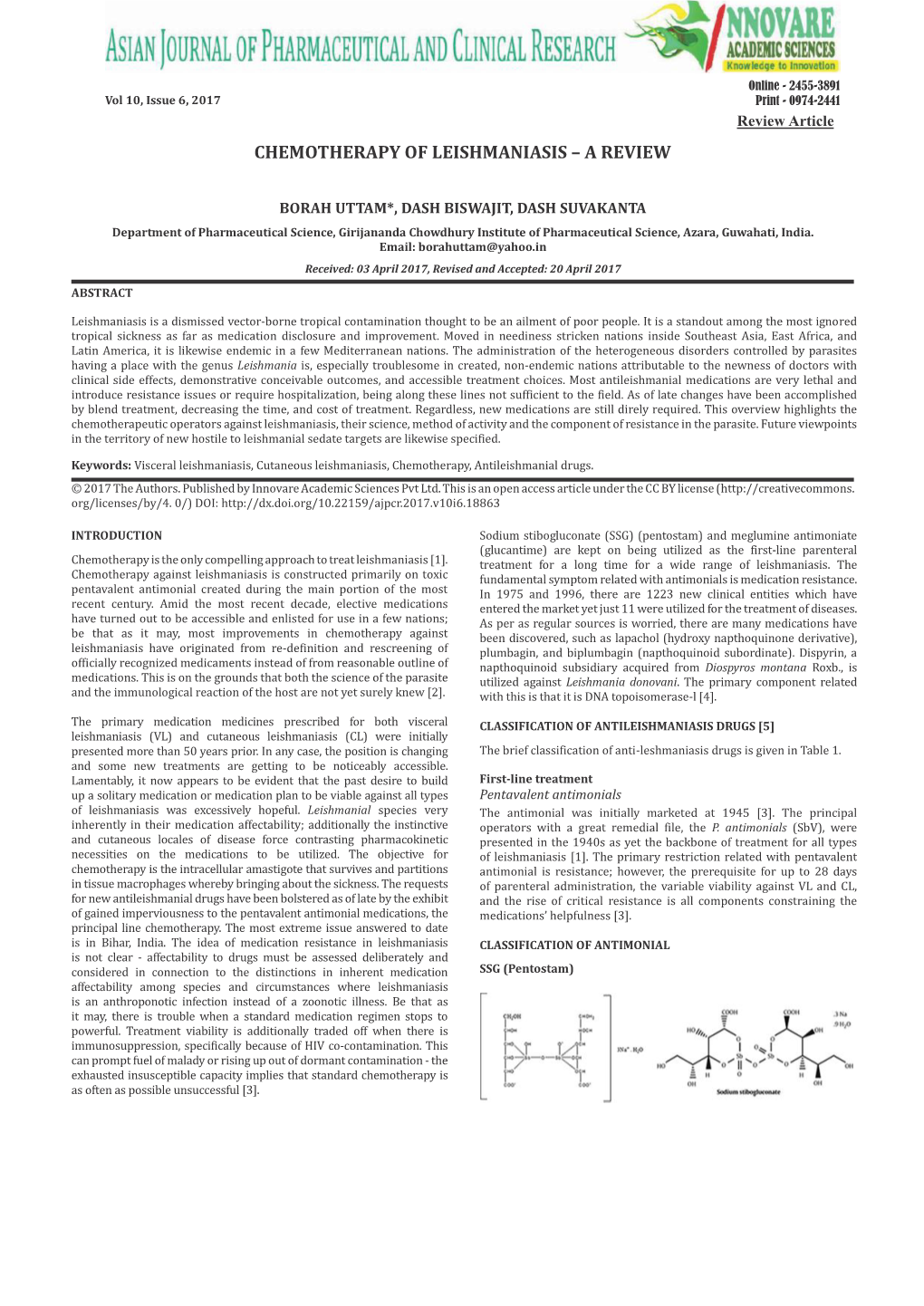
Versão Do Arquivo Anexado / Version of Attached File: Versão Do Editor / Published Version Mais Informações No Site Da Edito
UNIVERSIDADE ESTADUAL DE CAMPINAS SISTEMA DE BIBLIOTECAS DA UNICAMP REPOSITÓRIO DA PRODUÇÃO CIENTIFICA E INTELECTUAL DA UNICAMP Versão do arquivo anexado / Version of attached file: Versão do Editor / Published Version Mais informações no site da editora / Further information on publisher's website: https://www.sciencedirect.com/science/article/pii/S221132071830071X DOI: 10.1016/j.ijpddr.2018.09.006 Direitos autorais / Publisher's copyright statement: ©2018 by Elsevier. All rights reserved. DIRETORIA DE TRATAMENTO DA INFORMAÇÃO Cidade Universitária Zeferino Vaz Barão Geraldo CEP 13083-970 – Campinas SP Fone: (19) 3521-6493 http://www.repositorio.unicamp.br IJP: Drugs and Drug Resistance 8 (2018) 430–439 Contents lists available at ScienceDirect IJP: Drugs and Drug Resistance journal homepage: www.elsevier.com/locate/ijpddr Review Challenges in drug discovery targeting TriTryp diseases with an emphasis on T leishmaniasis ∗ Laura M. Alcântara, Thalita C.S. Ferreira, Fernanda R. Gadelha, Danilo C. Miguel Biology Institute, University of Campinas – UNICAMP, Campinas, São Paulo, Brazil ARTICLE INFO ABSTRACT Keywords: Tritryps diseases are devastating parasitic neglected infections caused by Leishmania spp., Trypanosoma cruzi and Chemotherapy Trypanosoma brucei subspecies. Together, these parasites affect more than 30 million people worldwide and Drug development cause high mortality and morbidity. Leishmaniasis comprises a complex group of diseases with clinical mani- Leishmania festation ranging from cutaneous lesions to systemic visceral damage. Antimonials, the first-choice drugs used to Public-private partnership treat leishmaniasis, lead to high toxicity and carry significant contraindications limiting its use. Drug-resistant Trypanosomatids parasite strains are also a matter for increasing concern, especially in areas with very limited resources.