Cutaneous Myiasis (Wohlfahrtia Magnifica)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical and Veterinary Entomology (2009) 23 (Suppl
Medical and Veterinary Entomology (2009) 23 (Suppl. 1), 1–7 Enabling technologies to improve area-wide integrated pest management programmes for the control of screwworms A. S. ROBINSON , M. J. B. VREYSEN , J. HENDRICHS and U. FELDMANN Joint Food and Agriculture Organization of the United Nations/International Atomic Energy Agency (FAO/IAEA) Programme of Nuclear Techniques in Food and Agriculture, Vienna, Austria Abstract . The economic devastation caused in the past by the New World screwworm fly Cochliomyia hominivorax (Coquerel) (Diptera: Calliphoridae) to the livestock indus- try in the U.S.A., Mexico and the rest of Central America was staggering. The eradication of this major livestock pest from North and Central America using the sterile insect tech- nique (SIT) as part of an area-wide integrated pest management (AW-IPM) programme was a phenomenal technical and managerial accomplishment with enormous economic implications. The area is maintained screwworm-free by the weekly release of 40 million sterile flies in the Darien Gap in Panama, which prevents migration from screwworm- infested areas in Columbia. However, the species is still a major pest in many areas of the Caribbean and South America and there is considerable interest in extending the eradica- tion programme to these countries. Understanding New World screwworm fly popula- tions in the Caribbean and South America, which represent a continuous threat to the screwworm-free areas of Central America and the U.S.A., is a prerequisite to any future eradication campaigns. The Old World screwworm fly Chrysomya bezziana Villeneuve (Diptera: Calliphoridae) has a very wide distribution ranging from Southern Africa to Papua New Guinea and, although its economic importance is assumed to be less than that of its New World counterpart, it is a serious pest in extensive livestock production and a constant threat to pest-free areas such as Australia. -

Evolutionary Background Entities at the Cellular and Subcellular Levels in Bodies of Invertebrate Animals
The Journal of Theoretical Fimpology Volume 2, Issue 4: e-20081017-2-4-14 December 28, 2014 www.fimpology.com Evolutionary Background Entities at the Cellular and Subcellular Levels in Bodies of Invertebrate Animals Shu-dong Yin Cory H. E. R. & C. Inc. Burnaby, British Columbia, Canada Email: [email protected] ________________________________________________________________________ Abstract The novel recognition that individual bodies of normal animals are actually inhabited by subcellular viral entities and membrane-enclosed microentities, prokaryotic bacterial and archaeal cells and unicellular eukaryotes such as fungi and protists has been supported by increasing evidences since the emergence of culture-independent approaches. However, how to understand the relationship between animal hosts including human beings and those non-host microentities or microorganisms is challenging our traditional understanding of pathogenic relationship in human medicine and veterinary medicine. In recent novel evolution theories, the relationship between animals and their environments has been deciphered to be the interaction between animals and their environmental evolutionary entities at the same and/or different evolutionary levels;[1-3] and evolutionary entities of the lower evolutionary levels are hypothesized to be the evolutionary background entities of entities at the higher evolutionary levels.[1,2] Therefore, to understand the normal existence of microentities or microorganisms in multicellular animal bodies is becoming the first priority for elucidating the ecological and evolutiological relationships between microorganisms and nonhuman macroorganisms. The evolutionary background entities at the cellular and subcellular levels in bodies of nonhuman vertebrate animals have been summarized recently.[4] In this paper, the author tries to briefly review the evolutionary background entities (EBE) at the cellular and subcellular levels for several selected invertebrate animal species. -

Microbial Communities Associated with Stable Fly (Diptera: Muscidae) Larvae and Their Developmental Substrates Erin Scully USDA-ARS, [email protected]
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Faculty Publications: Department of Entomology Entomology, Department of 2017 Microbial Communities Associated With Stable Fly (Diptera: Muscidae) Larvae and Their Developmental Substrates Erin Scully USDA-ARS, [email protected] Kristina Friesen USDA-ARS, [email protected] Brian Wienhold USDA-ARS, [email protected] Lisa M. Durso USDA-ARS, [email protected] Follow this and additional works at: http://digitalcommons.unl.edu/entomologyfacpub Part of the Entomology Commons Scully, Erin; Friesen, Kristina; Wienhold, Brian; and Durso, Lisa M., "Microbial Communities Associated With Stable Fly (Diptera: Muscidae) Larvae and Their eD velopmental Substrates" (2017). Faculty Publications: Department of Entomology. 502. http://digitalcommons.unl.edu/entomologyfacpub/502 This Article is brought to you for free and open access by the Entomology, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Faculty Publications: Department of Entomology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Annals of the Entomological Society of America, 110(1), 2017, 61–72 doi: 10.1093/aesa/saw087 Special Collection: Filth Fly–Microbe Interactions Research article Microbial Communities Associated With Stable Fly (Diptera: Muscidae) Larvae and Their Developmental Substrates Erin Scully,1 Kristina Friesen,2,3 Brian Wienhold,2 and Lisa M. Durso2 1USDA, ARS, Stored Product -

A Case in a Puppy and Overview of Geographical Distribution
ACTA VET. BRNO 2020, 89: 171–177; https://doi.org/10.2754/avb202089020171 Wohlfahrtiosis in Italy: a case in a puppy and overview of geographical distribution Teresa Bonacci1, Giuseppe Curia2, Chiara Scapoli3, Marco Pezzi3 1University of Calabria, Department of Biology, Ecology and Earth Science, Cosenza, Italy 2Azienda Sanitaria Provinciale di Cosenza, Servizio Veterinario, Cosenza, Italy 3University of Ferrara, Department of Life Sciences and Biotechnology, Ferrara, Italy Received November 26, 2019 Accepted April 30, 2020 Abstract The report describes a case of urogenital myiasis in a puppy, Canis lupus familiaris (Carnivora: Canidae) caused by Wohlfahrtia magnifica (Diptera: Sarcophagidae) in Calabria, southern Italy. This species is an obligatory agent of myiasis in human and other warm-blooded vertebrates. The puppy was healthy and was not living near farm animals, usual hosts of this flesh fly. An overview of cases of human and animal myiasis caused by W. magnifica in Italy and of data and specimens documented in entomology museum collections is also reported. Canine, urogenital myiasis, Wohlfahrtia magnifica Myiasis is an important parasitic disease caused by larvae of Diptera infesting vertebrates actively feeding on host tissues (Zumpt 1965). The term “wohlfahrtiosis” refers to myiasis caused by Wohlfahrtia magnifica (Schiner, 1862) (Insecta: Diptera: Sarcophagidae). Among the types of myiasis, wohlfahrtiosis is especially important not only because it may affect humans, but also because it usually induces serious damage due to the high number of deposited larvae and to their rapid growth. When attacking livestock, the parasite may cause heavy economic damages through loss of production and death (Hall and Farkas 2000). In Europe wohlfahrtiosis is an infestation reported in humans and domestic animals in several countries, especially in southern and eastern areas. -

Human Urinary Myiasis Due to Larvae of Clogmia (Telmatoscopus) Albipunctata Williston (Diptera: Psychodidae) First Report in Egypt
J Vector Borne Dis 51, September 2014, pp. 247–249 Human urinary myiasis due to larvae of Clogmia (Telmatoscopus) albipunctata Williston (Diptera: Psychodidae) first report in Egypt Ayman A. El-Badry1, Hosni Khairy Salem2, Yusuf Abd El-Aziz Edmardash3 1Medical Parasitology Department; 2Urology Department, Kasr Al-Ainy Faculty of Medicine; 3Entomology Department, Faculty of Science, Cairo University, Cairo, Egypt Key words Clogmia albipunctata; Egypt; human myasis Human myiasis is defined as “the infestation of the Case report tissue of living human with dipterous larvae”1. Parasito- The patient presented with repeated passage of nu- logically myiasis could be classified as obligatory, facul- merous living dark-colored larvae in urine, 7–12 larvae tative or accidental. Clinically myiasis may be classified were voided intermittently over two months. She was according to part of the body tissue invaded. Cutaneous complaining of dysuria, fever and itching in the periure- myiasis is the commonest type. Body cavity myiasis; na- thral and genital regions. No history of travelling outside sopharyngeal, ocular, aural and the gastrointestinal tract Egypt in the past or the present time. Complete urine urogenital system are less common. Urethral myiasis is analysis and stool examination using direct and concen- exceptionally rare, even in sites usually protected by trated smear was done. Plain X-ray and pelviabdominal clothes, inaccessible for the flies1–2. A large number of ultrasound were also done. fly species may cause urinary myiasis. Larvae of Fannia Larvae from two different fresh urine samples were scalaris3 is the most frequent cause of urinary myiasis. identified morphologically as larvae of Clogmia Other fly genera Musca, Sarcophaga, Lucilia, Wohlfahr- albipunctata (Diptera: Psychodidae). -

XIII) Arribas, Manuela Guerrero, José Mª Prieto, Mª Pilar Rodríguez E Isabel Morón) Y Del Servicio De J
13. Nuevas_2009 7/1/10 12:15 Página 249 Graellsia, 65(2): 249-280 (2009) NOTICIA DE NUEVOS TÁXONES PARA LA CIENCIA EN EL ÁMBITO ÍBERO-BALEAR Y MACARONÉSICO Nuevos táxones animales descritos en la península Museo Nacional de Ciencias Naturales (Purificación Ibérica y Macaronesia desde 1994 (XIII) Arribas, Manuela Guerrero, José Mª Prieto, Mª Pilar Rodríguez e Isabel Morón) y del Servicio de J. FERNÁNDEZ Museo Nacional de Ciencias Naturales, C.S.I.C. Reprografía (Ana Aguilar), así como de Rafael Araujo José Gutiérrez Abascal, 2. 28006. Madrid. (bibliotecario de la Sociedad Española de E-mail: [email protected] Malacología). Como en otras ocasiones, el Proyecto Fauna Ibérica IX (CGL2007-66786-CO8-01) subvenciona la Otra vez al final del año presentamos una nueva edición de estas notas y el apoyo de las editoras y del relación de novedades taxonómicas en el ámbito ibé- Comité de Redacción de Graellsia las hace posible. rico y macaronésico. Las características de esta nueva entrega son las habituales: se incluyen todos aquéllos táxones de nueva descripción que incluyan represen- tantes en el área considerada; en el caso de las espe- cies sólo se consideran aquéllas cuya localidad tipo se *Kryptrochozoa Dunn, Edgecombe, Giribet, Hejnol, Martindale y Rouse, 2009 encuentra en el área considerada y las que entre su REFERENCIA: Giribet, G., Dunn, C.W., Edgecombe, G.D., Hejnol, A., distribución conocida en el momento de la descrip- Rouse, G.W. y Martindale, M.Q., 2009. Assembling the spiralian ción haya alguna parte de la zona considerada. El tree of life. En: Animal evolution: genomes, fossils, and trees. -

Cutaneous Myiasis in a Child Scalp Caused by Wohlfahrtia Magnifica (Diptera: Sarcophagidae): a Case Report
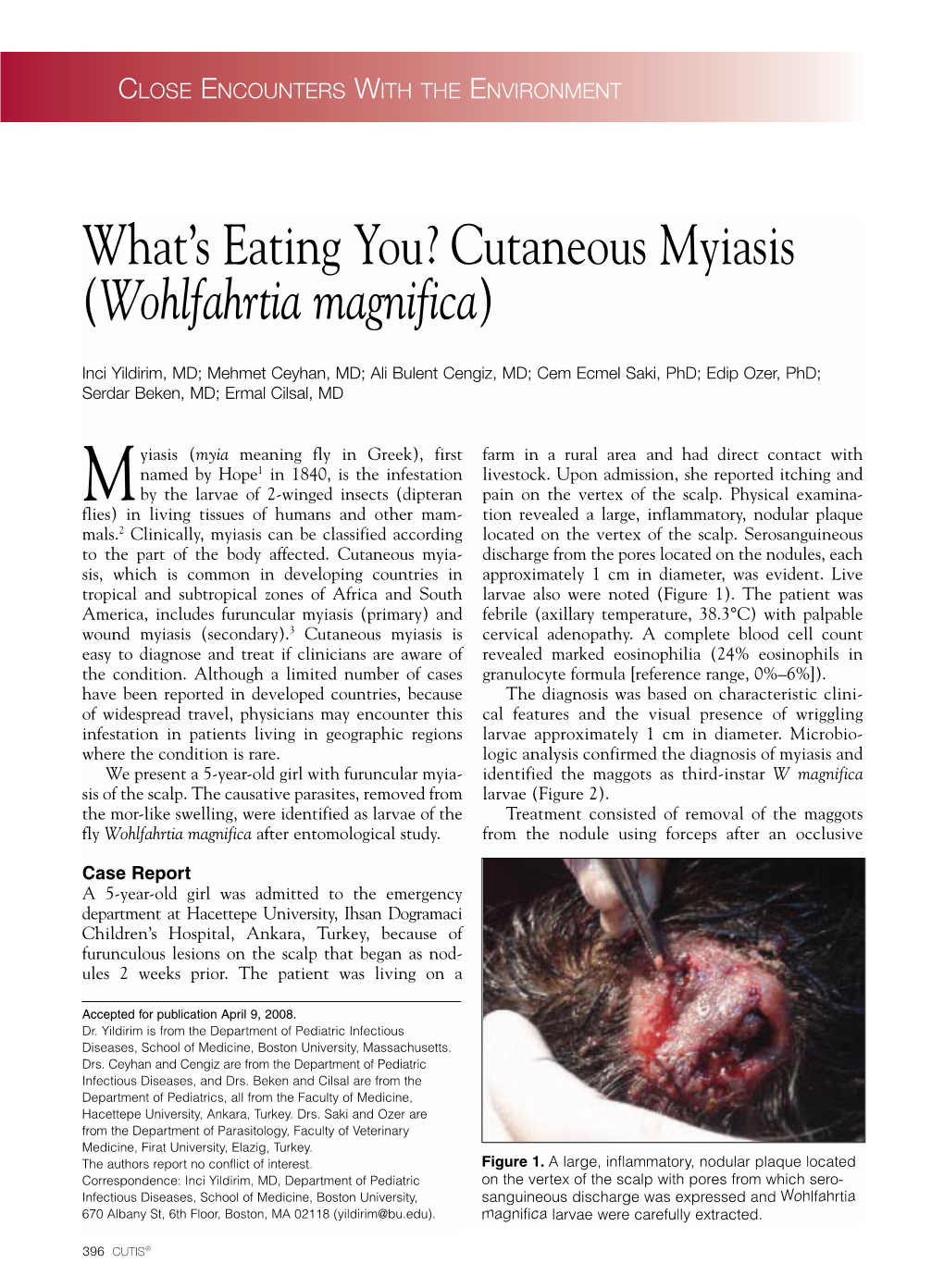
MOJ Clinical & Medical Case Reports Case Report Open Access Cutaneous myiasis in a child scalp caused by Wohlfahrtia Magnifica (Diptera: sarcophagidae): a case report Abstract Volume 4 Issue 3 - 2016 Background: Myiasis is caused by the invasion of tissues or organs of man or animals Raghad Al Badri,1 Taiba Al Harbi,1 Assad by dipterous larvae. A four-year-old girl presented with one month history of scalp 1 2 3,4 ulcer that has initially started as a painful itchy swelling in the occipital region. Tonnsi, Amal Almatary, Raafat Hassanein 1Pediatric Department, Maternity and Children Hospital, Saudi Physical examination revealed live maggots in the ulcerous wound. The maggots were Arabia identified as the third instar larvae of Wohlfahrtia magnifica. 2Department of Parasitology, Assiut University, Egypt 3 Case presentation: The patient presented to the emergency department with larva Department of Laboratory Medicine, Umm Al-Qura University, visualized inside the ulcer by the parents, the clinical examination has revealed a well Saudi Arabia 4Department of Animal Hygiene and Zoonoses, Assiut circumscribed circular lesion in the occipital region of the scalp with a diameter of University, Egypt approximately 4cm, it showed some signs of inflammation with necrotic tissue and many larva’s were seen inside the ulcer. The first surgical debridement was done in Correspondence: Raafat Hassanein, Department of the second day of admission to the hospital, during this operation a large number of Laboratory Medicine, Faculty of Applied Medical Sciences, Umm larvae were extracted and larval specimens were identified morphologically as larvae Al-Qura University, Makkah, Saudi Arabia, Tel +966-531664354, of Wohlfahrtia magnifica (Diptera: Sarcophagidae). -

(Insecta, Diptera, Sarcophagidae). - 1997
4)L ©Zoologische Staatssammlung München;download: http://www.biodiversitylibrary.org/; www.biologiezentrum.at \ 57Cls ^üniilTifiiiiiiii] miffit^iilllllliiiiülr SPIXIANA. |H, Zeitschrift für Zoologie ,ni|^S SPIXIANA • Supplement 24 • München, 15. Oktober 1997 • ISSN 0177-7424 • ISBN 3-931516-24-5 ©Zoologische Staatssammlung München;download: http://www.biodiversitylibrary.org/; www.biologiezentrum.at ©Zoologische Staatssammlung München;download: http://www.biodiversitylibrary.org/; www.biologiezentrum.at The Flesh-Flies of Central Europe (Insecta, Diptera, Sarcophagidae) Dalibor Povolny & Yuriy Verves ©Zoologische Staatssammlung München;download:SPIXIAMA http://www.biodiversitylibrary.org/; www.biologiezentrum.at ZEITSCHRIFT FÜR ZOOLOGIE herausgegeben von der ZOOLOGISCHEN STAATSSAMMLUNG MÜNCHEN SPIXIANA bringt Originalarbeiten aus dem Gesamtgebiet der Zoologischen Systematik mit Schwerpunkten in Morphologie, Phylogenie, Tiergeographie und Ökologie. Manuskripte werden in Deutsch, Englisch oder Französisch angenommen. Pro Jahr erscheint ein Band zu drei Heften. Umfangreiche Beiträge können in Supplementbänden herausgegeben werden. SPIXIANA publishes original papers on Zoological Systematics, with emphasis on Morphology, Phylogeny, Zoogeography and Ecology. Manuscripts will be accepted in German, English or French. A volume of three issues will be published annually. Extensive contributions may be edited in Supplement volumes. Redaktion - Editor-in-chief M. BAEHR Fotoarbeiten: M. MÜLLER Manuskripte, Korrekturen und Besprechungsexemplare Manuscripts, -

Maggot Wound Therapy Associated with Wohlfahrtiimonas Chitiniclastica Blood Infection
Open Access Case Report DOI: 10.7759/cureus.12471 Maggot Wound Therapy Associated with Wohlfahrtiimonas chitiniclastica Blood Infection Peter Bueide 1, 2 , Jeff Hunt 1, 2 , Dinesh Bande 1, 2 , Dubert M. Guerrero 1, 2 1. Internal Medicine, University of North Dakota School of Medicine and Health Sciences, Fargo, USA 2. Internal Medicine, Sanford Health, Fargo, USA Corresponding author: Dubert M. Guerrero, [email protected] Abstract Maggot therapy is the intentional application of live, disinfected fly larvae to wounds for debridement and wound care. Although some studies suggest possible beneficial applications for wound healing, subsequent infection is a potential risk of treatment. We present a case of a 70-year-old male with chronic left temporal wound from squamous cell carcinoma treated with maggot therapy complicated by bacteremia with Wohlfahrtiimonas chitiniclastica (W. chitiniclastica). This case illustrates the risk for W. chitiniclastica infection associated with maggots used in medical wound therapy of chronic wounds. Categories: Internal Medicine, Infectious Disease Keywords: maggot, wound, bacteremia Introduction Maggot therapy was made popular during the first world war following the observation that soldiers presenting with maggots in their wounds had a decreased mortality rate than their counterparts [1]. On certain occasions, it is still being used as an alternative treatment option for chronic wounds today [2]. However, much remains unknown regarding the biochemical and physiologic mechanisms underlying the process -

Morphology of the First Instar Larva of Obligatory Traumatic Myiasis Agents (Diptera: Calliphoridae, Sarcophagidae)
Parasitol Res DOI 10.1007/s00436-014-3808-x ORIGINAL PAPER Morphology of the first instar larva of obligatory traumatic myiasis agents (Diptera: Calliphoridae, Sarcophagidae) K. Szpila & M. J. R. Hall & A. H. Wardhana & T. P a p e Received: 13 December 2013 /Accepted: 2 February 2014 # The Author(s) 2014. This article is published with open access at Springerlink.com Abstract There are only three fly species that are obligate information provided by earlier authors. The relatively distant agents of traumatic myiasis of humans and livestock: a single taxonomic position of all three species is evidence that oblig- species of flesh fly, Wohlfahrtia magnifica (Sarcophagidae), atory myiasis has arisen independently, and the extensively and two species of blow flies, Chrysomya bezziana and similar morphology in the first instar larvae of Chrysomya Cochliomyia hominivorax (Calliphoridae). The morphology bezziana, Cochliomyia hominivorax and W.magnifica in com- of their first instar larvae is thoroughly and consistently doc- parison to necrophagous species, especially the enhancement umented here with light microscopy photographs and scan- of the anterior part of the cephaloskeleton and the segmental ning electron microscopy micrographs. The following mor- spinulation, is therefore best interpreted as homoplasic adap- phological structures are documented: pseudocephalon, an- tations to a life strategy as obligate vertebrate parasites. An tennal complex, maxillary palpus, oral ridges, thoracic and identification key for first instar larvae of all obligatory trau- abdominal spinulation, spiracular field, posterior spiracles and matic myiasis agents of mammals is provided. cephaloskeleton. New diagnostic features drawn from the cephaloskeleton and the spinulation of abdominal segments, Keywords Obligatory traumatic myiasis agents . -

First Reported Cases of Urinary Myiasis in Iraq
Crimson Publishers Case Report Wings to the Research First Reported Cases of Urinary Myiasis in Iraq Raghib JH Alshimmre2 and Mohammed B Ismail1* 1Department of Urology (CABMS), Iraq 2Department of Urology (FICMS), Iraq Abstract ISSN: 2689-2707 Myiasis is the infestation by larvae of flies. Myiasis may involve the skin, eyes, nasal passages, gastrointestinal and genitourinary tracts. Cases of urinary myiasis are very rare mostly occurs in immunocompromised hosts, those with previous urologic instrumentation or those with poor socioeconomic status. We present a case of successful outpatient treatment of urinary myiasis in two immunocompetent females without Introductionprior urological history. Myiasis is defined as invasion of the body by the larvae of flies, characterized as cutaneous (subdermal tissue), gastrointestinal, nasopharyngeal, ocular, or urinary, depending on the region invaded [1]. Any infection due to invasion of tissues or cavities of the body by larvae of dipterous insects [2]. The disease occurs predominantly in rural areas and is associated with *Corresponding author: poor hygienic practices. Myiasis producers can be divided into three classes: Ismail, Department of Urology (CABMS), Mohammed B A. Obligate parasites requiring living tissue for larval development. B. Facultative parasites whose larvae usually develop on carrion but may invade College of medicine, Iraq Submission: wounds and Published: February 8, 2020 C. Accidental myiasis [3]-which commonly is enteric, resulting from swallowing March 17, 2020 eggs or larvae with one’s food, i.e. pseudomyiasis can happen when eggs or larvae are Classificationaccidentally deposited on oral or genitourinary opening. HowVolume to 2 -cite Issue this 3 article: First Reported Cases ofRaghib Urinary JH MyiasisAlshimmre, in MohammedIraq B Ismail. -

The First Case of Ignatzschineria Ureiclastica/Larvae in the United States Presenting As a Myiatic Wound Infection
Open Access Case Report DOI: 10.7759/cureus.14518 The First Case of Ignatzschineria ureiclastica/larvae in the United States Presenting as a Myiatic Wound Infection Kasey Reed 1 , Samuel B. Reynolds 2 , Clayton Smith 2 1. Internal Medicine/Pediatrics, University of Louisville School of Medicine, Louisville, USA 2. Internal Medicine, University of Louisville School of Medicine, Louisville, USA Corresponding author: Kasey Reed, [email protected] Abstract Ignatzschineria is a recently identified genus of bacteria that has been isolated from the digestive tract of multiple flies associated with decomposing tissue. Species within this genus are rarely implicated in human disease, and less than 10 cases worldwide have been documented in the literature. Although there have been several documented cases of Ignatzschineria indica bacteremia in the United States (with one previous case in Louisville, KY), this case represents the first documented case of Ignatzschineria ureiclastica/larvae bacteremia in the United States. The natural insect host of this bacteria, parasitic flies that are commonly found among sheep and other livestock, may pose a public health hazard in the city and implicate geographic spread of this bacteria species and its host. Categories: Internal Medicine, Infectious Disease, Public Health Keywords: ignatzschineria, myiasis infestation, ignatzschineria ureiclastica, ignatzschineria larvae, bacteremia Introduction As a bacterial isolate, Ignatzschineria is most commonly found in the digestive tract of Wohlfahrtia magnifica, which is a parasitic fly that plays a significant role in the development of myiatic infections in livestock [1,2]. The patient in this case lived less than five miles from a large swine slaughterhouse in downtown Louisville, Kentucky.