The Complex Case Discharge Delay Problem
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chcios and Eligible Lists.Xlsx
CHCIO Certified First Name Last Name Organization David Abernethy CAN Community Health Jason Adams Texas Institute for Surgery Sajid Ahmed Martin Luther King Jr. Los Angeles Healthcare Corporation Mahdi Alalmaie King Faisal Medical City for Southern Region Saad Alamri King Fahd University Hospital Nasser Alawad Sidra Medical and Reseach Center Leslie V. Albright Bethesda Hospital, Inc. Larry Allen MCR Health Services Jeffrey Allport Valley Presbyterian Hospital Abdulgader Almoeen King Faisal Specialist Hospital & Research Centre Ann Altoe Cooper University Hospital Fred Ammons Health Care Central Georgia, Inc. (Community Health Works) Isil Arican Stanford Children's Health Sallie Arnett Licking Memorial Health Systems Scott Arnold Tampa General Hospital Pamela Arora Children's Medical Center of Dallas Omer Awan Navicent Health Cara Babachicos South Shore Hospital Raymond Baker University of Kentucky HealthCare Michael Balassone MUSC Physicians Bashar Balish Pamela Banchy Western Reserve Hospital Oliver Banta Columbus Regional Healthcare Systems, Inc. Daniel Barchi New York Presbyterian Hospital Kelly Barland Health Quest Bridget Barnes Oregon Health & Sciences University Gary Barnes Medical Center Health System Brian Barnette Shepherd Center Rhonda Bartlett New York-Presbyterian Hospital Bayanmunkh Battulga Mongolian National University of Medical Services Jonathan Bauer Atlantic General Hospital Tina Baugh Menninger Clinic Lori Beeby Community Hospital Tim Belec Owensboro Health Michael Bell Texas Dept. of Criminal Justice Heath Bell -

MVP Contracted Hospitals by Health Plan Line of Business
MVP Contracted Hospitals by Health Plan Line of Business HMO ASO EPO/PPO Medicare Advantage New York Individual Standard New York Individual Non- Standard New York Small Group Exchange Medicaid/ Child Health Plus Essential Plan Aurelia Osborn Fox Memorial Hospital Oneonta NY x x x x x x x Adirondack Medical Center Saranac Lake NY x x x x x x x Albany Medical Center Hospital Albany NY x x x x x x x x x Albany Memorial Hospital Albany NY x x x x x x x x x Alice Hyde Medical Center Malone NY x x x x x x x Arnot Ogden Medical Center Elmira NY x x x x x x x x x Auburn Community Hospital Auburn NY x x x x x x x Berkshire Medical Center Pittsfield MA x x x x Bertrand Chaffee Hospital Springville NY x x x x x x Blythedale Children's Hospital Valhalla NY x x x x x Bon Secours Community Hospital Port Jervis NY x x x x x x x x x Brattleboro Memorial Hospital Brattleboro VT x x x x Buffalo General Hospital Buffalo NY x x x x x x x x x Calvary Hospital Bronx NY x Canton Potsdam Hospital Potsdam NY x x x x x x x x x Carthage Area Hospital Carthage NY x x x x x x x x x Catskill Regional Medical Center Harris NY x x x x x x x x x Cayuga Medical Center at Ithaca Ithaca NY x x x x x x x Central Vermont Medical Center Berlin VT x x x x Champlain Valley Physicians Hospital Medical Center Plattsburgh NY x x x x x x Chenango Memorial Hospital Norwich NY x x x x x x x Claxton-Hepburn Medical Center Ogdensburg NY x x x x x x x x x Clifton Fine Hospital Star Lake NY x x x x x x x x x Clifton Springs Hospital Clifton Springs NY x x x x x x x x x Cobleskill Regional -
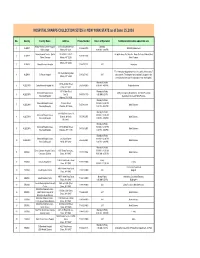
Hospital Sharps Collection Sites As of June 15 2016
HOSPITAL SHARPS COLLECTION SITES in NEW YORK STATE as of June 15,2016 No. County Facility Name Address Phone Number Hours of Operation Additional information about this site Albany Medical Center Hospital- 43 New Scotland Avenue Saturday 1 ALBANY 518-262-8700 E Building Basement Main Campus Albany, NY 12208 9:00 AM - 1:00 PM Albany Medical Center - South 25 HACKETT BLVD No public drop-off at this site. Drop off site is at Albany Med 2 ALBANY 518-262-1200 Clinical Campus Albany, NY 12208 Main Campus 600 Northern Blvd Albany, NY 12204 3 ALBANY Albany Memorial Hospital 518-471-3221 24/7 Laboratory The community sharps drop box is accessible 24 hrs a day 7 315 South Manning Blvd. 4 ALBANY St Peters Hospital 518-525-1163 24/7 days a week. The drop box is accessible if you park in the Albany, NY 12208 receiving dock and use the walkway to enter the hospital. Monday to Friday 140 West Main Street 5 ALLEGANY Cuba Memorial Hospital Inc 585-968-2000 8:00 AM - 4:00 PM Registration Area Cuba, NY 14727 191 N. Main Street Monday to Friday Memorial Hospital Jones Lobby, Emergency Department , Infection Prevention 6 ALLEGANY Box 72 585-593-1100 8:00 AM-5:00 PM Memorial Hospital Department or at each MD's Practice Andover, NY 14806 Monday to Friday Memorial Hospital Jones 15 Loder Street 9:00 AM - 12:00 PM 7 ALLEGANY 585-596-4101 Main Entrance Memorial Hospital Welsville, NY 14895 1:00 PM - 4:00 PM Monday to Friday 5877 Old State Route 19 Memorial Hospital Jones 9:00 AM - 12:00 PM 8 ALLEGANY Belmont, Wellsville 585-596-2051 Main Entrance Memorial Hospital -

An Organization That Is Delegated for Credentialing
Organizations Delegated for Credentialing Delegate Name • AdvantageCare Physicians • New York - Presbyterian Queens • Albany Medical Center • New York Eye and Ear Infirmary of Mount Sinai • Allied Pediatrics • Northwell Health • American Specialty Health (ASH) • NYC Health + Hospitals - Bellevue Hospital Center • Atlas IPA/Essen Medical Associates • NYC Health + Hospitals - Coney Island Hospital Center • Balance ACO/Corinthian IPA • NYC Health + Hospitals - Elmhurst Hospital Center • Bassett Healthcare Network • NYC Health + Hospitals - Gouverneur Health Services • Beacon Health Options • NYC Health + Hospitals - Harlem Hospital Center • BronxCare Health Systems • NYC Health + Hospitals - Kings County Hospital Center (Bronx Lebanon Hospital Center) • NYC Health + Hospitals - Lincoln Medical and Mental • Brookdale Hospital Medical Center Health Center • Brooklyn Hospital Center • NYC Health + Hospitals - Metropolitan Hospital Center • Care Management Organization (CMO Montefiore) • NYC Health + Hospitals - North Bronx Healthcare • Cayuga Medical Center Network • Charles B. Wang Community Health Center • NYC Health + Hospitals - Queens Hospital Center • Coalition of Asian-American IPA (CAIPA) • NYC Health + Hospitals -Woodhull Medical and Mental • Columbia Affiliated Physicians (CAP) Health Center • ColumbiaDoctors • NYU Langone Health • Community Health Care Network • OptumHealth - Managed Transplant Program • Cornell Medical Center IPA • Palladian Health • Crystal Run Healthcare • PHCS/Multiplan • DentaQuest • ProHEALTH Physicians • eviCore -

Community Health Initiatives Across New York State 2020 Edition About HANYS’ Community Health Improvement Award
Connecting with Communities: Community Health Initiatives Across New York State 2020 Edition About HANYS’ Community Health Improvement Award HANYS established the Community Health Improvement Award in 1997 to recognize outstanding initiatives aimed at improving the health and well-being of communities. The award is presented to member hospitals and health systems for their programs that target specific community health needs related to the New York State Prevention Agenda, demonstrate leadership, collaborate among diverse groups and, most importantly, achieve quantifiable results. THANK YOU TO OUR 2020 REVIEWERS: Sylvia Pirani (retired), former director, Office of Public Health Practice, NYSDOH Julia Resnick, MPH, senior program manager, The Value Initiative, American Hospital Association Julie Trocchio, senior director, community benefit and continuing care, Catholic Health Association of the United States Connecting with Communities 2020 | © 2020 Healthcare Association of New York State, Inc. Community Health Initiatives Across New York State 2020 Edition HANYS is pleased to present the 24th edition of Connecting with Communities: Community Health Initiatives across New York State. This publication highlights the winner and nominations for HANYS’ 2020 Community Health Improvement Award. HANYS’ Community Health Improvement Award recog- nizes member hospitals and healthcare systems for engaging key community stakeholders to implement programs to improve the health of their communities. Hospitals and healthcare systems collaborate in many ways with a variety of partners to achieve shared commu- nity health goals. The initiatives described in this publication are directly linked to the priorities of the New York State Prevention Agenda. The Prevention Agenda aims to make New York the healthiest state for people of all ages and to serve as a blueprint for local community health improvement. -

Designation of Regents Physician Shortage Areas (Rpsas)
THE STATE EDUCATION DEPARTMENT / THE UNIVERSITY OF THE STATE OF NEW YORK / ALBANY, NY 12234 TO: The Honorable the Members of the Board of Regents FROM: Douglas E. Lentivech SUBJECT: Designation of Regents Physician Shortage Areas (RPSAs) DATE: December 1, 2016 AUTHORIZATION(S): SUMMARY Issue for Consent Agenda Should the Board of Regents approve the updates to the list of Regents Physician Shortage Areas as recommended by the Department of Health? Reason(s) for Consideration Required by State Statute. Proposed Handling This item will come before the full Board at its December 2016 meeting where it will be voted on and action taken. Procedural History The Department of Health annually recommends updates to the list of Regents physician shortage areas. These updates include modifications to the following: Health Professions Shortage Areas (HPSAs) – Primary Care Shortage Areas, Facility Physician Shortage Areas, State Facility Shortage Areas, and Mental Health Professions Shortage Areas. Background Information In 1987, the Board of Regents approved a system for identifying and designating areas of physician shortage. In September 1995, the Board made a decision to update the shortage area list once a year. In addition, at its September 1997 meeting, the Board of Regents modified the system by adding a category of Mental Health Professions Shortage Areas, along with the following categories of shortage areas: Health Professions Shortage Areas (HPSAs) Federal Health Professions Shortage Areas (HPSAs) are used by the Federal government to identify areas of primary care physician shortages. The Federal government requires that all HPSA designations be updated every three years using the HPSA criteria. -

APPENDICES—Emerging Issues in Medicaid Payment and Delivery
Appendix A Thought Leaders and Stakeholders Interviewed National thought leaders Lindsey Browning, Senior Policy Analyst, National Association of Medicaid Directors Sophia Chang, Vice President of Programs, California Health Care Foundation Beth Feldpush, Senior Vice President of Policy and Advocacy, America’s Essential Hospitals Eliot Fishman, Director, State Demonstrations Group, Center for Medicaid and CHIP Services, Centers for Medicare and Medicaid Services Heather Howard, Program Director, State Health Reform Assistance Network, Robert Wood Johnson Foundation Frederick Isasi, Division Director, Health Division, National Governor’s Association Center for Best Practices Kathleen Nolan, Managing Principal, Health Management Associates (Director, State Policy and Programs, National Association of Medicaid Directors at time of interview) Chris Perrone, Director, Improving Access, California Health Care Foundation Trish Riley, Executive Director, National Academy for State Health Policy Matt Salo, Executive Director, National Association of Medicaid Directors Bruce Siegel, President and CEO, America’s Essential Hospitals Hemi Tewarson, Program Director, Health Division, National Governors Association Center for Best Practices New York stakeholders Gregory Allen, Director, Division of Program Development and Management, Office of Health Insurance Programs, New York State Department of Health Gary Belkin, Executive Deputy Commissioner for Mental Health, New York City Department of Health and Mental Hygiene Marc Berg, Principal, Health Care -

REGENTS DESIGNATED PHYSICIAN SHORTAGE AREAS in NEW YORK
REGENTS DESIGNATED PHYSICIAN SHORTAGE AREAS In NEW YORK STATE The University of the State of New York THE STATE EDUCATION DEPARTMENT Office of Access, Equity and Community Engagement Services Scholarships and Grants Administration Unit Room 967, Education Building Addition Albany, NY 12234 Effective March 15, 2021 THE UNIVERSITY OF THE STATE OF NEW YORK Regents of The University LESTER W. YOUNG, JR., Chancellor, B.S., M.S., Ed.D. .................................................. Beechhurst ROGER TILLES, B.A., J.D. ................................................................................................. Manhasset CHRISTINE D. CEA, B.A., M.A., Ph.D. ........................................................................... Staten Island WADE S. NORWOOD, B.A. ............................................................................................... Rochester KATHLEEN M. CASHIN, B.S., M.S., Ed.D. ...................................................................... Brooklyn JAMES E. COTTRELL, B.S., M.D. ....................................................................................... New York JOSEPHINE VICTORIA FINN, B.A., J.D. ............................................................................. Monticello JUDITH CHIN, M.S. in Ed. ............................................................................................... Little Neck BEVERLY L. OUDERKIRK, B.S. in Ed., M.S. in Ed. .......................................................... Morristown CATHERINE COLLINS, R.N., N.P., B.S., M.S. in Ed., Ed.D. .......................................... -

Saving Medicaid $213 Million by Capping Hospital Salaries, Not Patients’ Rights
Center for Justice & Democracy 90 Broad Street, Suite 401 New York, NY 10004 Tel: 212.267.2801 [email protected] http://centerjd.org SAVING MEDICAID $213 MILLION BY CAPPING HOSPITAL SALARIES, NOT PATIENTS’ RIGHTS March 22, 2011 On January 5, 2011, Governor Andrew M. Cuomo established a Medicaid Redesign Team (MRT) to provide the Governor with Medicaid reform “findings and recommendations for consideration in the budget process of New York State Fiscal Year 2011-12.”1 This Team was dominated by hospital and industry lobbyists, with consumer or patient advocates mostly excluded. Among the original 274 ideas distributed to MRT on February 9, 2011,2 was proposal 261, which would have limited multi-million dollar hospital executive salaries. The proposal was killed for reasons that remain unclear, although perhaps not surprising given the make-up of the Medicaid Redesign Team. In a March 25, 2011 article about multi-million dollar hospital CEO salaries, New York Times reporter Jim Dwyer wrote: A proposal to allow public financing for only the first $1 million in wages for an executive died before it even reached the task force. “It was classic how it was killed,” said Judy Wessler, director of the Commission on the Public’s Health System, an advocacy group that had suggested the limits. “We submitted the proposal in writing, met with the state staff members about it, then testified for our two minutes at a hearing,” Ms. Wessler said. “Then in the written summary of all the 4,000 proposals, they twisted the wording of ours so that it would be impossible to implement. -

Fleecing Patients: Hospitals Charge Patients More Than Four Times the Cost of Care
Fleecing Patients Hospitals Charge Patients More Than Four Times the Cost of Care November 2020 www.NationalNursesUnited.org Fleecing Patients Hospitals Charge Patients More Than Four Times the Cost of Care TABLE OF CONTENTS Summary of Findings 5 Introduction 6 Health Expenditures and the U.S. Economy 8 Rising Hospital Profits 12 Rising Hospital Prices 13 Charge-to-Cost Ratio in the United States 14 Charge-to-Cost Ratio Among Hospital Systems 19 Higher CCRs Correspond to Higher Net Income 21 Highest CCRs by State and Region 23 Beyond Charges: Other Hospital Practices to Maximize Profit 24 Conclusion 26 Appendices 27 Endnotes 88 Fleecing Patients » November 2020 3 LIST OF FIGURES AND APPENDICES Figure 1. U.S. Gross Domestic Product, 1999–2018 (page 8) Figure 2. National Health Expenditures, 1999–2018 (page 9) Figure 3. National Health Expenditure as Percentage of National Gross Domestic Product, 1999–2018 (page 9) Figure 4. National Health Expenditures Components, 2018 (page 10) Figure 5. National Hospital Expenditures, 1999–2018 (page 11) Figure 6. National Hospital Expenditures as Percentage of Health Expenditures, 1999–2018 (page 11) Figure 7. U.S. Hospitals’ Net Income, 1999–2018 (page 12) Figure 8. U.S. Hospitals’ Net Income, 1999–2018, Table (page 12) Figure 9. Consumer Price Index for Outpatient, Inpatient, and Medical Care, 1999–2018 (page 13) Figure 10. U.S. Hospitals’ Average Charge-to-Cost Ratio, 1999–2018 (page 15) Figure 11. System Owners of the Top 100 Hospitals by CCR (page 16) Figure 12. Charge-to-Cost Ratio by Provider Control Type, 2018 (page 17) Figure 13. -
COVID-19 Vaccination Details for Hospitals
Hospital Reported HERDS Data as of 9/21/2021 % of Hospital Workers with completed Region County Hospital Network vaccine series Statewide 84% Capital Region Albany Albany Medical Center Hospital Albany Medical Center 91% Capital Region Albany St Peters Hospital St. Peters Health Partners 90% Capital Region Columbia Columbia Memorial Hospital Albany Medical Center 83% Capital Region Rensselaer Samaritan Hospital St. Peters Health Partners 90% Capital Region Saratoga Saratoga Hospital Albany Medical Center 94% Capital Region Schenectady Ellis Hospital Independent 91% Capital Region Warren Glens Falls Hospital Independent 91% Central New York Cayuga Auburn Memorial Hospital Independent 80% Central New York Cortland Guthrie Cortland Medical Center The Guthrie Clinic 83% Central New York Madison Community Memorial Hospital Inc Crouse Health 82% Central New York Madison Oneida Health Hospital Independent 87% Central New York Onondaga Crouse Hospital Crouse Health 90% Central New York Onondaga St Josephs Hospital Health Center Trinity 77% Central New York Onondaga University Hospital Suny Health Science Center Independent 88% Central New York Onondaga Upstate University Hospital At Community General Independent 82% Central New York Oswego Oswego Hospital Independent 87% Finger Lakes Genesee United Memorial Medical Center Bank Street Campus Rochester Regional Health System 81% Finger Lakes Genesee United Memorial Medical Center North Street Campus Rochester Regional Health System 77% Finger Lakes Livingston Nicholas H Noyes Memorial Hospital University -
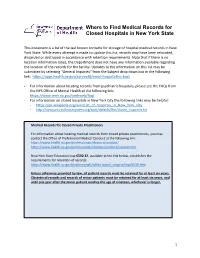
Where to Find Medical Records for Closed Hospitals in New York State
Where to Find Medical Records for Closed Hospitals in New York State This document is a list of the last known contacts for storage of hospital medical records in New York State. While every attempt is made to update this list, records may have been relocated, discarded or destroyed in accordance with retention requirements. Note that if there is no location information listed, the Department does not have any information available regarding the location of the records for the facility. Updates to the information on this list may be submitted by selecting “General Inquiries” from the Subject drop down box in the following link: https://apps.health.ny.gov/surveyd8/email-hospdtc#no-back - For information about locating records from psychiatric hospitals, please see the FAQs from the NYS Office of Mental Health at the following link: https://www.omh.ny.gov/omhweb/faq/ - For information on closed hospitals in New York City the following links may be helpful: - https://en.wikipedia.org/wiki/List_of_hospitals_in_New_York_City - http://newyork.resiliencesystem.org/sites/default/files/closed_hospitals.txt Medical Records for Closed Private Practitioners For information about locating medical records from closed private practitioners, you may contact the Office of Professional Medical Conduct at the following link: https://www.health.ny.gov/professionals/doctors/conduct/ https://www.health.ny.gov/professionals/doctors/conduct/contact.htm New York State Education Law 6530.32, available at the link below, establishes the requirements for retention of records: https://www.health.ny.gov/professionals/office-based_surgery/law/6530.htm Unless otherwise provided by law, all patient records must be retained for at least six years.