Successful Reversal of Furosemide-Induced Secondary Hyperparathyroidism with Cinacalcet Tarak Srivastava, Shahryar Jafri, William E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Calcimimetic Use in Dialysis-Dependent
Kidney360 Publish Ahead of Print, published on August 25, 2020 as doi:10.34067/KID.0003042020 Calcimimetic Use in Dialysis-Dependent Medicare Fee-for-Service Beneficiaries and Implications for Bundled Payment Mark Gooding1, Pooja Desai2, Holly Owens3, Allison A. Petrilla1, Mahesh Kambhampati1, Zach Levine1, Joanna Young1, Jack Fagan1, Robert Rubin4 1. Avalere Health, Washington, DC 2. Amgen, Inc., Global Health Economics, Thousand Oaks, CA 3. Amgen, Inc., US Government Affairs and Policy, Washington, DC 4. Georgetown University, Bethesda, MD Corresponding Author: Mark Gooding Avalere Health 1201 New York Avenue, NW Suite 1000 Washington, DC 2005 202-355-6096 [email protected] Copyright 2020 by American Society of Nephrology. Abstract: Background: Dialysis-dependent patients with secondary hyperparathyroidism (SHPT) may require calcimimetics to reduce parathyroid hormone levels to treatment goals. Medicare currently utilizes the Transitional Drug Add-on Payment Adjustment (TDAPA) designation under the ESRD Prospective Payment System (“bundled payment”) to pay for calcimimetics (the first products eligible for the adjustment); this payment designation for calcimimetics is expected to conclude after 2020. This study explores variability in calcimimetic use across key patient characteristics and its potential impact on policy options for incorporating calcimimetics permanently into the bundle. Methods: This descriptive analysis used the 100% sample of Medicare FFS Part B (outpatient) 2018 claims to describe national, regional, and patient-level variation (including race, dual eligibility, and dialysis vintage) in calcimimetic utilization among dialysis-dependent beneficiaries. Results: A total of 373,874 beneficiaries were analyzed, 28% had >90 days of calcimimetic use during 2018. At the national level, the proportion of dialysis patients utilizing calcimimetics was roughly 80% higher in African-American vs. -

Effects of the Calcimimetic Cinacalcet Hcl on Cardiovascular Disease, Fracture, and Health-Related Quality of Life in Secondary Hyperparathyroidism
Kidney International, Vol. 68 (2005), pp. 1793–1800 Effects of the calcimimetic cinacalcet HCl on cardiovascular disease, fracture, and health-related quality of life in secondary hyperparathyroidism JOHN CUNNINGHAM,MARK DANESE,KURT OLSON,PRESTON KLASSEN, and GLENN M. CHERTOW University College London, The Middlesex Hospital, London, UK; Outcomes Insights, Inc., Newbury Park, California; Amgen, Inc., Thousand Oaks, California; and Department of Medicine, University of California, San Francisco, California Effects of the calcimimetic cinacalcet HCl on cardiovascular tion and diminished pain. These data suggest that, in addition disease, fracture, and health-related quality of life in secondary to its effects on PTH and mineral metabolism, cinacalcet had hyperparathyroidism. favorable effects on important clinical outcomes. Background. Secondary hyperparathyroidism (HPT) and ab- normal mineral metabolism are thought to play an important role in bone and cardiovascular disease in patients with chronic kidney disease. Cinacalcet, a calcimimetic that modulates the Secondary hyperparathyroidism (HPT) is a frequent calcium-sensing receptor, reduces parathyroid hormone (PTH) secretion and lowers serum calcium and phosphorus concen- component of the natural progression of chronic kidney trations in patients with end-stage renal disease (ESRD) and disease (CKD), typically developing when the glomeru- secondary HPT. lar filtration rate (GFR) drops below approximately Methods. We undertook a combined analysis of safety data 80 mL/min/1.73m2 for ≥3 months [1]. Secondary HPT (parathyroidectomy, fracture, hospitalizations, and mortality) is an adaptive response to CKD and arises from dis- from 4 similarly designed randomized, double-blind, placebo- controlled clinical trials enrolling 1184 subjects (697 cinacalcet, ruptions in the homeostatic control of serum calcium, 487 control) with ESRD and uncontrolled secondary HPT (in- serum phosphorus, and vitamin D, which are associated tact PTH ≥300 pg/mL). -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

A Novel De Novo 20Q13.32&Ndash;Q13.33
Journal of Human Genetics (2015) 60, 313–317 & 2015 The Japan Society of Human Genetics All rights reserved 1434-5161/15 www.nature.com/jhg ORIGINAL ARTICLE Anovelde novo 20q13.32–q13.33 deletion in a 2-year-old child with poor growth, feeding difficulties and low bone mass Meena Balasubramanian1, Edward Atack2, Kath Smith2 and Michael James Parker1 Interstitial deletions of the long arm of chromosome 20 are rarely reported in the literature. We report a 2-year-old child with a 2.6 Mb deletion of 20q13.32–q13.33, detected by microarray-based comparative genomic hybridization, who presented with poor growth, feeding difficulties, abnormal subcutaneous fat distribution with the lack of adipose tissue on clinical examination, facial dysmorphism and low bone mass. This report adds to rare publications describing constitutional aberrations of chromosome 20q, and adds further evidence to the fact that deletion of the GNAS complex may not always be associated with an Albright’s hereditary osteodystrophy phenotype as described previously. Journal of Human Genetics (2015) 60, 313–317; doi:10.1038/jhg.2015.22; published online 12 March 2015 INTRODUCTION resuscitation immediately after birth and Apgar scores were 9 and 9 at 1 and Reports of isolated subtelomeric deletions of the long arm of 10 min, respectively, of age. Birth parameters were: weight ~ 1.56 kg (0.4th–2nd chromosome 20 are rare, but a few cases have been reported in the centile), length ~ 40 cm (o0.4th centile) and head circumference ~ 28.2 cm o fi literature over the past 30 years.1–13 Traylor et al.12 provided an ( 0.4th centile). -

Review Article Mouse Homologues of Human Hereditary Disease
I Med Genet 1994;31:1-19 I Review article J Med Genet: first published as 10.1136/jmg.31.1.1 on 1 January 1994. Downloaded from Mouse homologues of human hereditary disease A G Searle, J H Edwards, J G Hall Abstract involve homologous loci. In this respect our Details are given of 214 loci known to be genetic knowledge of the laboratory mouse associated with human hereditary dis- outstrips that for all other non-human mam- ease, which have been mapped on both mals. The 829 loci recently assigned to both human and mouse chromosomes. Forty human and mouse chromosomes3 has now two of these have pathological variants in risen to 900, well above comparable figures for both species; in general the mouse vari- other laboratory or farm animals. In a previous ants are similar in their effects to the publication,4 102 loci were listed which were corresponding human ones, but excep- associated with specific human disease, had tions include the Dmd/DMD and Hprt/ mouse homologues, and had been located in HPRT mutations which cause little, if both species. The number has now more than any, harm in mice. Possible reasons for doubled (table 1A). Of particular interest are phenotypic differences are discussed. In those which have pathological variants in both most pathological variants the gene pro- the mouse and humans: these are listed in table duct seems to be absent or greatly 2. Many other pathological mutations have reduced in both species. The extensive been detected and located in the mouse; about data on conserved segments between half these appear to lie in conserved chromo- human and mouse chromosomes are somal segments. -

Pseudohypoparathyroidism Cochlea Thus Being Involved
Arch Dis Child: first published as 10.1136/adc.52.10.798 on 1 October 1977. Downloaded from 798 Short reports vasopressin. Nonetheless, vasopressin being ela- Rose, F. C., Fraser, G. R., Friedman, A. I., and Kohner, E. M. (1966). The association of juvenile diabetes mellitus borated by the cells of the supraoptic hypothalamic and optic atrophy: clinical and genetical aspects. Quarterly nuclei, the diabetes insipidus must represent a Journal of Medicine, 35, 385-405. progressive degeneration of these hypothalamic cells Sunder, J. H., Danowski, T. S., Kenny, F. M., Khurana, or of the supra-optico-hypophyseal tract. R. C., Sun, A., Nolan, S., and Stephan, T. (1972). Pedigrees with diabetes insipidus, diabetes mellitus and optic Many of the reported cases have had urinary 408-412. tract abnormalities ranging from atonic bladder to atrophy. Journal of Medical Genetics, 9, hydronephrosis and hydroureter (Moore, 1971). JOYCE E. RICHARDSON and WILLIAM HAMILTON While congenital absence or progressive degenera- University Department of Child Health, Royal tion of the neural plexus of ureter and bladder is a Hospitalfor Sick Children, Yorkhill, Glasgow G3 8SJ. possible cause, it could be that the diabetes insipidus is contributory to the urinary tract dilatation. Correspondence to Dr. W. Hamilton. Reinvestigation after adequate treatment with vaso- pressin is clearly desirable. The deafness in the syndrome has uniformly been reported to be of high-tone type; the afferent fibres of the cochlear nerve from the basal coils of the Pseudohypoparathyroidism cochlea thus being involved. Published reports give no clear indication that there is progression of the Variable manifestations within a family deafness to suggest involvement of the afferent fibres from the middle and upper cochlear coils. -

208325Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208325Orig1s000 SUMMARY REVIEW Cross Discipline Team Leader Review of secondary hyperparathyroidism in patients with chronic kidney disease on hemodialysis from the label (b) (4) . Proprietary Name The proposed proprietary name for etelcalcetide, Parsabiv, was reassessed and deemed acceptable by the Office of Medication Error Prevention and Risk Management (refer to the review from 1/3/2017). A letter stating this was issued to the Applicant on 1/3/2017. Safety Update Updated safety data on 884 patients with CKD on hemodialysis participating in an, ongoing, long-term, open-label, extension study (i.e., Study 20130213 or Study 213 for short) was included in the current submission and reviewed by Dr. Sullivan. The new data covers the period from July 18, 2015 (the date of the last 120-day safety update included in the original application and reviewed by the Division) to October 6, 2016 (database lock for re- submission). Dr. Sullivan concludes that the reported causes of death and SAEs in this interim analysis are not unexpected in a population of patients with CKD requiring hemodialysis and who are at high risk for cardiovascular disease and infection. She assessed the rates of adverse events as comparable to those observed in the original submission and did not identify new adverse events current submission. In the current submission, the Applicant provided updated information and analyses related to events of fatal gastro-intestinal bleeds based on re-review of the data in Amgen’s Global Safety Database (AGSD). Three additional cases of fatal GIB were identified by the Applicant since the last review cycle for a total of 10 fatal GI bleed in patients treated with etelcalcetide in the etelcalcetide clinical program to date. -
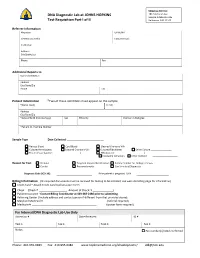
DNA Diagnostic Lab at JOHNS HOPKINS Test Requisition Part I of II
Shipping Address: DNA Diagnostic Lab at JOHNS HOPKINS 1812 Ashland Ave Sample Intake Rm 245 Test Requisition Part I of II Baltimore, MD 21205 Referrer Information Physician UPIN /NPI Genetic Counselor Contact Email: Institution Address City/State/Zip Phone Fax Additional Reports to Name /Institution Address City/State/Zip Phone Fax Patient Information *Two of these identifiers must appear on the sample *Name (Last) (First) Address City/State/Zip *Date of Birth (mm/dd/yyyy) Sex Ethnicity Position in Pedigree *Patient ID / Sample Number Sample Type Date Collected: _________________________ Venous Blood Cord Blood Cleaned Chorionic Villi Cultured Amniocytes Cultured Chorionic Villi Cultured Fibroblasts Other Culture ________________ Frozen tissue (source: _____________________) DNA (source: ______________________) PureGene Extraction Other method Reason for Test Prenatal Targeted Variant Identification Family member for Linkage analysis Carrier Presymptomatic Confirmatory/Diagnostic Diagnosis Code (ICD‐10): If the patient is pregnant: LMP Billing Information (All required documents must be received for testing to be initiated; see web site billing page for information) Credit Card – Attach Credit Card Authorization Form Check (Check # Amount of Check: $ ) Patient Insurance ‐ Contact Billing Coordinator at 443‐287‐2486 prior to submitting. Referring Center (Include address and contact person if different from that provided above) Maryland Medicaid # __________________________________ (referral required) Medicare # ____________________________________________ -

Pseudohypoparathyroidism Vs. Tricho-Rhino- Phalangeal Syndrome: Patient Reclassification
J Pediatr Endocr Met 2014; 27(11-12): 1089–1094 Arrate Peredaa, Sharona Azriela, Mariona Bonet, Intza Garin, Blanca Gener, Beatriz Lecumberri and Guiomar Pérez de Nanclares* Pseudohypoparathyroidism vs. tricho-rhino- phalangeal syndrome: patient reclassification Abstract Keywords: bulbous nose; pseudohypoparathyroidism; pseudopseudohypoparathyroidism; sparse hair; tricho- Objectives: Given that tricho-rhino-phalangeal syndrome rhino-phalangeal syndrome. (TRPS) and pseudohypoparathyroidism/pseudopseudo- hypoparathyroidism (PHP/PPHP) are very rare monogenic disorders that share some features (distinctive facies, DOI 10.1515/jpem-2014-0020 short stature, brachydactyly and, in some patients, intel- Received January 15, 2014; accepted May 8, 2014; previously pub- lished online June 19, 2014 lectual disability) that lead to their misdiagnosis in some cases, our objective was to identify clinical, biochemical or radiological signs that could help to distinguish these two syndromes. Introduction Methods and results: We report on two cases, which were Tricho-rhino-phalangeal syndrome (TRPS-I, OMIM referred to the Endocrinology and Pediatric Endocrinol- #190350; TRPS-III, OMIM #190351) and pseudohypopar- ogy Services for obesity. Clinical evaluation initially sug- athyroidism/pseudopseudohypoparathyroidism (PHP-Ia, gested the diagnosis of PHP-Ia [phenotype suggestive OMIM #103580; PPHP, OMIM #612463) can be clinically of Albright hereditary osteodystrophy (AHO) with para- confused with each other because they have an overlap- thyroid hormone (PTH) resistance] and PPHP (pheno- ping phenotype with rare or subtle dysmorphic features, type resembling AHO, without PTH resistance), but (epi) short stature, brachydactyly and intellectual disability genetic analysis of the GNAS locus ruled out the suspected (1–4). Typical facial dysmorphic traits described in TRPS diagnosis. Further clinical re-evaluation prompted us to [sparse, slowly growing scalp hair; laterally sparse eye- suspect TRPS, and this was confirmed genetically. -

Case Reports in Clinical Practice Brachymetatarsia; How Important
Case Reports in Clinical Practice VOL 3, NO 2, 2018 Case Report Brachymetatarsia; How Important Can It Be in Adolescence? 1 2* 2 Mojgan Mirabdolhagh , Sahar Karimpour Reyhan , Mahsa Abbaszadeh 1- Endocrinology and Metabolism Research Center (EMRC), Vali-Asr Hospital, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran 2- Department of Medicine Internal, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran Received: 29 March 2018 Revised: 18 April 2018 Accepted: 12 May 2018 ARTICLE INFO ABSTRACT Corresponding author: Hypocalcaemia is a dangerous electrolyte imbalance with 18% Sahar Karimpour Reyhan prevalence in hospital admitted patients. 1 Regulation of calcium level is by 3 main calcium-regulating hormones. These hormones are Email: parathyroid hormone (PTH), vitamin D, and calcitonin; and they act by [email protected] effecting on the bowel, kidneys, and skeleton. Causes of Keywords: hypocalcaemia includes vitamin D deficiency, hypoparathyroidism, Hypocalcaemia; renal diseases, hypomagnesaemia, hungry bone disease after Adolescence; parathyroidectomy, drugs like calcium chelators, massive blood Pseudohypoparathyro transfusion, critical illness, parathyroid hormone resistance, vitamin D idism (PHP) resistance. Pseudohypoparathyroidism (PHP) refers to a group of metabolic disorders in which resistance to parathyroid hormone leads to hypocalcaemia, hyperphosphatemia, and elevation of serum PTH level in the setting of normal renal function. Herein we report an interesting case of hypocalcaemia who came to the emergency department with suspicion to intracranial hemorrhage and lead to the diagnosis of pseudohypoparathyroidism. Citation: Mirabdolhagh M, Karimpour Reyhan S, Abbaszadeh M. Brachymetatarsia; How Important Can It Be in Adolescence? Case Rep Clin Pract 2018; 3(2): 38-41. Introduction skeleton, respectively (2). -

Assessment of Clinical Workload for General and Specialty Genetic Counsellors at an Academic Medical Center: a Tool for Evaluating Genetic Counselling Practices
www.nature.com/npjgenmed All rights reserved 2056-7944/16 ARTICLE OPEN Assessment of clinical workload for general and specialty genetic counsellors at an academic medical center: a tool for evaluating genetic counselling practices Brandie Heald1, Lisa Rybicki2, Diane Clements1, Jessica Marquard1, Jessica Mester1, Ryan Noss1, Monica Nardini1, Jill Polk1, Brittany Psensky1, Christina Rigelsky1, Allison Schreiber1, Amy Shealy1, Marissa Smith1 and Charis Eng1,2 With genomics influencing clinical decisions, genetics professionals are exponentially called upon as part of multidisciplinary care. Increasing demand for genetic counselling, a limited workforce, necessitates practices improve efficiency. We hypothesised that distinct differences in clinical workload exist between various disciplines of genetic counselling, complicating practice standardisation and patient volume expectations. We thus sought to objectively define and assess workload among various specialties of genetic counselling. Twelve genetic counsellors (GCs), representing 9.3 clinical FTE, in general or specialty (cancer, cardiovascular or prenatal) services at an academic health system developed a data collection tool for assessing time and complexity. Over a 6-week period, the data were recorded for 583 patient visits (136 general and 447 specialty) and analysed comparing general versus specialty GCs. Variables were compared with hierarchical linear models for ordinal or continuous data and hierarchical logistic models for binary data. General GCs completed more pre- and post-visit activities (P = 0.011) and spent more time (P = 0.009) per case. General GCs reported greater case discussion with other providers (Po0.001), literature review (P = 0.026), exploring testing options (P = 0.041), electronic medical record review (P = 0.040), insurance preauthorization (P = 0.05) and fielding patient inquiries (P = 0.003). -

Management of Renal Bone Disease
Management of renal bone disease Darren M Roberts, Advanced Trainee, and Richard F Singer, Staff Specialist, Department of Renal Medicine, The Canberra Hospital Summary Calcium and phosphate physiology Renal bone disease occurs in patients with Plasma concentrations of calcium and phosphate are chronic kidney disease. There are changes in the normally tightly regulated. Calcium absorption from the gut is concentrations of calcium, phosphate, vitamin D stimulated by calcitriol whereas phosphate absorption largely varies with dietary intake and has less regulation by calcitriol. and parathyroid hormone. Systemic complications Most of the absorbed calcium and phosphate is stored in the include renal osteodystrophy and soft tissue bones with very small amounts present in the circulation. Both calcification, which contribute to morbidity and calcium and phosphate are filtered at the glomerulus. Calcium mortality. As the changes of renal bone disease reabsorption is regulated by a calcium sensing receptor and are potentially modifiable, early referral to a increased by parathyroid hormone. Phosphate reabsorption nephrologist for monitoring and treatment is is decreased by parathyroid hormone and fibroblast growth recommended. Early advice about diet and regular factor-23 and increased by calcitriol (see Fig. 1 online). monitoring of calcium, phosphate and parathyroid Calcitriol and vitamin D hormone are necessary. Careful prescribing of Vitamin D (calciferol) is synthesised in vivo by photoactivation drugs and dialysis to achieve specific biochemical of steroid precursors in the skin. Calciferol is hydroxylated targets can minimise the complications. Phosphate in the liver to calcidiol (25-hydroxycalciferol) which is binders and vitamin D analogues are required by subsequently bioactivated to calcitriol (1,25-dihydroxycalciferol) most patients with advanced renal failure.