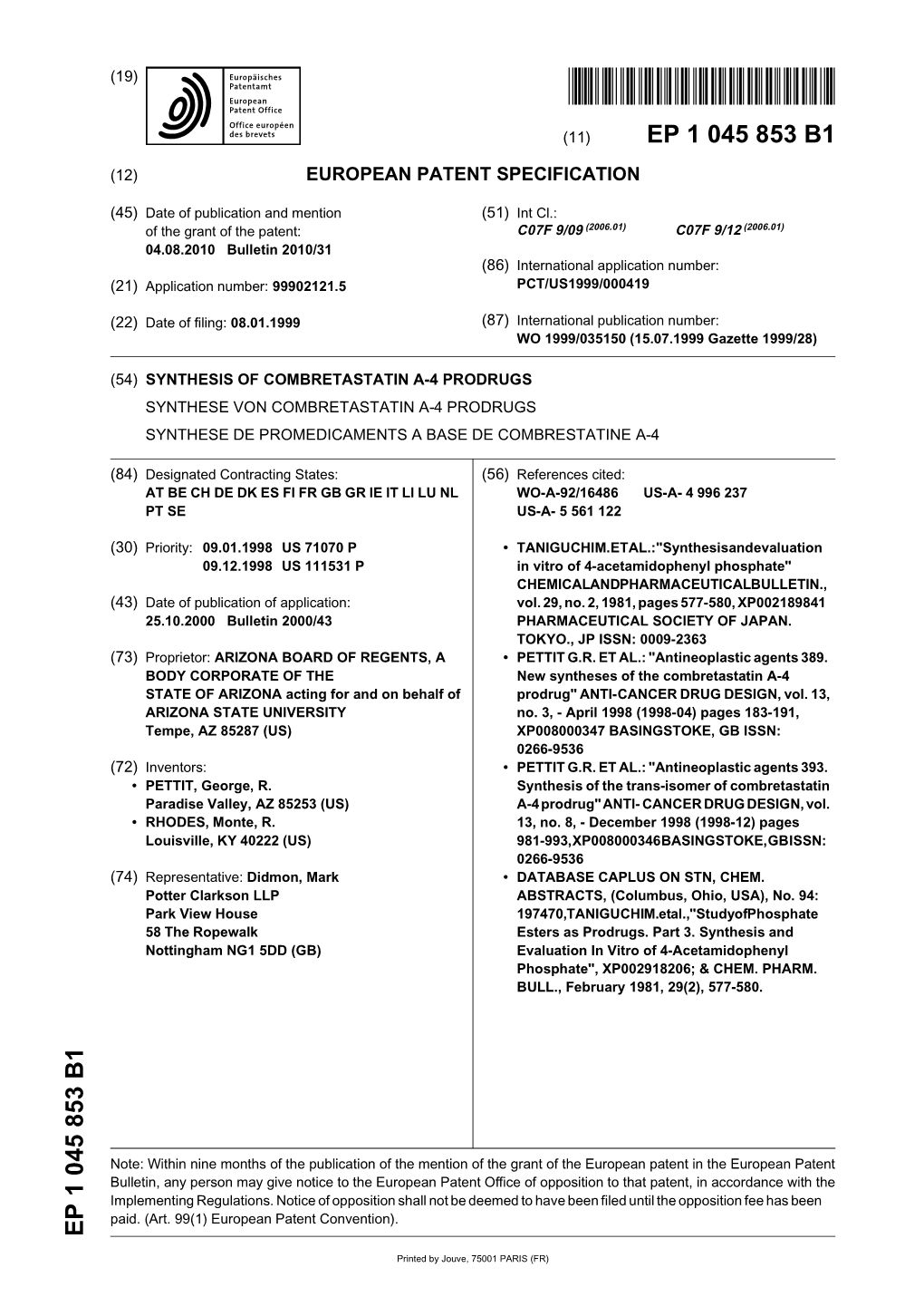
Synthesis of Combretastatin A-4 Prodrugs Synthese Von Combretastatin A-4 Prodrugs Synthese De Promedicaments a Base De Combrestatine A-4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Durham E-Theses
Durham E-Theses Meisenheimer complexes: some structural, equilibrium and kinetic studies Khan, Hassan Akhtar How to cite: Khan, Hassan Akhtar (1973) Meisenheimer complexes: some structural, equilibrium and kinetic studies, Durham theses, Durham University. Available at Durham E-Theses Online: http://etheses.dur.ac.uk/8740/ Use policy The full-text may be used and/or reproduced, and given to third parties in any format or medium, without prior permission or charge, for personal research or study, educational, or not-for-prot purposes provided that: • a full bibliographic reference is made to the original source • a link is made to the metadata record in Durham E-Theses • the full-text is not changed in any way The full-text must not be sold in any format or medium without the formal permission of the copyright holders. Please consult the full Durham E-Theses policy for further details. Academic Support Oce, Durham University, University Oce, Old Elvet, Durham DH1 3HP e-mail: [email protected] Tel: +44 0191 334 6107 http://etheses.dur.ac.uk MEISENHEIMER COMPLEXES: SOME STRUCTURAL, EQUILIBRIUM AND KINETIC STUDIES by HASSAN AKHTAR KHAN M.Sc. (Pakistan) A thesis submitted for the degree of Doctor of Philosophy in the University of Durham. JUNE 1973 Chemistry Department 1 6 JUL 1973 SEOriON ACKNOWLEDGEMENTS It is with gratitude that I thank my supervisor, Dr. M.R. Crampton, for his inspiration, generous help and encouragement throughput the course of this work. I would also like to thank the many staff members and technical staff of the department for their co-operation. -

A Publication of Reliable Methods for the Preparation of Organic Compounds
A Publication of Reliable Methods for the Preparation of Organic Compounds Working with Hazardous Chemicals The procedures in Organic Syntheses are intended for use only by persons with proper training in experimental organic chemistry. All hazardous materials should be handled using the standard procedures for work with chemicals described in references such as "Prudent Practices in the Laboratory" (The National Academies Press, Washington, D.C., 2011; the full text can be accessed free of charge at http://www.nap.edu/catalog.php?record_id=12654). All chemical waste should be disposed of in accordance with local regulations. For general guidelines for the management of chemical waste, see Chapter 8 of Prudent Practices. In some articles in Organic Syntheses, chemical-specific hazards are highlighted in red “Caution Notes” within a procedure. It is important to recognize that the absence of a caution note does not imply that no significant hazards are associated with the chemicals involved in that procedure. Prior to performing a reaction, a thorough risk assessment should be carried out that includes a review of the potential hazards associated with each chemical and experimental operation on the scale that is planned for the procedure. Guidelines for carrying out a risk assessment and for analyzing the hazards associated with chemicals can be found in Chapter 4 of Prudent Practices. The procedures described in Organic Syntheses are provided as published and are conducted at one's own risk. Organic Syntheses, Inc., its Editors, and its Board of Directors do not warrant or guarantee the safety of individuals using these procedures and hereby disclaim any liability for any injuries or damages claimed to have resulted from or related in any way to the procedures herein. -

EICG-Hot Spots: EICG Appendix C
INFORMAL REVIEW DRAFT [Note: The pre-existing regulation text is set forth below in normal type. The original proposed amendments are shown in underline to indicate additions and strikeout to indicate deletions. Additional proposed modifications are shown in double-underline to indicate additions and double-strikeout to indicate deletions. The square brackets “[ ]” are used to indicate minor adjustments to text (e.g., page numbers and adoption dates) that will be updated upon adoption of the proposed amendments.] APPENDIX C FACILITY GUIDELINE INDEX (FACILITY "LOOK-UP" TABLE) INFORMAL REVIEW DRAFT This Page Intentionally Left Blank INFORMAL REVIEW DRAFT APPENDIX C - I RESPONSIBILITIES OF ALL FACILITIES INFORMAL REVIEW DRAFT NOTES FOR APPENDIX CFACILITY GUIDELINE INDEX APPENDIX C-I RESPONSIBILITIES OF ALL FACILITIES NOTHING IN THIS APPENDIX SHALL BE CONSTRUED AS REQUIRING THAT SOURCE TESTING BE CONDUCTED FOR SUBSTANCES SET FORTH IN THIS APPENDIX. FURTHER, IN CASES WHERE A SUBSTANCE SET FORTH HEREIN IS NOT PRESENT AT A PARTICULAR FACILITY, THE FACILITY OPERATOR SHALL NOT ATTEMPT TO QUANTIFY THE EMISSIONS OF SUCH SUBSTANCE, BUT SHALL PROVIDE ADEQUATE DOCUMENTATION TO DEMONSTRATE TO THE DISTRICT THAT THE POSSIBLE PRESENCE OF THE SUBSTANCE AT THE FACILITY HAS BEEN ADDRESSED AND THAT THERE ARE NO EMISSIONS OF THE SUBSTANCE FOR SPECIFIED REASONS. Substances emitted by a particular device or process may not be limited to those listed in this Facility Guideline Index. THIS APPENDIX IS NOT AN EXHAUSTIVE LIST. ALL FACILITIES ARE RESPONSIBLE FOR IDENTIFYING AND ACCOUNTING FOR ANY LISTED SUBSTANCE USED, MANUFACTURED, FORMULATED, OR RELEASED. This Facility Guideline Index is arranged in alphabetical order. The first part of the index, Appendix C-I, lists devices common to many industries and the second part of the index, Appendix C-II, lists industry types. -

SODIUM METHOXIDE, 30% in Methanol
AKS761.5 - SODIUM METHOXIDE, 30% in methanol SODIUM METHOXIDE, 30% in methanol Safety Data Sheet AKS761.5 Date of issue: 10/26/2016 Version: 1.0 SECTION 1: Identification 1.1. Product identifier Product name : SODIUM METHOXIDE, 30% in methanol Product code : AKS761.5 Product form : Mixture Physical state : Liquid Formula : CH3NaO Synonyms : SODIUM METHYLATE METHANOL, SODIUM SALT Chemical family : METAL ALCOHOLATE 1.2. Recommended use of the chemical and restrictions on use Recommended use : Chemical intermediate For research and industrial use only 1.3. Details of the supplier of the safety data sheet GELEST, INC. 11 East Steel Road Morrisville, PA 19067 USA T 215-547-1015 - F 215-547-2484 - (M-F): 8:00 AM - 5:30 PM EST [email protected] - www.gelest.com 1.4. Emergency telephone number Emergency number : CHEMTREC: 1-800-424-9300 (USA); +1 703-527-3887 (International) SECTION 2: Hazard(s) identification 2.1. Classification of the substance or mixture GHS-US classification Flammable liquids Category 3 H226 Acute toxicity (oral) Category 3 H301 Acute toxicity (dermal) Category 3 H311 Acute toxicity (inhalation:vapor) Category 3 H331 Skin corrosion/irritation Category 1B H314 Serious eye damage/eye irritation Category 1 H318 Specific target organ toxicity (single exposure) Category 1 H370 Specific target organ toxicity (single exposure) Category 3 H336 Full text of H statements : see section 16 2.2. Label elements GHS-US labeling Hazard pictograms (GHS-US) : GHS02 GHS05 GHS06 GHS07 GHS08 Signal word (GHS-US) : Danger Hazard statements (GHS-US) : H226 - Flammable liquid and vapor H301+H311+H331 - Toxic if swallowed, in contact with skin or if inhaled H314 - Causes severe skin burns and eye damage H318 - Causes serious eye damage H336 - May cause drowsiness or dizziness H370 - Causes damage to organs Precautionary statements (GHS-US) : P280 - Wear protective gloves/protective clothing/eye protection/face protection P307 + P311 - If exposed: Call a poison center/doctor P210 - Keep away from heat, open flames, sparks. -

Alkoxylated Fatty Esters and Derivatives from Natural
(19) TZZ ¥¥ZZ_T (11) EP 2 633 008 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07C 211/00 (2006.01) 20.03.2019 Bulletin 2019/12 (86) International application number: (21) Application number: 11838497.3 PCT/US2011/057595 (22) Date of filing: 25.10.2011 (87) International publication number: WO 2012/061092 (10.05.2012 Gazette 2012/19) (54) ALKOXYLATED FATTY ESTERS AND DERIVATIVES FROM NATURAL OIL METATHESIS ALKOXYLIERTE FETTESTER UND DERIVATE AUS EINER ERDÖLMETATHESE ESTERS GRAS ALCOXYLÉS ET DÉRIVÉS À PARTIR DE LA MÉTATHÈSE D’HUILES NATURELLES (84) Designated Contracting States: • HOLLAND, Brian AL AT BE BG CH CY CZ DE DK EE ES FI FR GB Deerfield GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO IL 60015 (US) PL PT RO RS SE SI SK SM TR • MALEC, Andrew, D. Chicago (30) Priority: 25.10.2010 US 406556 P IL 60657 (US) 25.10.2010 US 406570 P • MASTERS, Ronald, A. 25.10.2010 US 406547 P Glenview IL 60025 (US) (43) Date of publication of application: • MURPHY, Dennis, S. 04.09.2013 Bulletin 2013/36 Libertyville IL 60048 (US) (73) Proprietor: Stepan Company •SKELTON,Patti Northfield, Illinois 60093 (US) Winder GA 30680 (US) (72) Inventors: • SOOK, Brian • ALLEN, Dave, R. Lawrenceville Chicago GA 30045 (US) IL 60610 (US) • WIESTER, Michael •ALONSO,Marcos Chicago Chicago IL 60625 (US) IL 60645-4922 (US) • WOLFE, Patrick, Shane • BERNHARDT, Randal, J. Palatine Antioch IL 60074 (US) IL 60002 (US) • BROWN, Aaron (74) Representative: Müller, Christian Stefan Gerd Chicago ZSP Patentanwälte -

Acroseal Packaging Your Solution for Air- and Moisture- Sensitive Reagents
AcroSeal Packaging Your solution for air- and moisture- sensitive reagents Extra dry solvents Deuterated solvents Organometallic compounds Reagents in solution Organics Introduction Since the launch of AcroSealTM packaging we have introduced a new septum, which helps preserve product quality for longer. In addition, our AcroSeal portfolio has been expanded to include a broad range of solvents, organometallics, reagents in solution and organic compounds. In this brochure we have categorized our products under chemical families to make it easier to locate the product you need. Introduction Page no. AcroSeal packaging highlights 3 AcroSeal packaging performance 4 New 25mL AcroSeal packaging 4 Solvents Extra dry solvents 5-7 Solvents for biochemistry 7 Deuterated solvents 7 Organometallics Grignard reagents 8-10 Organoaluminiums 11 Organolithiums 11 Organosodiums 12 Organotins 12 Organozincs 12 Reagents in solution Amines 13 Boranes 13 Halides 14-15 Hydrides 15 Oxides 16 Silanes 16 Other reagents in solution 17 Organics Aldehydes 18 Amines 18 Epoxides 18 Halides 19 Phosphines 19 Silanes 19 Other organics 20 How to use AcroSeal packaging 21 Alphabetical index 22-23 2 Introduction AcroSeal packaging: drier reagents for longer When using air- and moisture-sensitive solvents and reagents, it is essential that these products are not only as dry as possible when you first use them, but they should remain dry in storage as well. Through the innovative quadrant-style screw cap and specially designed septum, AcroSeal packaging ensures that you have access to high-quality and low-moisture products every use, guaranteeing improved yield and consistency of your research experiments while reducing chemical waste. AcroSeal packaging highlights New septum developed from a polymeric elastomer with an inert fluoropolymer-coated surface, preserves product quality for longer with better re-seal around needle punctures. -

A Proposed Radical-Chain Pathway for Photoinitiated Reductive
A PROPOSED RADICAL- CHAIN PATHWAY FOR PHOTOINITIATED REDUCTIVE- DEHALOGENATION AND SUBSTITUTION REACTIONS OF HETARYL AND ARYL HALIDES IN METHANOLIC METHOXIDE By GEORGE ALLISON LOCKO A DISSERTATION PRESENTED TO THE GRADUATE COUNCIL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIPJIMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 1976 UNIVERSITY OF FLORIDA 3 1262 08552 5797 To Mom and Dad ACKNOWLEDGEMENTS The author wishes to express sincere gratitude to Dr. John A. Zoltewicz, Chairman of his Supervisory Committee, for his guidance during the course of the research which is reported herein. Without the keen insight of Dr. Zoltewicz much of this work would not have been possible. Apprecia- tion is also expressed toward the other members of his committee: Dr. William R. Dolbier, Dr. Paul Tarrant, Dr. Kuang-Pang Li, and Dr. Charles Allen, Jr. The author is very grateful to Ms. Ann Kennedy for the long hours which she spent typing the manuscript. Very special thanks are extended to Sara for her love, patience, and understanding. Ill TABLE OF CONTENTS Page ACKNOWLEDGEMENTS iii LIST OF TABLES vii LIST OF FIGURES xiii ABSTRACT xvi CHAPTER: I. INTRODUCTION MECHANISTIC INVESTIGATIONS INVOLVING THE PHOTOINITIATED RADICAL-CHAIN RE- DUCTIVE- DEHALOGENATION AND PHOTOINITI- ATED SRi^jl REACTION OF 3-IODOPYRIDINE WITH THIOPHENOXIDE ION IC Results 10 Discussion 58 STRUCTURE-REACTIVITY CORRELATIONS AND RELATED INVESTIGATIONS PERTAINING TO THE PHOTOINITIATED REACTIONS OF HETARYL AND ARYL HALIDES WITH THIOPHENOXIDE ION IN -

The Copper Catalysed Reaction of Sodium Methoxide with Aryl Bromides : a Mechanistic Study Leading to a Facile Synthesis of Anisole Derivatives
The copper catalysed reaction of sodium methoxide with aryl bromides : a mechanistic study leading to a facile synthesis of anisole derivatives Citation for published version (APA): Aalten, H. L., Koten, van, G., Grove, D. M., Kuilman, T., Piekstra, O. G., Hulshof, L. A., & Sheldon, R. A. (1989). The copper catalysed reaction of sodium methoxide with aryl bromides : a mechanistic study leading to a facile synthesis of anisole derivatives. Tetrahedron, 45(17), 5565-5578. https://doi.org/10.1016/S0040-4020(01)89502- 8 DOI: 10.1016/S0040-4020(01)89502-8 Document status and date: Published: 01/01/1989 Document Version: Publisher’s PDF, also known as Version of Record (includes final page, issue and volume numbers) Please check the document version of this publication: • A submitted manuscript is the version of the article upon submission and before peer-review. There can be important differences between the submitted version and the official published version of record. People interested in the research are advised to contact the author for the final version of the publication, or visit the DOI to the publisher's website. • The final author version and the galley proof are versions of the publication after peer review. • The final published version features the final layout of the paper including the volume, issue and page numbers. Link to publication General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. -

Ep 0409164 A2
Europaisches Patentamt European Patent Office © Publication number: 0 409 1 64 A2 Office europeen des brevets © EUROPEAN PATENT APPLICATION © Application number: 90113679.6 © Int. CI* C07D 501/36, C07D 498/053, A61K 31/545, A61K 31/535 @ Date of filing: 17.07.90 © Priority: 18.07.89 JP 186330/89 © Applicant: SHIONOGI SEIYAKU KABUSHIKI KAISHA trading under the name of © Date of publication of application: SHIONOGI & CO. LTD.TD. 23.01.91 Bulletin 91/04 1-8, Doshomachi 3-chome Chuo-ku Osaka 541 (JP) © Designated Contracting States: CH DE FR GB IT LI NL © Inventor: Onoue, Hiroshi 3-7-4, Takatsukadai, Kawai-cho Kitakatsuragi-gun, Nara(JP) Inventor: Minami, Kyoji 720-42, Oze-cho Ikoma-shi, Nara(JP) Inventor: Ishikura, Koji 2-11-4, Mimatsu Nara-shi, Nara(JP) © Representative: Vossius & Partnerner Siebertstrasse 4 P.O. Box 86 07 67 D-8000 Munchen 86(DE) © Phenacylpyridiniothiocephalosporins. © An antibacterial- 3-optionally protected-vic-dihydroxyaroyl-Iower alkyl-pyridiniothiomethyl cephalosporin de- rivative represented by the following formula (I): {© (wherein, t™ R1 is an amino group or acylamino; R2 is hydrogen or methoxy; R3 is hydrogen or a mono- or divalent q) substituent; R4 is optionally protected vic-dihydroxyaryl; R5 is straight or branched lower alkylene; R6 is O hydrogen, a carboxy-protecting group or a negative charge when combined with Y; X is oxygen, sulfur, or "@jf sulfinyl; and Y is an anion or a negative charge when combined with R6; and the dotted line shows the presence © or absence of a bond), and method of bacterial infection it, and synthetic methods thereof are provided. -

Catalysed Pbotiodeiodination of Aryl Iodides. A
STUDIES OF BASE - CATALYSED PBOTIODEIODINATION OF ARYL IODIDES. A thesis presented for the degree of Doctor of Philosophy in the Faculty of Science of the University of London. by CLIVE MOORE November, 1981. Bedford College, London, ProQuest Number: 10098446 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest 10098446 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 2. ACKNOWLE DGEMENTS I would like to extend my unfeigned gratitude to my supervisors, Dr. R. Bolton and Dr. J.P.B, Sandall, for their initial suggestion of this research topic, and their incessant enthusiasm and forebearance throughout the period of this work. I am also indebted to the Science Research Council for the award of a grant for this research. Finally, I would like to thank Mrs.Irene Fraser for typing this thesis. 3. ABSTRACT. The rates of the methoxide ion induced protiodeiodination of a number of polychlorolodoarenes in dimethyl sulphoxide-methanol (9:1, v/v) have been measured at 323*2K. Chlorine substituents activate all positions in the order, o;-Cl > m-Cl > £;-Cl, although the more fully substituted polychloroiodoarenes show much weaker substituent effects. -

Mechanism and Stereochemistry of the Reaction Ofnitric Oxide with Secondary Amines
Mechanism and Stereochemistry of the Reaction ofNitric Oxide with Secondary Amines By Kamilah Smith A thesis submitted ta McGill University in partial fulfillment ofthe requirements for the degree of Doctor of Philosophy Department of Chemistry McGill University Montreal, Quebec Canada © Kamilah Smith, February 2007 Library and Bibliothèque et 1+1 Archives Canada Archives Canada Published Heritage Direction du Branch Patrimoine de l'édition 395 Wellington Street 395, rue Wellington Ottawa ON K1A ON4 Ottawa ON K1A ON4 Canada Canada Your file Votre référence ISBN: 978-0-494-32326-7 Our file Notre référence ISBN: 978-0-494-32326-7 NOTICE: AVIS: The author has granted a non L'auteur a accordé une licence non exclusive exclusive license allowing Library permettant à la Bibliothèque et Archives and Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par télécommunication ou par l'Internet, prêter, telecommunication or on the Internet, distribuer et vendre des thèses partout dans loan, distribute and sell th es es le monde, à des fins commerciales ou autres, worldwide, for commercial or non sur support microforme, papier, électronique commercial purposes, in microform, et/ou autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriété du droit d'auteur ownership and moral rights in et des droits moraux qui protège cette thèse. this thesis. Neither the thesis Ni la thèse ni des extraits substantiels de nor substantial extracts from it celle-ci ne doivent être imprimés ou autrement may be printed or otherwise reproduits sans son autorisation. -

UNITED STATES PATENT OFFICE 2,500,444 URAMIDOHOMOMEROQUINENE Robert Burns Woodward, Cambridge, Mass., and William Von Eggers Doering, New York, N
Patented Mar. 14, 1950 2,500,444 UNITED STATES PATENT OFFICE 2,500,444 URAMIDOHOMOMEROQUINENE Robert Burns Woodward, Cambridge, Mass., and William von Eggers Doering, New York, N. Y., assignors to Polaroid Corporation, Cambridge, Mass., a corporation of Delaware No Drawing. Application October 10, 1944, Serial No. 558,080 Claim. (C. 260-294) 2 This invention relates to the synthesis of Which stereoisomers may be isolated as chemical quinine and cinchona-like alkaloids. individuals and then subjected to further trans The present application is a continuation-in formation. It is preferable, however, instead of part of our copending applications Serial No. 508,- isolating the stereoisoners from their mixture, to 954, filed November 4, 1943, now Patent No. 2,475,- Oxidize the latter and thus form a mixture of the 932, entitled "7-hydroxyisoquinoline derivatives Corresponding ketones, i. e., the stereoisomers of and method of preparing the same,' and Serial 2-acetyl-7-keto - 8-methyldecahydroisoquino No. 523,940, filed February 25, 1944, now Patent line, and to isolate from the latter mixture the No. 2,395,526, entitled “Isoquinoline derivatives Stereochemically homogeneous products. The and methods of preparing the same.' 10 carbocyclic ring of each stereoisomeric ketone may It is one object of the present invention to pro then be cleaved to give the corresponding N vide a novel process of synthesizing homonero acetyl - 10 - oximinodihydrohomomeroquinene quinene from isoquinoline derivatives. ethyl ester having the formula Another object is to provide novel quinine and cinchona-like alkaloids, and particularly al H. kaloids having the structural formula of quinine 5 /\H NoH and quinotoxine, derived from 1-cis-homonero CH3CON 5C-C-CE quinene and racemic-cis-homomeroquinene and O from one of the trans-homomeroquinenes.