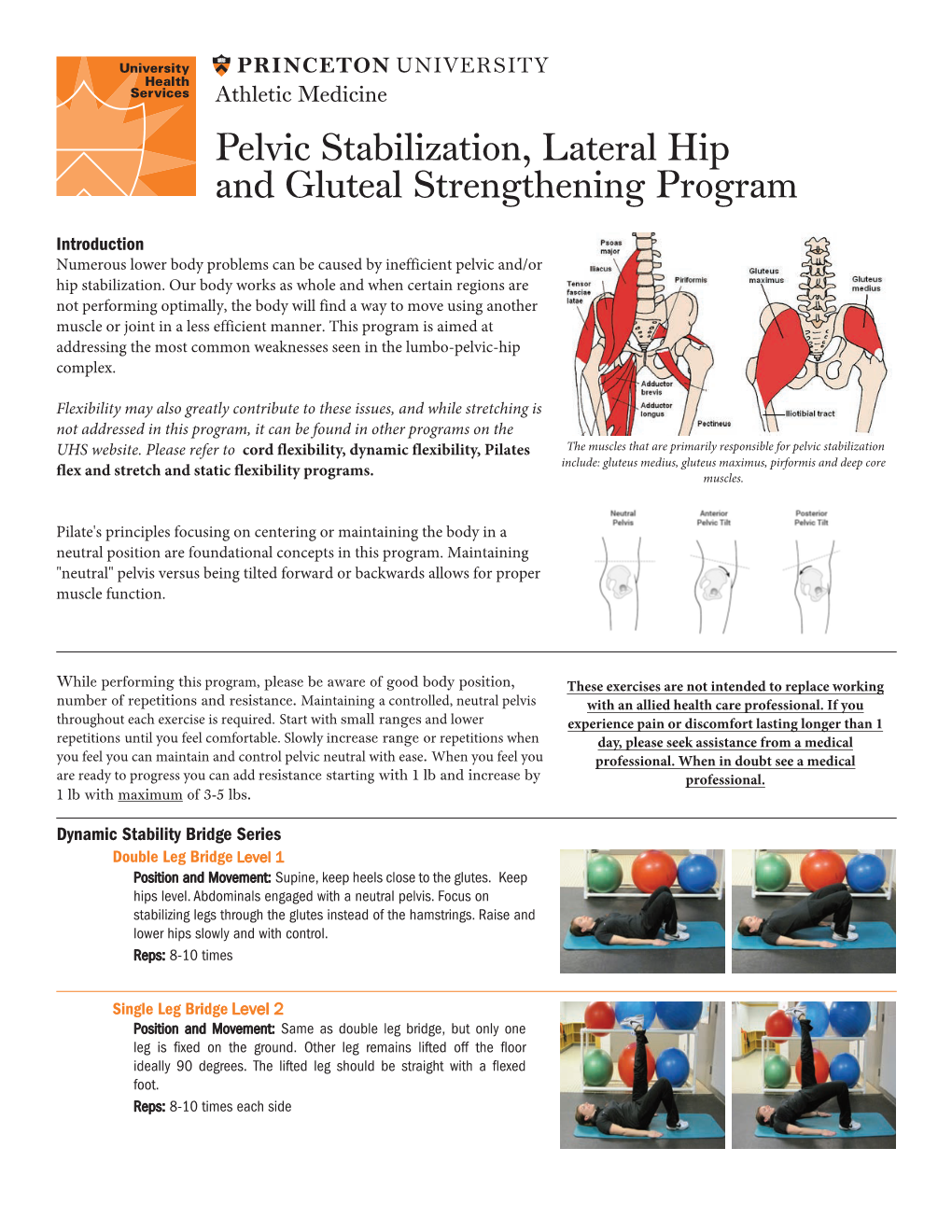
Pelvic Stabilization, Lateral Hip and Gluteal Strengthening Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Knee Flow Chart Acute
Symptom chart for acute knee pain START HERE Did the knee pain begin Does the knee joint You may have a fracture or Stop what you are doing immediately and go to a hospital emergency room YES YES suddenly, with an injury, appear deformed, or dislocated patella. or an orthopedic surgeon specializing in knee problems. slip, fall, or collision? out of position? If possible, splint the leg to limit the movement of the knee until you reach NO the doctor. Do not put any weight on the knee. Use a wheelchair, a cane, or NO crutch to prevent putting any weight on the leg, which might cause further damage to the joint. GO TO FLOW CHART #2 Go to an orthopedic surgeon Stop what you are doing. Continuing activity despite the feeling that the knee ON CHRONIC KNEE Did you hear a “pop” YES immediately, you may have is unstable can cause additional damage to other ligaments, meniscus , and PROBLEMS THAT DEVELOP and does your knee feel torn your anterior cruciate, or cartilage. Try ice on the knee to control swelling. Take anti-in ammatories OR WORSEN OVER TIME. unstable or wobbly? other ligaments in the knee. like Advil or Nuprin until your doctor’s appointment. About a third of ligament tears get better with exercises, a third may need a brace, and a third may need sur gery. NO Use R•I•C•E for sore knees Does your knee hurt YES You may have damaged the articular Try anti-in ammatories, as directed on the bottle, for two days to reduce R: Rest as you bend it? cartilage on the bottom of the the chronic in ammation. -

Total HIP Replacement Exercise Program 1. Ankle Pumps 2. Quad
3 sets of 10 reps (30 ea) 2 times a day Total HIP Replacement Exercise Program 5. Heel slides 1. Ankle Pumps Bend knee and pull heel toward buttocks. DO NOT GO Gently point toes up towards your nose and down PAST 90* HIP FLEXION towards the surface. Do both ankles at the same time or alternating feet. Perform slowly. 2. Quad Sets Slowly tighten thigh muscles of legs, pushing knees down into the surface. Hold for 10 count. 6. Short Arc Quads Place a large can or rolled towel (about 8”diameter) under the leg. Straighten knee and leg. Hold straight for 5 count. 3. Gluteal Sets Squeeze the buttocks together as tightly as possible. Hold for a 10 count. 7. Knee extension - Long Arc Quads Slowly straighten operated leg and try to hold it for 5 sec. Bend knee, taking foot under the chair. 4. Abduction and Adduction Slide leg out to the side. Keep kneecap pointing toward ceiling. Gently bring leg back to pillow. May do both legs at the same time. Copywriter VHI Corp 3 sets of 10 reps (30 ea) 2 times a day Total HIP Replacement Exercise Program 8. Standing Stair/Step Training: Heel/Toe Raises: 1. The “good” (non-operated) leg goes Holding on to an immovable surface. UP first. Rise up on toes slowly 2. The “bad” (operated) leg goes for a 5 count. Come back to foot flat and lift DOWN first. toes from floor. 3. The cane stays on the level of the operated leg. Resting positions: To Stretch your hip to neutral position: 1. -

Human Functional Anatomy 213 the Ankle and Foot In
2 HUMAN FUNCTIONAL ANATOMY 213 JOINTS OF THE FOOT THE ANKLE AND FOOT IN LOCOMOTION THE HINDFOOT -(JOINTS OF THE TALUS) THIS WEEKS LAB: Forearm and hand TROCHLEAR The ankle, and distal tibiofibular joints READINGS BODY The leg and sole of foot Subtalar joint (Posterior talocalcaneal) 1. Stern – Core concepts – sections 99, 100 and 101 (plus appendices) HEAD 2. Faiz and Moffat – Anatomy at a Glance – Sections 50 and 51 Talocalcaneonavicular 3. Grants Method:- The bones and sole of foot & Joints of the lower limb & Transverse tarsal joints or any other regional textbook - similar sections IN THIS LECTURE I WILL COVER: Joints related to the talus Ankle Subtalar Talocalcaneonavicular THE MID FOOT Transverse tarsal Other tarsal joints THE FOREFOOT Toe joints METATARSAL AND PHALANGEAL Ligaments of the foot JOINTS (same as in the hand) Arches of the foot Except 1st metatarsal and Hallux Movements of the foot & Compartments of the leg No saddle joint at base is 1st metatarsal The ankle in Locomotion Metatarsal head is bound by deep Ankle limps transverse metatarsal ligament 1. Flexor limp Toes are like fingers 2. Extensor limp Same joints, Lumbricals, Interossei, Extensor expansion Axis of foot (for abduction-adduction) is the 2nd toe. 3 4 JOINTS OF THE FOOT JOINTS OF THE FOOT (2 joints that allow inversion and eversion) DISTAL TIBIOFIBULAR SUBTALAR (Posterior talocalcaneal) JOINT Syndesmosis (fibrous joint like interosseous membrane) Two (or three) talocalcaneal joints Posterior is subtalar Fibres arranged to allow a little movement Anterior (and middle) is part of the talocalcaneonavicular. With a strong interosseus ligament running between them (tarsal sinus) THE TALOCALCANEONAVICULAR JOINT The head of the talus fits into a socket formed from the: The anterior talocalcaneal facets. -
Arthroscopic and Open Anatomy of the Hip 11
CHAPTER Arthroscopic and o'pen Anatomy of the Hip Michael B. Gerhardt, Kartik Logishetty, Morteza lV1eftah, and Anil S. Ranawat INTRODUCTION movements that they induce at the joint: 1) flexors; 2) extensors; 3) abductors; 4) adductors; 5) external rotators; and 6) interI12 I The hip joint is defined by the articulation between the head rotators. Although some muscles have dual roles, their primary of the femur and the aeetahulum of the pelvis. It is covered by functions define their group placem(:)nt, and they all have ullique :l large soft-tissue envelope and a complex array of neurovascu- neurovascular supplies (TIt ble 2-1). lar and musculotendinous structures. The joint's morphology The vascular supply of tbe hip stems from the external and anu orientation are complex, and there are wide anatomi c varia- internal iLiac ancries. An understanding of the course of these tions seen among individuals. The joint's deep location makes vessels is critical fo r ,lVo iding catasu"ophic vascular injury. fn both arthroscopic and open access challenging. To avoid iatro- addition, the blood supply to the fel11()ra l head is vulnerahle to genic injury while establishing functional and efficient access, both traumatic and iatrogenic injury; the disruption of this sup- the hip surgeon should possess a sound ana tomic knowledge of ply can result in avascular necrosis (Figure 2-2). the hip. T he human "hip" can be subdivided into three categories: I) the superficial surface anatomy; 2) the deep femoroacetabu- la r Joint and capsule; and 3) the associated structures, including the muscles, nerves, and vasculature, all of which directly affeet HIP MUSCULATURE its function. -

Hip Extensor Mechanics and the Evolution of Walking and Climbing Capabilities in Humans, Apes, and Fossil Hominins
Hip extensor mechanics and the evolution of walking and climbing capabilities in humans, apes, and fossil hominins Elaine E. Kozmaa,b,1, Nicole M. Webba,b,c, William E. H. Harcourt-Smitha,b,c,d, David A. Raichlene, Kristiaan D’Aoûtf,g, Mary H. Brownh, Emma M. Finestonea,b, Stephen R. Rossh, Peter Aertsg, and Herman Pontzera,b,i,j,1 aGraduate Center, City University of New York, New York, NY 10016; bNew York Consortium in Evolutionary Primatology, New York, NY 10024; cDepartment of Anthropology, Lehman College, New York, NY 10468; dDivision of Paleontology, American Museum of Natural History, New York, NY 10024; eSchool of Anthropology, University of Arizona, Tucson, AZ 85721; fInstitute of Ageing and Chronic Disease, University of Liverpool, Liverpool L7 8TX, United Kingdom; gDepartment of Biology, University of Antwerp, 2610 Antwerp, Belgium; hLester E. Fisher Center for the Study and Conservation of Apes, Lincoln Park Zoo, Chicago, IL 60614; iDepartment of Anthropology, Hunter College, New York, NY 10065; and jDepartment of Evolutionary Anthropology, Duke University, Durham, NC 27708 Edited by Carol V. Ward, University of Missouri-Columbia, Columbia, MO, and accepted by Editorial Board Member C. O. Lovejoy March 1, 2018 (received for review September 10, 2017) The evolutionary emergence of humans’ remarkably economical their effects on climbing performance or tested whether these walking gait remains a focus of research and debate, but experi- traits constrain walking and running performance. mentally validated approaches linking locomotor -

Iliopsoas Tendonitis/Bursitis Exercises
ILIOPSOAS TENDONITIS / BURSITIS What is the Iliopsoas and Bursa? The iliopsoas is a muscle that runs from your lower back through the pelvis to attach to a small bump (the lesser trochanter) on the top portion of the thighbone near your groin. This muscle has the important job of helping to bend the hip—it helps you to lift your leg when going up and down stairs or to start getting out of a car. A fluid-filled sac (bursa) helps to protect and allow the tendon to glide during these movements. The iliopsoas tendon can become inflamed or overworked during repetitive activities. The tendon can also become irritated after hip replacement surgery. Signs and Symptoms Iliopsoas issues may feel like “a pulled groin muscle”. The main symptom is usually a catch during certain movements such as when trying to put on socks or rising from a seated position. You may find yourself leading with your other leg when going up the stairs to avoid lifting the painful leg. The pain may extend from the groin to the inside of the thigh area. Snapping or clicking within the front of the hip can also be experienced. Do not worry this is not your hip trying to pop out of socket but it is usually the iliopsoas tendon rubbing over the hip joint or pelvis. Treatment Conservative treatment in the form of stretching and strengthening usually helps with the majority of patients with iliopsoas bursitis. This issue is the result of soft tissue inflammation, therefore rest, ice, anti- inflammatory medications, physical therapy exercises, and/or injections are effective treatment options. -

Tibialis Posterior Tendon Transfer Corrects the Foot Drop Component
456 COPYRIGHT Ó 2014 BY THE JOURNAL OF BONE AND JOINT SURGERY,INCORPORATED Tibialis Posterior Tendon Transfer Corrects the Foot DropComponentofCavovarusFootDeformity in Charcot-Marie-Tooth Disease T. Dreher, MD, S.I. Wolf, PhD, D. Heitzmann, MSc, C. Fremd, M.C. Klotz, MD, and W. Wenz, MD Investigation performed at the Division for Paediatric Orthopaedics and Foot Surgery, Department for Orthopaedic and Trauma Surgery, Heidelberg University Clinics, Heidelberg, Germany Background: The foot drop component of cavovarus foot deformity in patients with Charcot-Marie-Tooth disease is commonly treated by tendon transfer to provide substitute foot dorsiflexion or by tenodesis to prevent the foot from dropping. Our goals were to use three-dimensional foot analysis to evaluate the outcome of tibialis posterior tendon transfer to the dorsum of the foot and to investigate whether the transfer works as an active substitution or as a tenodesis. Methods: We prospectively studied fourteen patients with Charcot-Marie-Tooth disease and cavovarus foot deformity in whom twenty-three feet were treated with tibialis posterior tendon transfer to correct the foot drop component as part of a foot deformity correction procedure. Five patients underwent unilateral treatment and nine underwent bilateral treatment; only one foot was analyzed in each of the latter patients. Standardized clinical examinations and three-dimensional gait analysis with a special foot model (Heidelberg Foot Measurement Method) were performed before and at a mean of 28.8 months after surgery. Results: The three-dimensional gait analysis revealed significant increases in tibiotalar and foot-tibia dorsiflexion during the swing phase after surgery. These increases were accompanied by a significant reduction in maximum plantar flexion at the stance-swing transition but without a reduction in active range of motion. -

Plantar Fascia-Specific Stretching Program for Plantar Fasciitis
Plantar Fascia-Specific Stretching Program For Plantar Fasciitis Plantar Fascia Stretching Exercise 1. Cross your affected leg over your other leg. 2. Using the hand on your affected side, take hold of your affected foot and pull your toes back towards shin. This creates tension/stretch in the arch of the foot/plantar fascia. 3. Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string. 4. Hold the stretch for a count of 10. A set is 10 repetitions. 5. Perform at least 3 sets of stretches per day. You cannot perform the stretch too often. The most important times to stretch are before taking the first step in the morning and before standing after a period of prolonged sitting. Plantar Fascia Stretching Exercise 1 2 3 4 URMC Orthopaedics º 4901 Lac de Ville Boulevard º Building D º Rochester, NY 14618 º 585-275-5321 www.ortho.urmc.edu Over, Please Anti-inflammatory Medicine Anti-inflammatory medicine will help decrease the inflammation in the arch and heel of your foot. These include: Advil®, Motrin®, Ibuprofen, and Aleve®. 1. Use the medication as directed on the package. If you tolerate it well, take it daily for 2 weeks then discontinue for 1 week. If symptoms worsen or return, then resume medicine for 2 weeks, then stop. 2. You should eat when taking these medications, as they can be hard on your stomach. Arch Support 1. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Metatarsalgia
just the symptoms. What can I expect from treatment? With a proper diagnosis, and a well-rounded treatment plan including orthotics, the prog- nosis is excellent. With Sole Supports™ foot or- thotics you can expect either a dramatic loss The Truth About . of pain within the first weeks of use or a more gradual reduction of symptoms, depending Metatarsalgia on how long the problem has existed, normal body weight or how well you follow other ther- For more information and a apeutic regimens prescribed by your provider. professional consultation regarding Did you know that, with Sole whether Sole Supports may be Supports, metatarsal pads are rarely helpful for you, please contact the needed? following certified Sole Supports practitioner: What is it? Metatarsalgia is a term used to describe a pain- ful foot condition in the area just before the Arch Flattened small toes (more commonly referred to as the ball of the foot). The condition is characterized by pain and inflammation on the sole in the region of the metatarsal heads, which are the ends of the long bones in your foot. The joint This handout provides a general overview on this capsule or tendons may also be inflamed. topic and may not apply to everyone. To find out if this handout applies to you and to get more infor- mation on this subject, consult with your certified Sole Supports practitioner. Arch Restored The pain is generally aggravated by putting ments but your doctor is likely to recommend pressure off the metatarsals should also be pressure (as in walking) through the ball of a conservative approach first including: followed. -

Piriformis Syndrome: the Literal “Pain in My Butt” Chelsea Smith, PTA
Piriformis Syndrome: the literal “pain in my butt” Chelsea Smith, PTA Aside from the monotony of day-to-day pains and annoyances, piriformis syndrome is the literal “pain in my butt” that may not go away with sending the kids to grandmas and often takes the form of sciatica. Many individuals with pain in the buttock that radiates down the leg are experiencing a form of sciatica caused by irritation of the spinal nerves in or near the lumbar spine (1). Other times though, the nerve irritation is not in the spine but further down the leg due to a pesky muscle called the piriformis, hence “piriformis syndrome”. The piriformis muscle is a flat, pyramidal-shaped muscle that originates from the front surface of the sacrum and the joint capsule of the sacroiliac joint (SI joint) and is located deep in the gluteal tissue (2). The piriformis travels through the greater sciatic foramen and attaches to the upper surface of the greater trochanter (or top of the hip bone) while the sciatic nerve runs under (and sometimes through) the piriformis muscle as it exits the pelvis. Due to this close proximity between the piriformis muscle and the sciatic nerve, if there is excessive tension (tightness), spasm, or inflammation of the piriformis muscle this can cause irritation to the sciatic nerve leading to symptoms of sciatica (pain down the leg) (1). Activities like sitting on hard surfaces, crouching down, walking or running for long distances, and climbing stairs can all increase symptoms (2) with the most common symptom being tenderness along the piriformis muscle (deep in the gluteal region) upon palpation. -

Systematic Approach to the Interpretation of Pelvis and Hip
Volume 37 • Number 26 December 31, 2014 Systematic Approach to the Interpretation of Pelvis and Hip Radiographs: How to Avoid Common Diagnostic Errors Through a Checklist Approach MAJ Matthew Minor, MD, and COL (Ret) Liem T. Bui-Mansfi eld, MD After participating in this activity, the diagnostic radiologist will be better able to identify the anatomical landmarks of the pelvis and hip on radiography, and become familiar with a systematic approach to the radiographic interpretation of the hip and pelvis using a checklist approach. initial imaging examination for the evaluation of hip or CME Category: General Radiology Subcategory: Musculoskeletal pelvic pain should be radiography. In addition to the com- Modality: Radiography plex anatomy of the pelvis and hip, subtle imaging fi ndings often indicating signifi cant pathology can be challenging to the veteran radiologist and even more perplexing to the Key Words: Pelvis and Hip Anatomy, Radiographic Checklist novice radiologist given the paradigm shift in radiology residency education. Radiography of the pelvis and hip is a commonly ordered examination in daily clinical practice. Therefore, it is impor- tant for diagnostic radiologists to be profi cient with its inter- The initial imaging examination for the evaluation pretation. The objective of this article is to present a simple of hip or pelvic pain should be radiography. but thorough method for accurate radiographic evaluation of the pelvis and hip. With the advent of cross-sectional imaging, a shift in residency training from radiography to CT and MR imag- Systematic Approach to the Interpretation of Pelvis ing has occurred; and as a result, the art of radiographic and Hip Radiographs interpretation has suffered dramatically.