Hypercalcemia in Children and Adolescents Steven A
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

A Novel De Novo 20Q13.32&Ndash;Q13.33
Journal of Human Genetics (2015) 60, 313–317 & 2015 The Japan Society of Human Genetics All rights reserved 1434-5161/15 www.nature.com/jhg ORIGINAL ARTICLE Anovelde novo 20q13.32–q13.33 deletion in a 2-year-old child with poor growth, feeding difficulties and low bone mass Meena Balasubramanian1, Edward Atack2, Kath Smith2 and Michael James Parker1 Interstitial deletions of the long arm of chromosome 20 are rarely reported in the literature. We report a 2-year-old child with a 2.6 Mb deletion of 20q13.32–q13.33, detected by microarray-based comparative genomic hybridization, who presented with poor growth, feeding difficulties, abnormal subcutaneous fat distribution with the lack of adipose tissue on clinical examination, facial dysmorphism and low bone mass. This report adds to rare publications describing constitutional aberrations of chromosome 20q, and adds further evidence to the fact that deletion of the GNAS complex may not always be associated with an Albright’s hereditary osteodystrophy phenotype as described previously. Journal of Human Genetics (2015) 60, 313–317; doi:10.1038/jhg.2015.22; published online 12 March 2015 INTRODUCTION resuscitation immediately after birth and Apgar scores were 9 and 9 at 1 and Reports of isolated subtelomeric deletions of the long arm of 10 min, respectively, of age. Birth parameters were: weight ~ 1.56 kg (0.4th–2nd chromosome 20 are rare, but a few cases have been reported in the centile), length ~ 40 cm (o0.4th centile) and head circumference ~ 28.2 cm o fi literature over the past 30 years.1–13 Traylor et al.12 provided an ( 0.4th centile). -

Review Article Mouse Homologues of Human Hereditary Disease
I Med Genet 1994;31:1-19 I Review article J Med Genet: first published as 10.1136/jmg.31.1.1 on 1 January 1994. Downloaded from Mouse homologues of human hereditary disease A G Searle, J H Edwards, J G Hall Abstract involve homologous loci. In this respect our Details are given of 214 loci known to be genetic knowledge of the laboratory mouse associated with human hereditary dis- outstrips that for all other non-human mam- ease, which have been mapped on both mals. The 829 loci recently assigned to both human and mouse chromosomes. Forty human and mouse chromosomes3 has now two of these have pathological variants in risen to 900, well above comparable figures for both species; in general the mouse vari- other laboratory or farm animals. In a previous ants are similar in their effects to the publication,4 102 loci were listed which were corresponding human ones, but excep- associated with specific human disease, had tions include the Dmd/DMD and Hprt/ mouse homologues, and had been located in HPRT mutations which cause little, if both species. The number has now more than any, harm in mice. Possible reasons for doubled (table 1A). Of particular interest are phenotypic differences are discussed. In those which have pathological variants in both most pathological variants the gene pro- the mouse and humans: these are listed in table duct seems to be absent or greatly 2. Many other pathological mutations have reduced in both species. The extensive been detected and located in the mouse; about data on conserved segments between half these appear to lie in conserved chromo- human and mouse chromosomes are somal segments. -

Pseudohypoparathyroidism Cochlea Thus Being Involved
Arch Dis Child: first published as 10.1136/adc.52.10.798 on 1 October 1977. Downloaded from 798 Short reports vasopressin. Nonetheless, vasopressin being ela- Rose, F. C., Fraser, G. R., Friedman, A. I., and Kohner, E. M. (1966). The association of juvenile diabetes mellitus borated by the cells of the supraoptic hypothalamic and optic atrophy: clinical and genetical aspects. Quarterly nuclei, the diabetes insipidus must represent a Journal of Medicine, 35, 385-405. progressive degeneration of these hypothalamic cells Sunder, J. H., Danowski, T. S., Kenny, F. M., Khurana, or of the supra-optico-hypophyseal tract. R. C., Sun, A., Nolan, S., and Stephan, T. (1972). Pedigrees with diabetes insipidus, diabetes mellitus and optic Many of the reported cases have had urinary 408-412. tract abnormalities ranging from atonic bladder to atrophy. Journal of Medical Genetics, 9, hydronephrosis and hydroureter (Moore, 1971). JOYCE E. RICHARDSON and WILLIAM HAMILTON While congenital absence or progressive degenera- University Department of Child Health, Royal tion of the neural plexus of ureter and bladder is a Hospitalfor Sick Children, Yorkhill, Glasgow G3 8SJ. possible cause, it could be that the diabetes insipidus is contributory to the urinary tract dilatation. Correspondence to Dr. W. Hamilton. Reinvestigation after adequate treatment with vaso- pressin is clearly desirable. The deafness in the syndrome has uniformly been reported to be of high-tone type; the afferent fibres of the cochlear nerve from the basal coils of the Pseudohypoparathyroidism cochlea thus being involved. Published reports give no clear indication that there is progression of the Variable manifestations within a family deafness to suggest involvement of the afferent fibres from the middle and upper cochlear coils. -
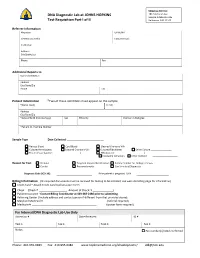
DNA Diagnostic Lab at JOHNS HOPKINS Test Requisition Part I of II
Shipping Address: DNA Diagnostic Lab at JOHNS HOPKINS 1812 Ashland Ave Sample Intake Rm 245 Test Requisition Part I of II Baltimore, MD 21205 Referrer Information Physician UPIN /NPI Genetic Counselor Contact Email: Institution Address City/State/Zip Phone Fax Additional Reports to Name /Institution Address City/State/Zip Phone Fax Patient Information *Two of these identifiers must appear on the sample *Name (Last) (First) Address City/State/Zip *Date of Birth (mm/dd/yyyy) Sex Ethnicity Position in Pedigree *Patient ID / Sample Number Sample Type Date Collected: _________________________ Venous Blood Cord Blood Cleaned Chorionic Villi Cultured Amniocytes Cultured Chorionic Villi Cultured Fibroblasts Other Culture ________________ Frozen tissue (source: _____________________) DNA (source: ______________________) PureGene Extraction Other method Reason for Test Prenatal Targeted Variant Identification Family member for Linkage analysis Carrier Presymptomatic Confirmatory/Diagnostic Diagnosis Code (ICD‐10): If the patient is pregnant: LMP Billing Information (All required documents must be received for testing to be initiated; see web site billing page for information) Credit Card – Attach Credit Card Authorization Form Check (Check # Amount of Check: $ ) Patient Insurance ‐ Contact Billing Coordinator at 443‐287‐2486 prior to submitting. Referring Center (Include address and contact person if different from that provided above) Maryland Medicaid # __________________________________ (referral required) Medicare # ____________________________________________ -

Successful Reversal of Furosemide-Induced Secondary Hyperparathyroidism with Cinacalcet Tarak Srivastava, Shahryar Jafri, William E
Successful Reversal of Tarak Srivastava, MD, a Shahryar Jafri, a William E. Truog, MD, b Judith Sebestyen Furosemide-InducedVanSickle, MD, a Winston M. Manimtim, MD, b Uri S. Alon, MDa Secondary Hyperparathyroidism With Cinacalcet abstract Secondary hyperparathyroidism (SHPT) is a rare complication of furosemide therapy that can occur in patients treated with the loop diuretic for a long period of time. We report a 6-month-old 28-weeks premature infant treated chronically with furosemide for his bronchopulmonary dysplasia, who developed hypocalcemia and severe SHPT, adversely affecting his bones. Discontinuation of the loop diuretic and the addition of supplemental calcium and calcitriol only partially reversed the SHPT, aSections of Nephrology, Bone and Mineral Disorder Clinic, bringing serum parathyroid hormone level down from 553 to 238 pg/mL. and bNeonatology, The Children’s Mercy Hospitals and Clinics, University of Missouri at Kansas City, Kansas City, After introduction of the calcimimetic Cinacalcet, we observed a sustained Missouri normalization of parathyroid hormone concentration at 27 to 63 pg/mL and, with that correction, of all biochemical abnormalities and healing of the Drs Srivastava and Alon conceptualized and designed the study and drafted the initial bone disease. No adverse effects were noted. We conclude that in cases of manuscript; Drs Truog, Manimtim, Sebestyen SHPT due to furosemide in which traditional treatment fails, there may be VanSickle, and Mr Jafri carried out the initial room to consider the addition of a calcimimetic agent. analyses and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted. DOI: https:// doi. org/ 10. 1542/ peds. -

Pseudohypoparathyroidism Vs. Tricho-Rhino- Phalangeal Syndrome: Patient Reclassification
J Pediatr Endocr Met 2014; 27(11-12): 1089–1094 Arrate Peredaa, Sharona Azriela, Mariona Bonet, Intza Garin, Blanca Gener, Beatriz Lecumberri and Guiomar Pérez de Nanclares* Pseudohypoparathyroidism vs. tricho-rhino- phalangeal syndrome: patient reclassification Abstract Keywords: bulbous nose; pseudohypoparathyroidism; pseudopseudohypoparathyroidism; sparse hair; tricho- Objectives: Given that tricho-rhino-phalangeal syndrome rhino-phalangeal syndrome. (TRPS) and pseudohypoparathyroidism/pseudopseudo- hypoparathyroidism (PHP/PPHP) are very rare monogenic disorders that share some features (distinctive facies, DOI 10.1515/jpem-2014-0020 short stature, brachydactyly and, in some patients, intel- Received January 15, 2014; accepted May 8, 2014; previously pub- lished online June 19, 2014 lectual disability) that lead to their misdiagnosis in some cases, our objective was to identify clinical, biochemical or radiological signs that could help to distinguish these two syndromes. Introduction Methods and results: We report on two cases, which were Tricho-rhino-phalangeal syndrome (TRPS-I, OMIM referred to the Endocrinology and Pediatric Endocrinol- #190350; TRPS-III, OMIM #190351) and pseudohypopar- ogy Services for obesity. Clinical evaluation initially sug- athyroidism/pseudopseudohypoparathyroidism (PHP-Ia, gested the diagnosis of PHP-Ia [phenotype suggestive OMIM #103580; PPHP, OMIM #612463) can be clinically of Albright hereditary osteodystrophy (AHO) with para- confused with each other because they have an overlap- thyroid hormone (PTH) resistance] and PPHP (pheno- ping phenotype with rare or subtle dysmorphic features, type resembling AHO, without PTH resistance), but (epi) short stature, brachydactyly and intellectual disability genetic analysis of the GNAS locus ruled out the suspected (1–4). Typical facial dysmorphic traits described in TRPS diagnosis. Further clinical re-evaluation prompted us to [sparse, slowly growing scalp hair; laterally sparse eye- suspect TRPS, and this was confirmed genetically. -

Case Reports in Clinical Practice Brachymetatarsia; How Important
Case Reports in Clinical Practice VOL 3, NO 2, 2018 Case Report Brachymetatarsia; How Important Can It Be in Adolescence? 1 2* 2 Mojgan Mirabdolhagh , Sahar Karimpour Reyhan , Mahsa Abbaszadeh 1- Endocrinology and Metabolism Research Center (EMRC), Vali-Asr Hospital, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran 2- Department of Medicine Internal, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran Received: 29 March 2018 Revised: 18 April 2018 Accepted: 12 May 2018 ARTICLE INFO ABSTRACT Corresponding author: Hypocalcaemia is a dangerous electrolyte imbalance with 18% Sahar Karimpour Reyhan prevalence in hospital admitted patients. 1 Regulation of calcium level is by 3 main calcium-regulating hormones. These hormones are Email: parathyroid hormone (PTH), vitamin D, and calcitonin; and they act by [email protected] effecting on the bowel, kidneys, and skeleton. Causes of Keywords: hypocalcaemia includes vitamin D deficiency, hypoparathyroidism, Hypocalcaemia; renal diseases, hypomagnesaemia, hungry bone disease after Adolescence; parathyroidectomy, drugs like calcium chelators, massive blood Pseudohypoparathyro transfusion, critical illness, parathyroid hormone resistance, vitamin D idism (PHP) resistance. Pseudohypoparathyroidism (PHP) refers to a group of metabolic disorders in which resistance to parathyroid hormone leads to hypocalcaemia, hyperphosphatemia, and elevation of serum PTH level in the setting of normal renal function. Herein we report an interesting case of hypocalcaemia who came to the emergency department with suspicion to intracranial hemorrhage and lead to the diagnosis of pseudohypoparathyroidism. Citation: Mirabdolhagh M, Karimpour Reyhan S, Abbaszadeh M. Brachymetatarsia; How Important Can It Be in Adolescence? Case Rep Clin Pract 2018; 3(2): 38-41. Introduction skeleton, respectively (2). -

Assessment of Clinical Workload for General and Specialty Genetic Counsellors at an Academic Medical Center: a Tool for Evaluating Genetic Counselling Practices
www.nature.com/npjgenmed All rights reserved 2056-7944/16 ARTICLE OPEN Assessment of clinical workload for general and specialty genetic counsellors at an academic medical center: a tool for evaluating genetic counselling practices Brandie Heald1, Lisa Rybicki2, Diane Clements1, Jessica Marquard1, Jessica Mester1, Ryan Noss1, Monica Nardini1, Jill Polk1, Brittany Psensky1, Christina Rigelsky1, Allison Schreiber1, Amy Shealy1, Marissa Smith1 and Charis Eng1,2 With genomics influencing clinical decisions, genetics professionals are exponentially called upon as part of multidisciplinary care. Increasing demand for genetic counselling, a limited workforce, necessitates practices improve efficiency. We hypothesised that distinct differences in clinical workload exist between various disciplines of genetic counselling, complicating practice standardisation and patient volume expectations. We thus sought to objectively define and assess workload among various specialties of genetic counselling. Twelve genetic counsellors (GCs), representing 9.3 clinical FTE, in general or specialty (cancer, cardiovascular or prenatal) services at an academic health system developed a data collection tool for assessing time and complexity. Over a 6-week period, the data were recorded for 583 patient visits (136 general and 447 specialty) and analysed comparing general versus specialty GCs. Variables were compared with hierarchical linear models for ordinal or continuous data and hierarchical logistic models for binary data. General GCs completed more pre- and post-visit activities (P = 0.011) and spent more time (P = 0.009) per case. General GCs reported greater case discussion with other providers (Po0.001), literature review (P = 0.026), exploring testing options (P = 0.041), electronic medical record review (P = 0.040), insurance preauthorization (P = 0.05) and fielding patient inquiries (P = 0.003). -

Downloaded from Bioscientifica.Com at 09/29/2021 10:33:54AM Via Free Access
ID: 20-0615 10 5 A Zervas et al. The endocrine fairytale 10:5 R189–R199 REVIEW Snow White and the Seven Dwarfs: a fairytale for endocrinologists Athanasios Zervas1, George Chrousos2,3 and Sarantis Livadas1 1Endocrine Unit, Athens Medical Centre, Athens, Greece 2Division of Endocrinology, Metabolism and Diabetes, First Department of Pediatrics, University Research Institute of Maternal and Child Health and Precision Medicine, and UNESCO Chair on Adolescent Health Care, National and Kapodistrian University of Athens, Athens, Greece 3National and Kapodistrian University of Athens Medical School, ‘Aghia Sophia’ Children’s Hospital, Athens, Greece Correspondence should be addressed to S Livadas: [email protected] Abstract ‘Snow White and the Seven Dwarfs’, a fairytale that is widely known across the Western Key Words world, was originally written by the Brothers Grimm, and published in 1812 as ‘Snow White’. f growth Though each dwarf was first given an individual name in the 1912 Broadway play, in Walt f dwarfism Disney’s 1937 film ‘Snow White and the Seven Dwarfs’, they were renamed, and the dwarfs f pituitary have become household names. It is well known that myths, fables, and fairytales, though f pseudohypoparathyroidism appearing to be merely children’s tales about fictional magical beings and places, have, more often than not, originated from real facts. Therefore, the presence of the seven brothers with short stature in the story is, from an endocrinological point of view, highly intriguing, in fact, thrilling. The diversity of the phenotypes among the seven dwarfs is also stimulating, although puzzling. We undertook a differential diagnosis of their common underlying disorder based on the original Disney production’s drawings and the unique characteristics of these little gentlemen, while we additionally evaluated several causes of short stature and, focusing on endocrine disorders that could lead to these clinical features among siblings, we have, we believe, been able to reveal the underlying disease depicted in Endocrine Connections this archetypal tale. -

Ocular Manifestations of Inherited Diseases Maya Eibschitz-Tsimhoni
10 Ocular Manifestations of Inherited Diseases Maya Eibschitz-Tsimhoni ecognizing an ocular abnormality may be the first step in Ridentifying an inherited condition or syndrome. Identifying an inherited condition may corroborate a presumptive diagno- sis, guide subsequent management, provide valuable prognostic information for the patient, and determine if genetic counseling is needed. Syndromes with prominent ocular findings are listed in Table 10-1, along with their alternative names. By no means is this a complete listing. Two-hundred and thirty-five of approxi- mately 1900 syndromes associated with ocular or periocular manifestations (both inherited and noninherited) identified in the medical literature were chosen for this chapter. These syn- dromes were selected on the basis of their frequency, the char- acteristic or unique systemic or ocular findings present, as well as their recognition within the medical literature. The boldfaced terms are discussed further in Table 10-2. Table 10-2 provides a brief overview of the common ocular and systemic findings for these syndromes. The table is organ- ized alphabetically; the boldface name of a syndrome is followed by a common alternative name when appropriate. Next, the Online Mendelian Inheritance in Man (OMIM™) index num- ber is listed. By accessing the OMIM™ website maintained by the National Center for Biotechnology Information at http://www.ncbi.nlm.nih.gov, the reader can supplement the material in the chapter with the latest research available on that syndrome. A MIM number without a prefix means that the mode of inheritance has not been proven. The prefix (*) in front of a MIM number means that the phenotype determined by the gene at a given locus is separate from those represented by other 526 chapter 10: ocular manifestations of inherited diseases 527 asterisked entries and that the mode of inheritance of the phe- notype has been proven. -

Congenital Hand Anomalies and Associated Syndromes Ghazi M
Congenital Hand Anomalies and Associated Syndromes Ghazi M. Rayan • Joseph Upton III Congenital Hand Anomalies and Associated Syndromes Editors Ghazi M. Rayan Joseph Upton III INTEGRIS Baptist Medical Center Chestnut Hill, USA Orthopaedic Surgery – Hand Oklahoma City, USA ISBN 978-3-642-54609-9 ISBN 978-3-642-54610-5 (eBook) DOI 10.1007/978-3-642-54610-5 Library of Congress Control Number: 2014946208 Springer © Springer-Verlag Berlin Heidelberg 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the mate- rial is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter devel- oped. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provi- sions of the Copyright Law of the Publisher´s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use.