For Personal Use Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Standard Operating Procedure Initiation And
STANDARD OPERATING PROCEDURE Title: Procedure Document Version INITIATION AND PRESCRIBING OF PALIPERIDONE No: Replaced: LONG ACTING INJECTION (PLAI) Clinical N/A 2 SOP 03 Procedure Written By: Procedure Approved By: Approved Review Page Senior Pharmacist Gurj Bhella Date: Date: Deputy Chief Pharmacist Chief Pharmacist 22/05/2018 22/05/2020 1 of 3 Objective To ensure that all prescriptions for paliperidone are initiated by consultants on a named-patient basis and that a record of all patients is kept. Scope All BCPFT consultant teams, Pharmacy Team. Procedure 1. When a patient is identified as being a candidate for paliperidone LAI, the following criteria must be fulfilled: a. The prescribing of a typical antipsychotic depot injection first line has been tried to no effect or has not been tolerated, or is not considered clinically appropriate. b. PLAI to be initiated by Consultants only and be prescribed for its licensed indication only i.e. for maintenance treatment of schizophrenia in adult patients stabilised with risperidone (Oral or LAI) or have responded to it previously. In selected adult patients with schizophrenia and previous responsiveness to oral paliperidone or risperidone, it may be used without prior stabilisation with oral treatment if psychotic symptoms are mild to moderate and a long-acting injectable treatment is needed. Patients may now be switched from oral risperidone as well as risperidone LAI. c. PLAI must be prescribed in line with the treatment guidance for the use of long acting injections contained within NICE guideline CG178 ‘Psychosis and schizophrenia in adults: treatment and management’ issued February 2014. d. Paliperidone LAI must be prescribed once each calendar month i.e.12 times a year. -

Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Adjunctive Risperidone Treatment for Antidepressant-Resistant
Supplementary Online Content Krystal JH, Rosenheck RA, Cramer JA, et al. Adjunctive risperidone treatment for antidepressant- resistant symptoms of chronic military service–related PTSD. JAMA. 2011;306(5):493-502. eTable 1. Follow-up Drugs Started After Randomization eTable 2. Baseline Medications eTable 3. Number of Different Drugs From Each Major Class Each Patient Is Taking at Baseline eTable 4. Baseline Medication Combinations eTable 5. Adverse Events eFigure 1. Product-Limit Survival Estimates With Number of Subjects at Risk eFigure 2. Percentage of Veterans at Each CAPS Severity Level at 24 Weeks, by Treatment This supplementary material has been provided by the authors to give readers additional information about their work. © 2011 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/23/2021 eTable 1. Follow-up Drugs Started After Randomization Placebo Risperidone N= 134 N= 133 Total Patients % Patients % Patients % p-value Drugs started after randomization 46 34.3 59 44.4 105 39.3 0.10 Adrenergic Drugs 4 3.0 5 3.8 9 3.4 0.75 Atenolol 0 0.0 2 1.5 2 0.7 Metoprolol 3 2.2 2 1.5 5 1.9 Propranolol 1 0.7 1 0.8 2 0.7 Opiates 22 16.4 19 14.3 41 15.4 0.73 Codeine 1 0.7 1 0.8 2 0.7 Fentanyl 3 2.2 0 0.0 3 1.1 Hydrocodone (With Or Without 13 9.7 10 7.5 23 8.6 Acetaminophen) Methadone 1 0.7 0 0.0 1 0.4 Morphine 3 2.2 2 1.5 5 1.9 Oxycodone (With Or Without 4 3.0 7 5.3 11 4.1 Acetaminophen) Tramadol 3 2.2 2 1.5 5 1.9 Psycho-Stimulants 0 0.0 2 1.5 2 0.7 0.25 Methylphenidate 0 0.0 2 1.5 2 0.7 Muscle -

PRODUCT INFORMATION Perphenazine Item No
PRODUCT INFORMATION Perphenazine Item No. 20735 CAS Registry No.: 58-39-9 HO Formal Name: 4-[3-(2-chloro-10H-phenothiazin-10-yl) N propyl]-1-piperazineethanol N Synonyms: NSC 150866, SCH 3940 MF: C21H26ClN3OS FW: 404.0 Purity: ≥98% N Cl UV/Vis.: λmax: 257, 312 nm Supplied as: A crystalline solid Storage: -20°C S Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Perphenazine is supplied as a crystalline solid. A stock solution may be made by dissolving the perphenazine in the solvent of choice, which should be purged with an inert gas. Perphenazine is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide. The solubility of perphenazine in these solvents is approximately 5, 20, and 30 mg/ml, respectively. Description 1 Perphenazine is a typical antipsychotic. It binds to dopamine D2, α1A-, α2A-, α2B-, and α2C-adrenergic, M3 muscarinic, and histamine H1 receptors (Kis = 1.4, 10, 1,848, 104.9, 85.2, 810.5 and 8 nM, respectively), as well as the serotonin (5-HT) receptor subtypes 5-HT1A, 5-HT2A, 5-HT2C, 5-HT6, and 5-HT7 (Kis = 421, 5.6, 132, 17, and 23 nM, respectively). Perphenazine (1, 5, and 10 mg/kg) enhances morphine-induced analgesia in the tail-flick and hot plate tests in rats.2 It reduces cannibalism in female mice when administered at doses of 2 and 4 mg/kg.3 Formulations containing perphenazine have been used in the treatment of schizophrenia and psychosis. References 1. -

Appendix 13C: Clinical Evidence Study Characteristics Tables
APPENDIX 13C: CLINICAL EVIDENCE STUDY CHARACTERISTICS TABLES: PHARMACOLOGICAL INTERVENTIONS Abbreviations ............................................................................................................ 3 APPENDIX 13C (I): INCLUDED STUDIES FOR INITIAL TREATMENT WITH ANTIPSYCHOTIC MEDICATION .................................. 4 ARANGO2009 .................................................................................................................................. 4 BERGER2008 .................................................................................................................................... 6 LIEBERMAN2003 ............................................................................................................................ 8 MCEVOY2007 ................................................................................................................................ 10 ROBINSON2006 ............................................................................................................................. 12 SCHOOLER2005 ............................................................................................................................ 14 SIKICH2008 .................................................................................................................................... 16 SWADI2010..................................................................................................................................... 19 VANBRUGGEN2003 .................................................................................................................... -

Datasheet Inhibitors / Agonists / Screening Libraries a DRUG SCREENING EXPERT
Datasheet Inhibitors / Agonists / Screening Libraries A DRUG SCREENING EXPERT Product Name : Aripiprazole Lauroxil Catalog Number : T14319 CAS Number : 1259305-29-7 Molecular Formula : C36H51Cl2N3O4 Molecular Weight : 660.71 Description: Aripiprazole lauroxil is cleaved by body’s enzyme esterase to N-hydroxymethyl aripiprazole (plus lauric acid) and then to aripiprazole (plus formaldehyde), no toxicity[1]. Aripiprazole lauroxil, an N-acyloxymethyl prodrug of aripiprazole, is a Long-acting injectable (LAI) typical antipsychotic for schizophrenia. Storage: 2 years -80°C in solvent; 3 years -20°C powder; Receptor (IC50) Others In vivo Activity Aripiprazole lauroxil (intravenous administration; 1.87 mg/ml) bioconversion in vivo involves the formation of an intermediate, N- hydroxymethyl aripiprazole. The in vitro data indicates a high bioconversion of aripiprazole lauroxil, thus, the concentration of N- hydroxymethyl aripiprazole observed in the animals dosed with aripiprazole lauroxil is surprisingly high[1]. Reference 1. Jann MW, et al. Long-Acting Injectable Second-Generation Antipsychotics: An Update and Comparison Between Agents.CNS Drugs. 2018 Mar;32(3):241-257. 2. Rohde M, et al. Biological conversion of aripiprazole lauroxil - An N-acyloxymethyl aripiprazole prodrug.Results Pharma Sci. 2014 May 2;4:19-25. FOR RESEARCH PURPOSES ONLY. NOT FOR DIAGNOSTIC OR THERAPEUTIC USE. Information for product storage and handling is indicated on the product datasheet. Targetmol products are stable for long term under the recommended storage conditions. Our products may be shipped under different conditions as many of them are stable in the short-term at higher or even room temperatures. We ensure that the product is shipped under conditions that will maintain the quality of the reagents. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

INVEGA SUSTENNA® (Paliperidone Palmitate)
INVEGA SUSTENNA® INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use (paliperidone palmitate) extended-release injectable suspension, for intramuscular use --------------------------- DOSAGE FORMS AND STRENGTHS --------------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION Extended-release injectable suspension: 39 mg/0.25 mL, 78 mg/0.5 mL, 117 mg/0.75 mL, These highlights do not include all the information needed to use 156 mg/mL, or 234 mg/1.5 mL (3) INVEGA SUSTENNA® safely and effectively. See full prescribing information for INVEGA SUSTENNA®. ----------------------------------- CONTRAINDICATIONS ----------------------------------- INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable Known hypersensitivity to paliperidone, risperidone, or to any excipients in suspension, for intramuscular use INVEGA SUSTENNA®. (4) Initial U.S. Approval: 2006 -----------------------------WARNINGS AND PRECAUTIONS ----------------------------- WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS • Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with WITH DEMENTIA-RELATED PSYCHOSIS Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse See full prescribing information for complete boxed warning. reactions (e.g. stroke, transient ischemic attack). (5.2) • Neuroleptic Malignant Syndrome: Manage with immediate discontinuation of Elderly patients with dementia-related psychosis treated with antipsychotic drug and close monitoring. (5.3) drugs are -

Treatment of Adult Major Depressive Disorder (MDD) Tool
Section: A B C D E F G Resources References Treatment of Adult Major Depressive Disorder (MDD) Tool This tool is designed to support primary care providers in the treatment of adult patients (≥ 18 years) who have major depressive disorder (MDD). MDD is the most prevalent depressive disorder, and approximately 7% of Canadians meet the diagnostic criteria every year.1,2 The treatment of MDD involves psychotherapy and/or pharmacotherapy. Providers should work with patients to create a treatment plan together using providers’ clinical expertise and keeping in mind the patient’s preferences, as well as the practicality, feasibility, availability and affordability of treatment. TABLE OF CONTENTS pg. 1 Section A: Overview of MDD pathway pg. 6 Section E: Complementary and alternative medicine pg. 2 Section B: Assessing suicidality and managing pg. 7 Section F: Follow-up and monitoring suicide-related behaviour pg. 9 Section G: Special patient populations pg. 3 Section C: Psychotherapy options pg. 10 Resources pg.3 Section D: Pharmacotherapy management SECTION A: Overview of MDD pathway Patient has suspected depression Talking Points It is important to provide your patient with non-judgmental care (e.g. “Being Consider unexpected life events (e.g. death in the family, diagnosed with depression is nothing to be ashamed of, it is very common and change in family status, financial crisis). Consider special many adults are diagnosed with it every year”) patient populations. • Don’t use clinical/psychiatric language (e.g. “mental health,” “psychiatric,” and/or “maladaptive”) unless the patient uses these terms first • Use understandable language for cognitive distortions (e.g. -
Product Data Sheet
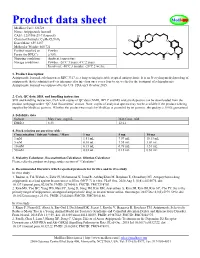
Product data sheet MedKoo Cat#: 326728 Name: Aripiprazole lauroxil CAS#: 1259305-29-7 (lauroxil) Chemical Formula: C36H51Cl2N3O4 Exact Mass: 659.3257 Molecular Weight: 660.721 Product supplied as: Powder Purity (by HPLC): ≥ 98% Shipping conditions Ambient temperature Storage conditions: Powder: -20°C 3 years; 4°C 2 years. In solvent: -80°C 3 months; -20°C 2 weeks. 1. Product description: Aripiprazole lauroxil, aslo known as RDC 3317, is a long-acting injectable atypical antipsychotic. It is an N-acyloxymethyl prodrug of aripiprazole that is administered via intramuscular injection once every four to six weeks for the treatment of schizophrenia. Aripiprazole lauroxil was approved by the U.S. FDA on 5 October 2015. 2. CoA, QC data, SDS, and handling instruction SDS and handling instruction, CoA with copies of QC data (NMR, HPLC and MS analytical spectra) can be downloaded from the product web page under “QC And Documents” section. Note: copies of analytical spectra may not be available if the product is being supplied by MedKoo partners. Whether the product was made by MedKoo or provided by its partners, the quality is 100% guaranteed. 3. Solubility data Solvent Max Conc. mg/mL Max Conc. mM DMSO 8.33 12.61 4. Stock solution preparation table: Concentration / Solvent Volume / Mass 1 mg 5 mg 10 mg 1 mM 1.51 mL 7.57 mL 15.13 mL 5 mM 0.30 mL 1.51 mL 3.03 mL 10 mM 0.15 mL 0.76 mL 1.51 mL 50 mM 0.03 mL 0.15 mL 0.30 mL 5. -

Drug Information Sheet
University Health System PSYCHIATRIC SERVICES Antipsychotics "Depot" Injectable Typical Neuroleptics Fluphenazine Decanoate (Prolixin Decanoate®) Haloperidol Decanoate (Haldol Decanoate®) Course of Treatment: _________________________________________________________________________________ PURPOSE AND GENERAL INFORMATION 1. This medication is used to treat a variety of psychiatric problems such as overactivity, preoccupation with troublesome and recurring thoughts, and unpleasant and unusual experiences such as hearing and seeing things not normally heard nor seen. This medication will reduce or stop these experiences and help you remain outside the hospital. 2. This medication cannot "cure" the illness, but it can take away many of the symptoms or make them milder. It is important to take this medication as directed, even when you begin to feel better. It is necessary to continue taking this medication in order to keep feeling well. 3. Depot medication is an alternative to taking medicine by mouth. An injection is used to deposit medication into muscle tissue and from there the medication is slowly released into your system over a number of weeks. When medication is taken by mouth, it is quickly absorbed through the stomach and intestines; unfortunately, much of it is lost in this digestive process. 4. This medication does not produce euphoria (a high feeling) and is not addictive. BENEFITS Relief of Symptoms 1. Reduction or elimination of voices or visions not heard nor seen by others. 2. Reduction or elimination of frightening or strange beliefs and ideas not shared by others. 3. Decreased tension and agitation with more calm, relaxed feelings. 4. Improved concentration and clearer thinking; better control over thoughts and feelings with less hostile, strange, or aggressive thoughts. -

Optimal Duration of Risperidone Or Olanzapine Adjunctive Therapy to Mood Stabilizer Following Remission of a Manic Episode: a CANMAT Randomized Double-Blind Trial
Molecular Psychiatry (2016) 21, 1050–1056 OPEN © 2016 Macmillan Publishers Limited All rights reserved 1359-4184/16 www.nature.com/mp ORIGINAL ARTICLE Optimal duration of risperidone or olanzapine adjunctive therapy to mood stabilizer following remission of a manic episode: A CANMAT randomized double-blind trial LN Yatham1, S Beaulieu2, A Schaffer3, M Kauer-Sant’Anna4, F Kapczinski4, B Lafer5, V Sharma6, SV Parikh7, A Daigneault8, H Qian9, DJ Bond1, PH Silverstone10, N Walji1, R Milev11, P Baruch12, A da Cunha13, J Quevedo14, R Dias5, M Kunz4, LT Young15, RW Lam1 and H Wong16 Atypical antipsychotic adjunctive therapy to lithium or valproate is effective in treating acute mania. Although continuation of atypical antipsychotic adjunctive therapy after mania remission reduces relapse of mood episodes, the optimal duration is unknown. As many atypical antipsychotics cause weight gain and metabolic syndrome, they should not be continued unless the benefits outweigh the risks. This 52-week double-blind placebo-controlled trial recruited patients with bipolar I disorder (n = 159) who recently remitted from a manic episode during treatment with risperidone or olanzapine adjunctive therapy to lithium or valproate. Patients were randomized to one of three conditions: discontinuation of risperidone or olanzapine and substitution with placebo at (i) entry (‘0-weeks’ group) or (ii) at 24 weeks after entry (‘24-weeks’ group) or (iii) continuation of risperidone or olanzapine for the full duration of the study (‘52-weeks’ group). The primary outcome measure was time to relapse of any mood episode. Compared with the 0-weeks group, the time to any mood episode was significantly longer in the 24-weeks group (hazard ratio (HR) 0.53; 95% confidence interval (CI): 0.33, 0.86) and nearly so in the 52-weeks group (HR: 0.63; 95% CI: 0.39, 1.02).