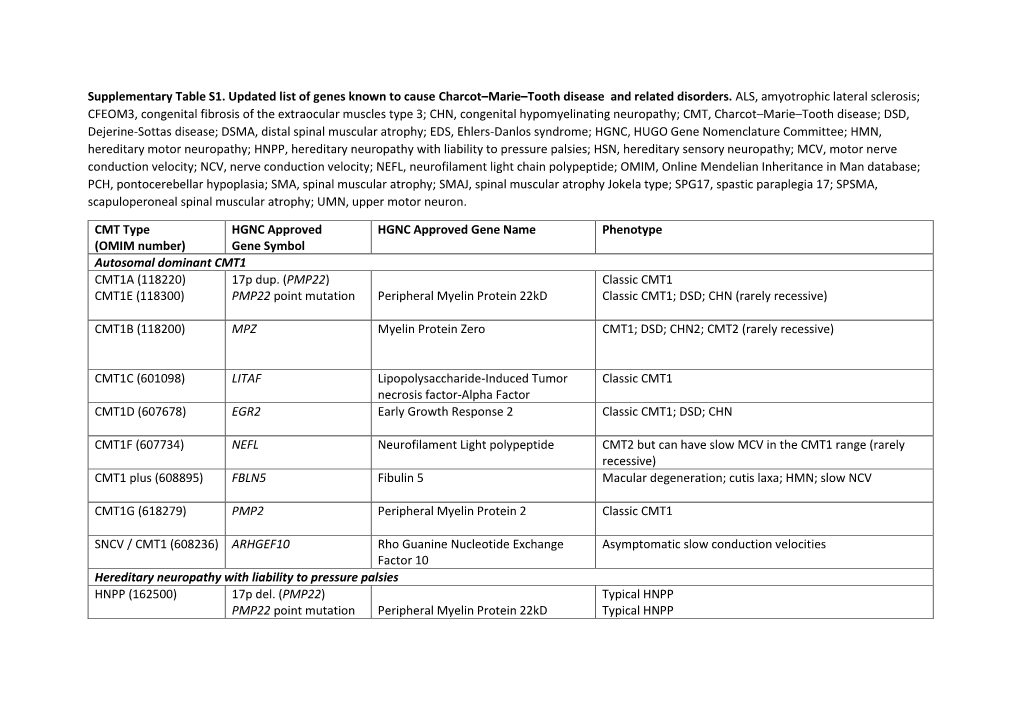
Pipis NRN CMT Review for UCL RPS Supplem.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lamin-Related Congenital Muscular Dystrophy Alters Mechanical Signaling and Skeletal Muscle Growth
International Journal of Molecular Sciences Article Lamin-Related Congenital Muscular Dystrophy Alters Mechanical Signaling and Skeletal Muscle Growth Daniel J. Owens 1,2 , Julien Messéant 1, Sophie Moog 3, Mark Viggars 2, Arnaud Ferry 1,4, Kamel Mamchaoui 1,5, Emmanuelle Lacène 5 , Norma Roméro 5,6, Astrid Brull 1 , Gisèle Bonne 1 , Gillian Butler-Browne 1 and Catherine Coirault 1,* 1 Center for Research in Myology, Sorbonne Université, INSERM UMRS_974, 75013 Paris, France; [email protected] (D.J.O.); [email protected] (J.M.); [email protected] (A.F.); [email protected] (K.M.); [email protected] (A.B.); [email protected] (G.B.); [email protected] (G.B.-B.) 2 Research Institute for Sport and Exercise Science, Liverpool John Moores University, Liverpool L3 3AF, UK; [email protected] 3 Inovarion, 75005 Paris, France; [email protected] 4 Université de Paris, 75006 Paris, France 5 Neuromuscular Morphology Unit, Institute of Myology, Pitié-Salpêtrière Hospital, 75013 Paris, France; [email protected] (E.L.); [email protected] (N.R.) 6 APHP, Reference Center for Neuromuscular Disorders, Pitié-Salpêtrière Hospital, Institute of Myology, 75013 Paris, France * Correspondence: [email protected]; Tel.: +33-1-1-4216-5708 Abstract: Laminopathies are a clinically heterogeneous group of disorders caused by mutations in the LMNA gene, which encodes the nuclear envelope proteins lamins A and C. The most frequent diseases associated with LMNA mutations are characterized by skeletal and cardiac involvement, and include autosomal dominant Emery–Dreifuss muscular dystrophy (EDMD), limb-girdle muscular Citation: Owens, D.J.; Messéant, J.; dystrophy type 1B, and LMNA-related congenital muscular dystrophy (LMNA-CMD). -

ARVC-Variants.Pdf
Updated gene list responsible for ARVC/D pathology Subtype Gene Location Reference ARVC1 TGFB3 14q24.3 Beffagna G, Occhi G, Nava A, et al. Regulatory mutations in transforming growth factor-beta3 gene cause arrhythmogenic right ventricular cardiomyopathy type 1. Cardiovasc Res. 2005;65:366–73. ARVC2 RYR2 1q43 Tiso N, Stephan DA, Nava A, et al. Identification of mutations in the cardiac ryanodine receptor gene in families affected with arrhythmogenic right ventricular cardiomyopathy type 2 (ARVD2). Hum Mol Genet. 2001;10:189–94. ARVC3 Unknown 14q12-q22 Severini GM, Krajinovic M, Pinamonti B, et al. A new locus for arrhythmogenic right ventricular dysplasia on the long arm of chromosome 14. Genomics. 1996;31:193–200. ARVC4 TTN 2q32.1-q32.3 Taylor M, Graw S, Sinagra G, et al. Genetic variation in titin in arrhythmogenic right ventricular cardiomyopathy-overlap syndromes. Circulation. 2011;124:876–85. ARVC5 TMEM43 3p25.1 Merner ND, Hodgkinson KA, Haywood AF, et al. Arrhythmogenic right ventricular cardiomyopathy type 5 is a fully penetrant, lethal arrhythmic disorder caused by a missense mutation in the TMEM43 gene. Am J Hum Genet. 2008;82:809–21. ARVC6 Unknown 10p14-p12 Li D, Ahmad F, Gardner MJ, et al. The locus of a novel gene responsible for arrhythmogenic right- ventricular dysplasia characterized by early onset and high penetrance maps to chromosome 10p12-p14. Am J Hum Genet. 2000;66:148–56. ARVC7 DES 2q35 Klauke B, Kossmann S, Gaertner A, et al. De novo desmin-mutation N116S is associated with arrhythmogenic right ventricular cardiomyopathy. Hum Mol Genet. 2010;19:4595–607. -

Entrez Symbols Name Termid Termdesc 117553 Uba3,Ube1c
Entrez Symbols Name TermID TermDesc 117553 Uba3,Ube1c ubiquitin-like modifier activating enzyme 3 GO:0016881 acid-amino acid ligase activity 299002 G2e3,RGD1310263 G2/M-phase specific E3 ubiquitin ligase GO:0016881 acid-amino acid ligase activity 303614 RGD1310067,Smurf2 SMAD specific E3 ubiquitin protein ligase 2 GO:0016881 acid-amino acid ligase activity 308669 Herc2 hect domain and RLD 2 GO:0016881 acid-amino acid ligase activity 309331 Uhrf2 ubiquitin-like with PHD and ring finger domains 2 GO:0016881 acid-amino acid ligase activity 316395 Hecw2 HECT, C2 and WW domain containing E3 ubiquitin protein ligase 2 GO:0016881 acid-amino acid ligase activity 361866 Hace1 HECT domain and ankyrin repeat containing, E3 ubiquitin protein ligase 1 GO:0016881 acid-amino acid ligase activity 117029 Ccr5,Ckr5,Cmkbr5 chemokine (C-C motif) receptor 5 GO:0003779 actin binding 117538 Waspip,Wip,Wipf1 WAS/WASL interacting protein family, member 1 GO:0003779 actin binding 117557 TM30nm,Tpm3,Tpm5 tropomyosin 3, gamma GO:0003779 actin binding 24779 MGC93554,Slc4a1 solute carrier family 4 (anion exchanger), member 1 GO:0003779 actin binding 24851 Alpha-tm,Tma2,Tmsa,Tpm1 tropomyosin 1, alpha GO:0003779 actin binding 25132 Myo5b,Myr6 myosin Vb GO:0003779 actin binding 25152 Map1a,Mtap1a microtubule-associated protein 1A GO:0003779 actin binding 25230 Add3 adducin 3 (gamma) GO:0003779 actin binding 25386 AQP-2,Aqp2,MGC156502,aquaporin-2aquaporin 2 (collecting duct) GO:0003779 actin binding 25484 MYR5,Myo1e,Myr3 myosin IE GO:0003779 actin binding 25576 14-3-3e1,MGC93547,Ywhah -

Genetic Mutations and Mechanisms in Dilated Cardiomyopathy
Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, … , Jessica R. Golbus, Megan J. Puckelwartz J Clin Invest. 2013;123(1):19-26. https://doi.org/10.1172/JCI62862. Review Series Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of congestive heart failure. In hypertrophic cardiomyopathy (HCM), cardiac output is limited by the thickened myocardium through impaired filling and outflow. Mutations in the genes encoding the thick filament components myosin heavy chain and myosin binding protein C (MYH7 and MYBPC3) together explain 75% of inherited HCMs, leading to the observation that HCM is a disease of the sarcomere. Many mutations are “private” or rare variants, often unique to families. In contrast, dilated cardiomyopathy (DCM) is far more genetically heterogeneous, with mutations in genes encoding cytoskeletal, nucleoskeletal, mitochondrial, and calcium-handling proteins. DCM is characterized by enlarged ventricular dimensions and impaired systolic and diastolic function. Private mutations account for most DCMs, with few hotspots or recurring mutations. More than 50 single genes are linked to inherited DCM, including many genes that also link to HCM. Relatively few clinical clues guide the diagnosis of inherited DCM, but emerging evidence supports the use of genetic testing to identify those patients at risk for faster disease progression, congestive heart failure, and arrhythmia. Find the latest version: https://jci.me/62862/pdf Review series Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, Jessica R. Golbus, and Megan J. Puckelwartz Department of Human Genetics, University of Chicago, Chicago, Illinois, USA. Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of conges- tive heart failure. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
![Downloaded from [266]](https://docslib.b-cdn.net/cover/7352/downloaded-from-266-347352.webp)
Downloaded from [266]
Patterns of DNA methylation on the human X chromosome and use in analyzing X-chromosome inactivation by Allison Marie Cotton B.Sc., The University of Guelph, 2005 A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY in The Faculty of Graduate Studies (Medical Genetics) THE UNIVERSITY OF BRITISH COLUMBIA (Vancouver) January 2012 © Allison Marie Cotton, 2012 Abstract The process of X-chromosome inactivation achieves dosage compensation between mammalian males and females. In females one X chromosome is transcriptionally silenced through a variety of epigenetic modifications including DNA methylation. Most X-linked genes are subject to X-chromosome inactivation and only expressed from the active X chromosome. On the inactive X chromosome, the CpG island promoters of genes subject to X-chromosome inactivation are methylated in their promoter regions, while genes which escape from X- chromosome inactivation have unmethylated CpG island promoters on both the active and inactive X chromosomes. The first objective of this thesis was to determine if the DNA methylation of CpG island promoters could be used to accurately predict X chromosome inactivation status. The second objective was to use DNA methylation to predict X-chromosome inactivation status in a variety of tissues. A comparison of blood, muscle, kidney and neural tissues revealed tissue-specific X-chromosome inactivation, in which 12% of genes escaped from X-chromosome inactivation in some, but not all, tissues. X-linked DNA methylation analysis of placental tissues predicted four times higher escape from X-chromosome inactivation than in any other tissue. Despite the hypomethylation of repetitive elements on both the X chromosome and the autosomes, no changes were detected in the frequency or intensity of placental Cot-1 holes. -

Nuclear Titin Interacts with A- and B-Type Lamins in Vitro and in Vivo
Research Article 239 Nuclear Titin interacts with A- and B-type lamins in vitro and in vivo Michael S. Zastrow1,*, Denise B. Flaherty2‡, Guy M. Benian2 and Katherine L. Wilson1,§ 1Department of Cell Biology, The Johns Hopkins University School of Medicine, 725 N. Wolfe St, Baltimore, MD 21205, USA 2Department of Pathology, Emory University, Whitehead Biomedical Research Building, Atlanta, GA 30332, USA *Present address: Department of Developmental Biology, Stanford University School of Medicine, Beckman Center, B300, 279 Campus Drive, Stanford, CA 94305, USA ‡Department of Biology, Eckerd College, SHB 105, 4200 54th Ave, St Petersburg, FL 33711, USA §Author for correspondence (e-mail: [email protected]) Accepted 4 October 2005 Journal of Cell Science 119, 239-249 Published by The Company of Biologists 2006 doi:10.1242/jcs.02728 Summary Lamins form structural filaments in the nucleus. Mutations lamin-downregulated [lmn-1(RNAi)] embryos, Ce-titin was in A-type lamins cause muscular dystrophy, undetectable at the nuclear envelope suggesting its cardiomyopathy and other diseases, including progeroid localization or stability requires Ce-lamin. In human cells syndromes. To identify new binding partners for lamin A, (HeLa), antibodies against the titin-specific domain M-is6 we carried out a two-hybrid screen with a human skeletal- gave both diffuse and punctate intranuclear staining by muscle cDNA library, using the Ig-fold domain of lamin A indirect immunofluorescence, and recognized at least three as bait. The C-terminal region of titin was recovered twice. bands larger than 1 MDa in immunoblots of isolated HeLa Previous investigators showed that nuclear isoforms of titin nuclei. -

(Ser739) Antibody-SL10016R
SunLong Biotech Co.,LTD Tel: 0086-571- 56623320 Fax:0086-571- 56623318 E-mail:[email protected] www.sunlongbiotech.com Rabbit Anti-phospho-ZCWCC1 (Ser739) antibody SL10016R Product Name: phospho-ZCWCC1 (Ser739) Chinese Name: 磷酸化ZCWCC1抗体 AC004542.C22.1.; p-MORC2(Ser739); phospho-ZCWCC1(Ser739); CW type with coiled coil domain 1; KIAA0852; ZCW3; ZCWCC1; Zinc finger; Zinc finger CW type Alias: coiled coil domain protein 1; Zinc finger CW type with coiled coil domain 1; Zing finger CW type 3 zinc finger CW-type coiled-coil domain protein 1; MORC family CW-type zine finger 2; MORC2. Organism Species: Rabbit Clonality: Polyclonal React Species: Human,Mouse,Rat, WB=1:500-2000ELISA=1:500-1000IHC-P=1:400-800IHC-F=1:400-800ICC=1:100- 500IF=1:100-500(Paraffin sections need antigen repair) Applications: not yet tested in other applications. optimal dilutions/concentrations should be determined by the end user. Molecular weight: 114kDa Cellular localization: The nucleuscytoplasmic Form: Lyophilizedwww.sunlongbiotech.com or Liquid Concentration: 1mg/ml KLH conjugated synthesised phosphopeptide derived from human MORC2 around the immunogen: phosphorylation site of Ser739:KR(p-S)VA Lsotype: IgG Purification: affinity purified by Protein A Storage Buffer: 0.01M TBS(pH7.4) with 1% BSA, 0.03% Proclin300 and 50% Glycerol. Store at -20 °C for one year. Avoid repeated freeze/thaw cycles. The lyophilized antibody is stable at room temperature for at least one month and for greater than a year Storage: when kept at -20°C. When reconstituted in sterile pH 7.4 0.01M PBS or diluent of antibody the antibody is stable for at least two weeks at 2-4 °C. -

Lamin A/C Cardiomyopathy: Implications for Treatment
Current Cardiology Reports (2019) 21:160 https://doi.org/10.1007/s11886-019-1224-7 MYOCARDIAL DISEASE (A ABBATE AND G SINAGRA, SECTION EDITORS) Lamin A/C Cardiomyopathy: Implications for Treatment Suet Nee Chen1 & Orfeo Sbaizero1,2 & Matthew R. G. Taylor1 & Luisa Mestroni1 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review The purpose of this review is to provide an update on lamin A/C (LMNA)-related cardiomyopathy and discuss the current recommendations and progress in the management of this disease. LMNA-related cardiomyopathy, an inherited autosomal dominant disease, is one of the most common causes of dilated cardiomyopathy and is characterized by steady progression toward heart failure and high risks of arrhythmias and sudden cardiac death. Recent Findings We discuss recent advances in the understanding of the molecular mechanisms of the disease including altered cell biomechanics, which may represent novel therapeutic targets to advance the current management approach, which relies on standard heart failure recommendations. Future therapeutic approaches include repurposed molecularly directed drugs, siRNA- based gene silencing, and genome editing. Summary LMNA-related cardiomyopathy is the focus of active in vitro and in vivo research, which is expected to generate novel biomarkers and identify new therapeutic targets. LMNA-related cardiomyopathy trials are currently underway. Keywords Lamin A/C gene . Laminopathy . Heart failure . Arrhythmias . Mechanotransduction . P53 . CRISPR–Cas9 therapy Introduction functions, including maintaining nuclear structural integrity, regulating gene expression, mechanosensing, and Mutations in the lamin A/C gene (LMNA)causelaminopathies, mechanotransduction through the lamina-associated proteins a heterogeneous group of inherited disorders including muscu- [6–11]. -
Proteomic and Bioinformatic Investigation of Altered Pathways in Neuroglobin-Deficient Breast Cancer Cells
molecules Article Proteomic and Bioinformatic Investigation of Altered Pathways in Neuroglobin-Deficient Breast Cancer Cells Michele Costanzo 1,2 , Marco Fiocchetti 3 , Paolo Ascenzi 3, Maria Marino 3 , Marianna Caterino 1,2,* and Margherita Ruoppolo 1,2,* 1 Department of Molecular Medicine and Medical Biotechnology, School of Medicine, University of Naples Federico II, 80131 Naples, Italy; [email protected] 2 CEINGE—Biotecnologie Avanzate S.C.Ar.L., 80145 Naples, Italy 3 Department of Science, University Roma Tre, 00146 Rome, Italy; marco.fi[email protected] (M.F.); [email protected] (P.A.); [email protected] (M.M.) * Correspondence: [email protected] (M.C.); [email protected] (M.R.) Abstract: Neuroglobin (NGB) is a myoglobin-like monomeric globin that is involved in several processes, displaying a pivotal redox-dependent protective role in neuronal and extra-neuronal cells. NGB remarkably exerts its function upon upregulation by NGB inducers, such as 17β-estradiol (E2) and H2O2. However, the molecular bases of NGB’s functions remain undefined, mainly in non- neuronal cancer cells. Human MCF-7 breast cancer cells with a knocked-out (KO) NGB gene obtained using CRISPR/Cas9 technology were analyzed using shotgun label-free quantitative proteomics in comparison with control cells. The differential proteomics experiments were also performed after treatment with E2, H2O2, and E2 + H2O2. All the runs acquired using liquid chromatography–tandem mass spectrometry were elaborated within the same MaxQuant analysis, leading to the quantification Citation: Costanzo, M.; Fiocchetti, of 1872 proteins in the global proteomic dataset. Then, a differentially regulated protein dataset was M.; Ascenzi, P.; Marino, M.; Caterino, M.; Ruoppolo, M. -

Supplementary Table S1. Correlation Between the Mutant P53-Interacting Partners and PTTG3P, PTTG1 and PTTG2, Based on Data from Starbase V3.0 Database
Supplementary Table S1. Correlation between the mutant p53-interacting partners and PTTG3P, PTTG1 and PTTG2, based on data from StarBase v3.0 database. PTTG3P PTTG1 PTTG2 Gene ID Coefficient-R p-value Coefficient-R p-value Coefficient-R p-value NF-YA ENSG00000001167 −0.077 8.59e-2 −0.210 2.09e-6 −0.122 6.23e-3 NF-YB ENSG00000120837 0.176 7.12e-5 0.227 2.82e-7 0.094 3.59e-2 NF-YC ENSG00000066136 0.124 5.45e-3 0.124 5.40e-3 0.051 2.51e-1 Sp1 ENSG00000185591 −0.014 7.50e-1 −0.201 5.82e-6 −0.072 1.07e-1 Ets-1 ENSG00000134954 −0.096 3.14e-2 −0.257 4.83e-9 0.034 4.46e-1 VDR ENSG00000111424 −0.091 4.10e-2 −0.216 1.03e-6 0.014 7.48e-1 SREBP-2 ENSG00000198911 −0.064 1.53e-1 −0.147 9.27e-4 −0.073 1.01e-1 TopBP1 ENSG00000163781 0.067 1.36e-1 0.051 2.57e-1 −0.020 6.57e-1 Pin1 ENSG00000127445 0.250 1.40e-8 0.571 9.56e-45 0.187 2.52e-5 MRE11 ENSG00000020922 0.063 1.56e-1 −0.007 8.81e-1 −0.024 5.93e-1 PML ENSG00000140464 0.072 1.05e-1 0.217 9.36e-7 0.166 1.85e-4 p63 ENSG00000073282 −0.120 7.04e-3 −0.283 1.08e-10 −0.198 7.71e-6 p73 ENSG00000078900 0.104 2.03e-2 0.258 4.67e-9 0.097 3.02e-2 Supplementary Table S2. -

Genome-Wide DNA Methylation Analysis on C-Reactive Protein Among Ghanaians Suggests Molecular Links to the Emerging Risk of Cardiovascular Diseases ✉ Felix P
www.nature.com/npjgenmed ARTICLE OPEN Genome-wide DNA methylation analysis on C-reactive protein among Ghanaians suggests molecular links to the emerging risk of cardiovascular diseases ✉ Felix P. Chilunga 1 , Peter Henneman2, Andrea Venema2, Karlijn A. C. Meeks 3, Ana Requena-Méndez4,5, Erik Beune1, Frank P. Mockenhaupt6, Liam Smeeth7, Silver Bahendeka8, Ina Danquah9, Kerstin Klipstein-Grobusch10,11, Adebowale Adeyemo 3, Marcel M.A.M Mannens2 and Charles Agyemang1 Molecular mechanisms at the intersection of inflammation and cardiovascular diseases (CVD) among Africans are still unknown. We performed an epigenome-wide association study to identify loci associated with serum C-reactive protein (marker of inflammation) among Ghanaians and further assessed whether differentially methylated positions (DMPs) were linked to CVD in previous reports, or to estimated CVD risk in the same population. We used the Illumina Infinium® HumanMethylation450 BeadChip to obtain DNAm profiles of blood samples in 589 Ghanaians from the RODAM study (without acute infections, not taking anti-inflammatory medications, CRP levels < 40 mg/L). We then used linear models to identify DMPs associated with CRP concentrations. Post-hoc, we evaluated associations of identified DMPs with elevated CVD risk estimated via ASCVD risk score. We also performed subset analyses at CRP levels ≤10 mg/L and replication analyses on candidate probes. Finally, we assessed for biological relevance of our findings in public databases. We subsequently identified 14 novel DMPs associated with CRP. In post-hoc evaluations, we found 1234567890():,; that DMPs in PC, BTG4 and PADI1 showed trends of associations with estimated CVD risk, we identified a separate DMP in MORC2 that was associated with CRP levels ≤10 mg/L, and we successfully replicated 65 (24%) of previously reported DMPs.