'Medicine in Context'
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UC Berkeley UC Berkeley Electronic Theses and Dissertations
UC Berkeley UC Berkeley Electronic Theses and Dissertations Title Ripples, Echoes, and Reverberations: 1965 and Now in Indonesia Permalink https://escholarship.org/uc/item/5fv121wm Author Stroud, Martha Publication Date 2015 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California Ripples, Echoes, and Reverberations: 1965 and Now in Indonesia by Martha Stroud A dissertation submitted in partial satisfaction of the requirements for the degree Joint Doctor of Philosophy with University of California, San Francisco in Medical Anthropology in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Nancy Scheper-Hughes, Chair Professor Laura Nader Professor Sharon Kaufman Professor Jeffrey A. Hadler Spring 2015 “Ripples, Echoes, and Reverberations: 1965 and Now in Indonesia” © 2015 Martha Stroud 1 Abstract Ripples, Echoes, and Reverberations: 1965 and Now in Indonesia by Martha Stroud Joint Doctor of Philosophy with University of California, San Francisco in Medical Anthropology University of California, Berkeley Professor Nancy Scheper-Hughes, Chair In Indonesia, during six months in 1965-1966, between half a million and a million people were killed during a purge of suspected Communist Party members after a purported failed coup d’état blamed on the Communist Party. Hundreds of thousands of Indonesians were imprisoned without trial, many for more than a decade. The regime that orchestrated the mass killings and detentions remained in power for over 30 years, suppressing public discussion of these events. It was not until 1998 that Indonesians were finally “free” to discuss this tragic chapter of Indonesian history. In this dissertation, I investigate how Indonesians perceive and describe the relationship between the past and the present when it comes to the events of 1965-1966 and their aftermath. -

Culture, Health and Illness (Introduction to Medical Anthropology)
Department of Anthropology, University of British Columbia Anthropology 227.001 Winter 2007 Culture, Health and Illness (Introduction to Medical Anthropology) Instructor Teaching Assistant Dr. Vinay R. Kamat Stephen Robbins Class: Mon, Wed, Fri 10:00 a.m. to 11:00 a.m. Office: ANSO 0305 Lasserre, 6333 Memorial Road, Room 104 Office hours: Mon, Wed, 11:00-12:00 Office: ANSO 2319; Office phone 604-822-4802 Email: [email protected] Office hours: Mon, Wed, 11:30 a.m. to 1:00 p.m. Email: [email protected] Course Description This is an introductory course in medical anthropology which includes the study of health, illness and healing from a cross-cultural perspective. The course examines aspects of health and illness from a biocultural perspective. In reading ethnographic materials from Western and non-Western settings, we will explore how medical anthropologists creatively use different theoretical and methodological approaches to understand and highlight how health, illness and healing practices are culturally constructed and mediated. The case studies and other required readings will help us learn to appreciate the contribution of medical anthropology to the study of international public health problems including specific life-threatening diseases such as HIV/ AIDS, tuberculosis and malaria. Topics covered by this course include cultural interpretations of sickness and healing, medical systems as social systems, medical pluralism, belief and ethnomedical systems, medical decision making, social relations of therapy management, cultural construction of efficacy and “side-effects,” pharmaceuticalization of health, explanatory models, cultural competence, narrative representation of illness, the body and debate surrounding female genital mutilation/ cutting, the political economy of HIV/AIDS in Africa, structural violence and social suffering, the New Genetics and social stigma. -
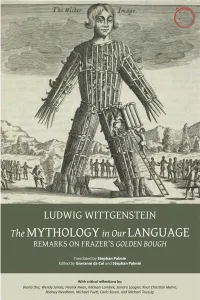
The Mythology in Our Language
THE MYTHOLOGY IN OUR LANGUAGE THE MYTHOLOGY IN OUR LANGUAGE Remarks on Frazer’s Golden Bough Translated by Stephan Palmié Edited by Giovanni da Col and Stephan Palmié With critical reflections by Veena Das, Wendy James, Heonik Kwon, Michael Lambek, Sandra Laugier, Knut Christian Myhre, Rodney Needham, Michael Puett, Carlo Severi, and Michael Taussig Hau Books Chicago © 2018 Hau Books and Ludwig Wittgenstein, Stephan Palmié, Giovanni da Col, Veena Das, Wendy James, Heonik Kwon, Michael Lambek, Sandra Laugier, Knut Christian Myhre, Rodney Needham, Michael Puett, Carlo Severi, and Michael Taussig Cover: “A wicker man, filled with human sacrifices (071937)” © The British Library Board. C.83.k.2, opposite 105. Cover and layout design: Sheehan Moore Editorial office: Michelle Beckett, Justin Dyer, Sheehan Moore, Faun Rice, and Ian Tuttle Typesetting: Prepress Plus (www.prepressplus.in) ISBN: 978-1-912808-40-3 LCCN: 2018962822 Hau Books Chicago Distribution Center 11030 S. Langley Chicago, IL 60628 www.haubooks.com Hau Books is printed, marketed, and distributed by The University of Chicago Press. www.press.uchicago.edu Printed in the United States of America on acid-free paper. Table of Contents Preface xi chapter 1 Translation is Not Explanation: Remarks on the Intellectual History and Context of Wittgenstein’s Remarks on Frazer 1 Stephan Palmié chapter 2 Remarks on Frazer’s The Golden Bough 29 Ludwig Wittgenstein, translated by Stephan Palmié chapter 3 On Wittgenstein’s Remarks on Frazer’s Golden Bough 75 Carlo Severi chapter 4 Wittgenstein’s -

Erica Caple James
Erica Caple James MIT Anthropology Program 77 Massachusetts Avenue Room E53-335G Cambridge, MA 02139-4307 (617) 253-7321 [email protected] EDUCATION Harvard University, Ph.D. in Social Anthropology 2003 Harvard University, A.M. in Social Anthropology 1998 Harvard Divinity School, Masters of Theological Studies (M.T.S.) 1995 Princeton University, A.B. in Anthropology 1992 DISSERTATION “The Violence of Misery: ‘Insecurity’ in Haiti in the ‘Democratic’ Era” Advisor: Dr. Arthur Kleinman FELLOWSHIPS AND HONORS Abdul Latif Jameel World Water and Food Security Lab Grant 2015-2017 Todman Family Fund, for launch of Global Health and Medical Humanities Initiative 2014 Alumni Class Funds 2014 Tenure, Massachusetts Institute of Technology 2013 Gordon K. and Sybille Lewis (Book) Award, Caribbean Studies Association 2013 School for Advanced Research on the Human Experience, Advanced Seminar 2013 James A. and Ruth Levitan Prize in the Humanities, MIT 2012 Gregory Bateson Book Prize, Society for Cultural Anthropology, Honorable Mention 2011 MIT Old Dominion Fellowship 2011 Class of 1947 Career Development Professorship 2010 Rita E. Hauser Fellow, Radcliffe Institute for Advanced Study 2010-2011 MIT School of the Humanities, Arts, and Social Sciences Research Fund 2009 NIH National Loan Repayment Program Funding for Health Disparities Research 2007-2009 Career Enhancement Fellowship, Woodrow Wilson National Fellowship Foundation, 2007 Honorable Mention Mellon Foundation Support for the Study of Science, Technology, and Medicine 2006 School of the Humanities, -

INTRODUCTION a Concept Note
INTRODUCTION A Concept Note Clara Han and Veena Das Dōgen, a thirteenth-century Buddhist scholar from Japan, provocatively reversed the commonsense notion of life and death, which takes birth as the inception of a linear stretch of time over which a particular life is lived and death as the moment of cessation of that time. Instead, he thought that within Buddhist practice and hence within each moment, life and death can be seen as working together. What if we took such ways of conceptualizing the relation between life and death as present not only in exotic practices but also in concepts generated from the experiences of everyday life and its perils? Then we could become attentive to the multiple forms in which human societies generate understanding of life that comes from their varied experiences of how living and dying have been transformed in our contemporary conditions. This book is conceived as a response to the idea that our concepts are honed from the everyday experiences to which the people we study struggle to give expression, and to the idea that we ourselves become apprentices to death as we survey the altered landscape on which life and death become conjoined in our contemporary world. Our intention in this introductory chapter is not to summarize the chapters that follow: the section introductions show how the particular chapters in each section take forward the ways in which life and death are folded together in the lives of individuals and communities. Here we want to reflect on how anthropo- logical conceptions of life have absorbed the discussion of these issues from philosophy and from the history of medicine even as the anthropological attention to the concrete- ness of lives and deaths has put pressure on the abstract formulations of these other disciplines. -

Current Anthropology October 2015 Volume 56 Supplement 11 Pages S1–S180
Forthcoming Current Anthropology Wenner-Gren Symposium Current Anthropology Supplementary Issues (in order of appearance) VOLUME 56 SUPPLEMENT 11 OCTOBER 2015 The Life and Death of the Secret. Lenore Manderson, Mark Davis, and Current Chip Colwell, eds. Reintegrating Anthropology: From Inside Out. Agustín Fuentes and Polly Wiessner, eds. Anthropology Previously Published Supplementary Issues Working Memory: Beyond Language and Symbolism. Thomas Wynn and Frederick L. Coolidge, eds. THE WENNER-GREN SYMPOSIUM SERIES Engaged Anthropology: Diversity and Dilemmas. Setha M. Low and October 2015 Sally Engle Merry, eds. POLITICS OF THE URBAN POOR: AESTHETICS, Corporate Lives: New Perspectives on the Social Life of the Corporate Form. Damani Partridge, Marina Welker, and Rebecca Hardin, eds. ETHICS, VOLATILITY, PRECARITY The Origins of Agriculture: New Data, New Ideas. T. Douglas Price and GUEST EDITORS: VEENA DAS AND SHALINI RANDERIA Ofer Bar-Yosef, eds. The Biological Anthropology of Living Human Populations: World Histories, Politics of the Urban Poor: Aesthetics, Ethics, Volatility, Precarity National Styles, and International Networks. Susan Lindee and 56 Volume The Urban Poor and Their Ambivalent Exceptionalities: Notes from Jakarta Ricardo Ventura Santos, eds. The Politics of Not Studying the Poorest of the Poor in Urban South Africa Human Biology and the Origins of Homo. Susan Antón and Leslie C. Plebeians of the Arab Spring Aiello, eds. Political Leadership and the Urban Poor: Local Histories Potentiality and Humanness: Revisiting the Anthropological Object in The Need for Patience: The Politics of Housing Emergency in Buenos Aires Contemporary Biomedicine. Klaus Hoeyer and Karen-Sue Taussig, eds. The Politics of the Urban Poor in Postwar Colombo Supplement 11 Alternative Pathways to Complexity: Evolutionary Trajectories in the Middle Sectarianism and the Ambiguities of Welfare in Lebanon Paleolithic and Middle Stone Age. -

Three Approaches to the Study of Health, Disease and Illness; the Strengths and Weaknesses of Each, with Special Reference to Refugee Populations
Anne Sigfrid Grønseth Three approaches to the study of health, disease and illness; the strengths and weaknesses of each, with special reference to refugee populations NAKMIs skriftserie om minoriteter og helse 2/2009 Redaktør Karin Harsløf Hjelde Anne Sigfrid Grønseth Three approaches to the study of health, disease and illness; the strengths and weaknesses of each, with special reference to refugee populations NAKMIs skriftserie om minoriteter og helse 2/2009 Redaktør Karin Harsløf Hjelde © NAKMI – Nasjonal kompetanseenhet for minoritetshelse 2009 NAKMIs skriftserie for minoriteter og helse Serieredaktør: Karin Harsløf Hjelde ISSN 1503-1659 ISBN 978-82-92564-06-6 Design og produksjon: 07 Gruppen AS Alle henvendelser om rapporten kan rettes til: NAKMI Oslo Universitetssykehus, HF, avd. Ullevål Bygg 37 0407 Oslo Tlf.: 23 01 60 60 Faks: 23 01 60 61 [email protected] www.nakmi.no Three approaches to the study of health, disease and illness; the strengths and weaknesses of each, with special reference to refugee populations. Thesis Defence Lecture, Dr. Polit, NTNU 15 December 2006 Anne Sigfrid Grønseth Introduction In this lecture I start by establishing a thematic and conceptual context in which to under- stand health, illness and disease, as well as refugee populations. Then I turn to three approaches that highlight distinct and interrelated aspects in the exploration and under- standing of illness and health. Each of these approaches will be evaluated in terms of its strengths and weaknesses with special reference to refugee populations. Introducing the different perspectives, I provide a general description supported by references to well known studies. Further, I have selected one recent case study for each, on which I elaborate more extensively. -

Gender and Sexuality
PERSPECTIVES: AN OPEN INTRODUCTION TO CULTURAL ANTHROPOLOGY SECOND EDITION Nina Brown, Thomas McIlwraith, Laura Tubelle de González 2020 American Anthropological Association 2300 Clarendon Blvd, Suite 1301 Arlington, VA 22201 ISBN Print: 978-1-931303-67-5 ISBN Digital: 978-1-931303-66-8 http://perspectives.americananthro.org/ This book is a project of the Society for Anthropology in Community Colleges (SACC) http://sacc.americananthro.org/ and our parent organization, the American Anthropological Association (AAA). Please refer to the website for a complete table of contents and more information about the book. Perspectives: An Open Introduction to Cultural Anthropology, 2nd Edition by Nina Brown, Thomas McIlwraith, Laura Tubelle de González is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, except where otherwise noted. Under this CC BY-NC 4.0 copyright license you are free to: Share — copy and redistribute the material in any medium or format Adapt — remix, transform, and build upon the material Under the following terms: Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. NonCommercial — You may not use the material for commercial purposes. 1010 GENDER AND SEXUALITY Carol C. Mukhopadhyay, San Jose State University [email protected] http://www.sjsu.edu/people/carol.mukhopadhyay Tami Blumenfield, Yunnan University [email protected] with Susan Harper, Texas Woman’s University, [email protected], and Abby Gondek, [email protected] Learning Objectives • Identify ways in which culture shapes sex/gender and sexuality. -

Citizens and Anthropologists 59 CITIZENS AND
Citizens and Anthropologists 59 CITIZENS AND ANTHROPOLOGISTS Myriam Jimeno Introduction In this paper I propose to outline some of the debates and positions that have shaped anthropology in Colombia since it was established as a disciplinary and professional field in the mid 1940s. Although archeology, linguistics or biological anthropology might also be interesting perspectives from which to approach this subject, my intention here is to focus on socio-cultural anthropology. I will argue that the evolution of anthropology can be understood in terms of the tension between the global orientations of the discipline (concerning dominant narratives and practices, theories, field work, relations between subjects of study) and the way they are put into practice within the Colombian context. In countries such as Colombia, anthropological practice is permanently faced with the uneasy choice between adopting dominant anthropological concepts and orientations, or modifying them, adapting them, rejecting them and proposing alternatives. This need to adapt the practice stems from the specific social condition of anthropologists in these countries; that is, our dual position as both researchers and fellow citizens of our subjects of study, as a result of which we are continually torn between our duty as scientists and our role as citizens. From this perspective, there is a danger of falling into a nationalistic interpretation of the history of anthropology in Colombia. As Claudio Lomnitz (1999) ironically comments, such is the case of Mexican anthropology, -

Curriculum Vitae
CURRICULUM VITAE Arthur Kleinman Personal Born: March 11, 1941, New York, New York Married: Joan Andrea Kleinman (d. March 6 2011) Children: Peter and Anne Grandchildren: Gabriel, Kendall, Allegra, Clayton Arthur Office Address: 21 Divinity Avenue, Room 414 Tozzer Anthropology Building Cambridge, MA 02138 Office Telephone: 617-496-8336 E-Mail: [email protected] Education 1962 A.B. with highest honors Stanford University 1967 M.D. Stanford University 1974 M.A. in Social Anthropology Harvard University Honorary Degrees 1996 Doctorate of Science, York University (Canada), Honoris Causa Postgraduate Training 1967-1968 Medical Intern, Yale-New Haven Hospital, New Haven 1968-1970 Research Fellow, Geographic Medicine Branch, National Institute of Allergy and Infectious Diseases, National Institutes of Heath 1969-1970 Research Fellow, U.S. Naval Medical Research Unit #2, Taipei, Taiwan 1970-1972 Research Fellow in the Comparative Study of Medicine, Department of History of Science, Harvard University 1972-1975 Resident, Department of Psychiatry, Harvard Medical School, Massachusetts General Hospital 1974-1976 Foundations Fund Research in Psychiatry, Postdoctoral Fellow, Massachusetts General Hospital, Harvard Medical School Faculty Positions (Present) 2011- Harvard College Professor, Harvard University 2008-2016 Victor and William Fung Director, Harvard University Asia Center 2004-2007 Chair, Department of Anthropology, Harvard University 2002- Esther and Sidney Rabb Professor of Anthropology, Department of Anthropology, Faculty of Arts -

Lancet and University College London Commission on Culture and Health
1 Lancet and University College London Commission on Culture and Health A. David Napier, Clyde Arcano, Beverly Butler, Joseph Calabrese, Angel Chater, Helen Chatterjee, François Guesnet, Robert Horne, Stephen Jacyna, Sushrut Jadhav, Alison Macdonald, Ulrike Neuendorf, Aaron Parkhurst, Rodney Reynolds, Graham Scambler, Sonu Shamdasani, Sonia Smith, Jakob Stougaard-Nielsen, Nick Tyler, Anna-Maria Volkmann, Trinley Walker, Jessica Watson, Amanda C de C Williams, Chris Willott, James Wilson, Katherine Woolf. Claim: The systematic neglect of culture in health is the single biggest barrier to advancing the highest attainable standard of health worldwide. Advisory Board: Cyril Chantler, Veena Das, Didier Fassin, Hansjoerg Dilger, Sahra Gibbon, Mary-Jo DelVecchio Good, Byron Good, Nora Groce, Richard Grinker, Anita Hardon, Angela Hobart, Roland Littlewood, Lenore Manderson, Martin Marshall, Emily Martin, Jonathan Montgomery, David Nugent, Stanley Okolo, David Pencheon, Ivo Quaranta, James Roberts, Cynthia Rosenberg, Sylvie Schuster, James Scott, Paul Stoller, Alan Thompson, Miriam Ticktin, Bencie Woll. 2 Summary Perceptions of physical and psychological wellbeing vary dramatically across and within systems of value, as do individual experiences within diverse contexts and patterns of practice. Today, global forces, planned and unplanned migrations, and emerging disease vectors create new forms of experience that continuously transform how health and wellbeing are understood and negotiated. At the same time, familiar illnesses - both communicable and non-communicable - persist and impact on individual health and household, community, and state economies. Such forces shape medical knowledge and shape how medical knowledge is understood, how it comes to be valued, and how and when it is adopted. Cultural systems of value are dynamic and always changing. -

Culture and Personality Syllabus Fall 2018 1
Culture and Personality Syllabus Fall 2018 1 Culture and Personality Anthropology 21: 070: 305: 90 Fall 2018 Dr. Carol E. Henderson Dept. of Sociology and Anthropology Rutgers University-Newark [email protected] Phone: 973-353-5255 Manganiyar men of Rajasthan, with children (photo by C. Henderson). What makes us tick? Are women and men the same the world over? Why do some peoples seem warlike, while others seem peaceful? How do different cultures define mental and emotional health and wellness? How do the biological substrates of cognition and emotion, along with our life experiences, interact with how diverse cultures model and pattern personality? Course Description This course familiarizes us with how anthropologists have studied the psychological dimensions of the human experience. We explore case studies about emotion and thought in diverse cultural settings, and how people in different cultures experience selfhood as individuals and as members of collective groups. We study the interface between biology, emotion, cognition and culture. Our course subject matter features: Core questions, approaches, and methods of psychological anthropology Significant contributions of psychological anthropology to the understanding of human diversity New trends and the relationship of psychological anthropology to the emerging neuroscience paradigm. This course syllabus describes our course policies, the program of work, and important information about this course. Be sure to download and print out a copy of this course syllabus. Course