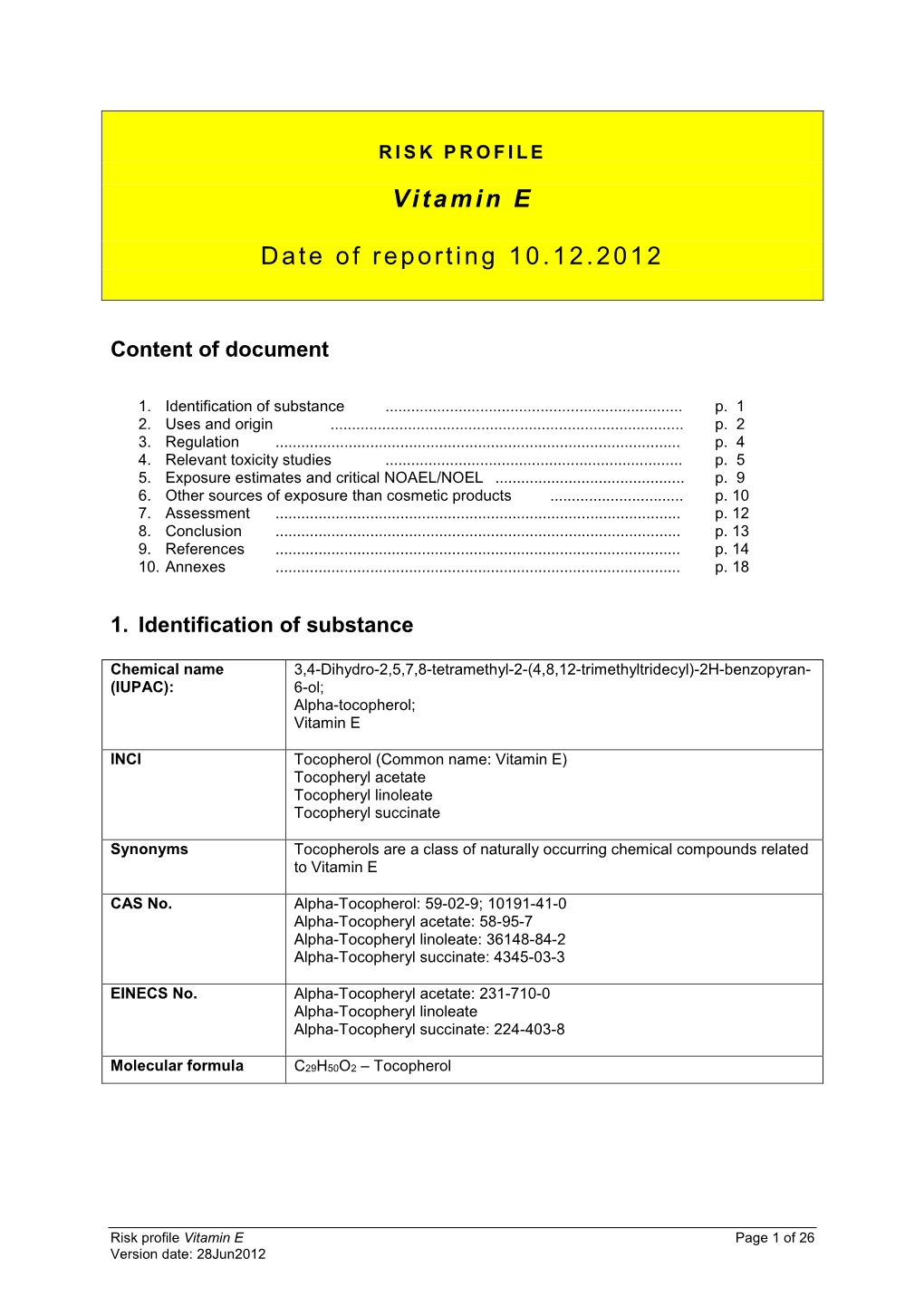
RISK PROFILE of Vitamin E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dispensing of Vitamin Products by Retail Pharmacies in South Africa: Implications for Dietitians
South African Journal of Clinical Nutrition 2016; 29(4):133–138 http://dx.doi.org/10.1080/16070658.2016.1219468 SAJCN ISSN 1607-0658 EISSN 2221-1268 Open Access article distributed under the terms of the © 2016 The Author(s) Creative Commons License [CC BY-NC 3.0] http://creativecommons.org/licenses/by-nc/3.0 RESEARCH Dispensing of vitamin products by retail pharmacies in South Africa: Implications for dietitians Ilse Trutera* and Liana Steenkampb a Department of Pharmacy, Drug Utilisation Research Unit (DURU), Nelson Mandela Metropolitan University, Port Elizabeth, South Africa b HIV & AIDS Research Unit, Nelson Mandela Metropolitan University, Port Elizabeth, South Africa *Corresponding author, email: [email protected] Objective: The objective of this study was to analyse the dispensing patterns of vitamins (Anatomical Therapeutic Chemical (ATC) group A11) over a one-year period in a group of community pharmacies in South Africa. Design and setting: A retrospective drug utilisation study was conducted on community pharmacy electronic dispensing records in South Africa recorded in 2013. Outcome measures: All products for ATC subgroup A11 were extracted and analysed. Results: A total of 164 233 vitamin products were dispensed to 84 805 patients (62.64% female patients). Males received on average 2.09 (SD = 2.63) vitamin products per year, compared to 1.84 (SD = 2.13) products for females. Ergocalciferol (A11CC01) was the most often dispensed (37.48% of all vitamin products), followed by plain Vitamin B-complex products (A11EA00) accounting for 32.77%. Ergocalciferol (vitamin D2) is only available on prescription (50 000 IU tablets or 50 000 IU/ml oily drops) in South Africa. -

Dry Vitamin E- Acetate 50% DC/GFP
Dry Vitamin E-Acetate 50% DC Chemical names of active ingredient DL--tocopheryl acetate, DL-alpha-tocopherol acetate, all-rac-alpha- tocopherol acetic acid ester, racemic 5,7,8-trim- ethyltocol acetate CAS-No. 52225-20-4 C31H52O3 Molar mass 472.8 g/mol EINECS-No. 231-710-0 Monographs PRD-No. The product complies with the current “-tocopheryl 30041051 acetate concentrate (powder form)” Ph. Eur. and “Vitamin E preparation” USP monographs. Article Regulations 50051053 25 kg bag in box The product meets the regulatory requirements for a vitamin E source in most countries. How- Country of origin ever, regulations on the ingredients used in the Denmark respective countries and for the intended use have to be observed. Units 1 International Unit (IU) = 1 mg vitamin E-acetate Bulk density Approx. 0.5 g/ml Description Dry, almost white, virtually odorless, free-flowing Stability powder, consisting of spherical particles. The stability of Dry Vitamin E-Acetate 50% DC is excellent even in the presence of minerals. Composition Stored in its original packaging at room tem- Ingredients in descending order of weight: perature (max. 25 °C), the product is stable for DL-alpha-tocopheryl acetate, corn starch, gelatin, at least 36 months. sucrose, sodium aluminum silicate. Storage/Handling Solubility The product should be stored in the original Dispersible in warm water (35 – 40 °C), to form a packaging in a dry place at room temperature milky emulsion. Insoluble particles may be visible. (max. 25 °C). Specification Assay min. 50% DL--tocopheryl acetate (= 500 former IU of vitamin E = 336 -TE per gram) For further information see separate document: “Standard Specification” (not for regulatory purposes) available via BASF’s WorldAccount: https://worldaccount.basf.com (registered access). -

Report on Effects of Beta-Carotene Supplementation in Combination with Tocopherol and Ascorbate in Clinical and Chemopreventive Trials (Adopted by the SCF on 19/3/98)
Report on Effects of Beta-carotene Supplementation in Combination with Tocopherol and Ascorbate in Clinical and Chemopreventive Trials (Adopted by the SCF on 19/3/98) Terms of Reference The committee was asked by the Commission to review on recent reports of the studies on health effects of high doses of beta-carotene, retinol and alpha-tocopherol as well as ascorbate in controlled studies. Introduction Epidemiological studies of the last ten years have indicated that beta-carotene is a potential agent for the chemical prevention against carcinogenesis. In contrast, the recent prospective study performed by Heinonen et al. (1) has strikingly suggested that supplementation with beta-carotene significantly increased the incidence of lung, prostate and stomach cancer. The rising question is the possible dose dependency of a preventive or harmful action of beta-carotene and possible synergistic effects with other antioxidants. To answer this question clinical trials for therapy and intervention studies in healthy populations dealing with beta- carotene supplementation in different dosages below the GRAS daily intake of 200 mg have to be regarded. Clinical trials Therapeutic dosages of beta-carotene applied varied in a relative wide range of 20 mg/d to 180 mg/d. The highest daily dosage of 180 mg beta-carotene in combination with 100.000 IU vitamin A ( 30 mg retinol equivalents) was applied 1988 by Stich et al. (2) in tobacco chewers who had already sustained premalignant leukoplakia. After 6 months the single treatment with beta-carotene induced a significant remission of leukoplakias compared to the placebo group, although the combination of beta-carotene and retinol was much more effective. -

Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Antioxidative Effects of A-Tocopherol and Riboflavin-Butyrate in Rats Dosed with Methyl Linoleate Hydroperoxide
Agric. Biol. Chem., 47 (7), 1577- 1582, 1983 1577 Antioxidative Effects of a-Tocopherol and Riboflavin-butyrate in Rats Dosed with Methyl Linoleate Hydroperoxide Teruo Miyazawa, Chiharu Sato and Takashi Kaneda Department of Food Chemistry, Faculty of Agriculture, Tohoku University, Sendai 980, Japan Received January 6, 1983 The antioxidative effects of dietary a-tocopherol (TOC) and riboftavin-tetrabutyrate (RTB)against tissue lipoperoxidation caused by the long-term administration of methyl linole- ate hydroperoxide (HPO) to rats were investigated by measuring the spontaneous chemilumi- nescence (CL) intensities and thiobarbituric acid (TBA) reactants of the liver, lung and heart. TOCsupplementation resulted in the effective decrease of CLintensities and TBAreac- tants in the three organs, while RTBsupplementation led to the definitive decay of both indices of the lung and a significant decrease in the CL intensity of the heart, as compared with those of rats dosed with HPOand not given any supplemental antioxidant. Although the activities of glutathione peroxidase and glutathione reductase in the three organs obtained from rats dosed with HPOfor 29 days were clearly lower than those of the control rats, both enzyme activities in rats dosed with antioxidants other than HPOwere gener- ally maintained at levels almost equal to those of the control rats. Glutathione peroxidase of the liver and heart and glutathione reductase of the liver were shownto be further activated by the simultaneous supplementation of TOCand RTB. The results indicated that both TOCand RTBeffectively act as antioxidants in rats dosed with HPOover a long-term. Oneof the antioxidative actions of both agents is ascribed to pro- tection of the glutathione peroxidase system in organs undergoing lipoperoxidation caused by the long-term treatment of dietary hydroperoxides. -

Vitamin A, E, & D Unit Change
Vitamin A, E, & D Unit Change Agenda The following provides an overview of the updated units that NQAC Dublin will be using to adhere to FDA guideline changes regarding Nutrition and Supplement Facts labels. This presentation will review: • FDA Guidelines • Methods Affected • Unit Changes by Vitamin • Conversions In August of 2019, the FDA updated its guideline requirements for Nutrition and Supplement Facts labels regarding vitamin A, vitamin D, and vitamin E. The following link can be used to access the FDA guidelines directly: www.fda.gov/regulatory-information Which methods are affected by this change? • LI-00.608 –Multi Fat • LI-03.701 –Fat Soluble Vitamin Determination in Premixes • LI-00.683- Carotene • GOP-756-1001- Total Vitamin A by Calculation (will be obsoleted) FDA Provided Unit Conversion Table: Vitamin A The previous RDI for vitamin A was expressed in International Units (IU), a measurement based on the biological activity or effect, where one IU of vitamin A activity had been defined as equal to 0.30 mcg of all-trans-retinol or 0.60 mcg of all-trans-β-carotene The new unit of measure, RAE, considers the vitamin A activity of β-carotene in supplements to be half the activity of pre-formed retinol, and the vitamin A activity of dietary β-carotene to be one- sixth of the β-carotene in supplements Furthermore, carotenoids, such as β-carotene, added to food is assumed to have the same bioconversion as those naturally occurring in foods (12:1). For the other dietary provitamin A carotenoids, β-cryptoxanthin and α-carotene, the RAE is set at 24 based on a vitamin A activity approximately half of that for β-carotene. -

Vitamins a and E and Carotenoids
Fat-Soluble Vitamins & Micronutrients: Vitamins A and E and Carotenoids Vitamins A (retinol) and E (tocopherol) and the carotenoids are fat-soluble micronutrients that are found in many foods, including some vegetables, fruits, meats, and animal products. Fish-liver oils, liver, egg yolks, butter, and cream are known for their higher content of vitamin A. Nuts and seeds are particularly rich sources of vitamin E (Thomas 2006). At least 700 carotenoids—fat-soluble red and yellow pigments—are found in nature (Britton 2004). Americans consume 40–50 of these carotenoids, primarily in fruits and vegetables (Khachik 1992), and smaller amounts in poultry products, including egg yolks, and in seafoods (Boylston 2007). Six major carotenoids are found in human serum: alpha-carotene, beta-carotene, beta-cryptoxanthin, lutein, trans-lycopene, and zeaxanthin. Major carotene sources are orange-colored fruits and vegetables such as carrots, pumpkins, and mangos. Lutein and zeaxanthin are also found in dark green leafy vegetables, where any orange coloring is overshadowed by chlorophyll. Trans-Lycopene is obtained primarily from tomato and tomato products. For information on the carotenoid content of U.S. foods, see the 1998 carotenoid database created by the U.S. Department of Agriculture and the Nutrition Coordinating Center at the University of Minnesota (http://www.nal.usda.gov/fnic/foodcomp/Data/car98/car98.html). Vitamin A, found in foods that come from animal sources, is called preformed vitamin A. Some carotenoids found in colorful fruits and vegetables are called provitamin A; they are metabolized in the body to vitamin A. Among the carotenoids, beta-carotene, a retinol dimer, has the most significant provitamin A activity. -

Niacin (Nicotinic Acid) in Non-Physiological Doses Causes Hyperhomocysteineaemia in Sprague–Dawley Rats
Downloaded from British Journal of Nutrition (2002), 87, 115–119 DOI: 10.1079/BJN2001486 q The Authors 2002 https://www.cambridge.org/core Niacin (nicotinic acid) in non-physiological doses causes hyperhomocysteineaemia in Sprague–Dawley rats Tapan K. Basu*, Neelam Makhani and Gary Sedgwick . IP address: Department of Agricultural, Food and Nutritional Science, University of Alberta, Edmonton, Alberta, T6G 2P5 Canada (Received 22 September 2000 – Revised 17 July 2001 – Accepted 6 August 2001) 170.106.35.93 Niacin (nicotinic acid) in its non-physiological dose level is known to be an effective lipid- , on lowering agent; its potential risk as a therapeutic agent, however, has not been critically 27 Sep 2021 at 22:43:08 considered. Since niacin is excreted predominantly as methylated pyridones, requiring methionine as a methyl donor, the present study was undertaken to examine whether metabolism of the amino acid is altered in the presence of large doses of niacin. Male Sprague–Dawley rats were given a nutritionally adequate, semi-synthetic diet containing niacin at a level of either 400 or 1000 mg/kg diet (compared to 30 mg/kg in the control diet) for up to 3 months. Supplementation with niacin (1000 mg/kg diet) for 3 months resulted in a significant increase in plasma and urinary total homocysteine levels; this increase was further accentuated in the , subject to the Cambridge Core terms of use, available at presence of a high methionine diet. The hyperhomocysteineaemia was accompanied by a significant decrease in plasma concentrations of vitamins B6 and B12, which are cofactors for the metabolism of homocysteine. -

Nutrition and Supplement Facts Labels Changes
NUTRITION AND SUPPLEMENT FACTS LABELS CHANGES The compliance date for these regulations is January 1, 2020 except for businesses with less that $10 million in food sales. These companies have until January 1, 2021. These changes will affect several aspects of current labeling practices and serving sizes. You may have questions concerning these new regulations and what these changes mean to the industry, your company and current practices. Eurofins Food Integrity and Innovation is here to help you answer your questions and, as always, serve as an insightful and resourceful partner to you during this change. General Overview 1. How are daily values changing? The majority of daily values (based on RDI and DRV) are being updated to match recommendations from the National Academy of Science (Institute of Medicine). Changes are listed here for adults and children 4 years of age and older, based on a 2000-calorie diet, as applicable. There are also changes to the daily values for infants, children 1 to 3 and pregnant and lactating women. The components that have a new unit of measure are in bold below: Component Expiring Daily Value New Daily Value Component Expiring Daily Value New Daily Value Fat 65 g 78 g Folate 400 mcg 400 mcg DFE Total Carbohydrate 300 g 275 g Vitamin B12 6 mcg 2.4 mcg Sodium 2400 mg 2300 mg Biotin 300 mcg 30 mcg Dietary Fiber 25 g 28 g Pantothenic acid 10 mg 5 mg Added Sugar 50 g Phosphorous 1000 mg 1250 mg Vitamin A 5000 IU 900 mcg RAE Magnesium 400 mg 420 mg Vitamin C 60 mg 90 mg Zinc 15 mg 11 mg Calcium 1000 mg 1300 mg Selenium 70 mcg 55 mcg Vitamin D 400 IU 20 mcg Copper 2 mg 0.9 mg Vitamin E 30 IU 15 mg Manganese 2 mg 2.3 mg Vitamin K 80 mcg 120 mcg Chromium 120 mcg 35 mcg Thiamin 1.5 mg 1.2 mg Molybdenum 75 mcg 45 mcg Riboflavin 1.7 mg 1.3 mg Chloride 3400 mg 2300 mg Niacin 20 mg 16 mg NE Potassium 3500 mg 4700 mg Vitamin B6 2 mg 1.7 mg Choline 550 mg www.eurofinsUS.com/food NUTRITION AND SUPPLEMENT FACTS LABELS CHANGES 2. -

Adverse Effects of Antioxidative Vitamins
REVIEW PAPERS International Journal of Occupational Medicine and Environmental Health 2012;25(2):105 – 121 DOI 10.2478/S13382-012-0022-x ADVERSE EFFECTS OF ANTIOXIDATIVE VITAMINS MACIEJ RUTKOWSKI1 and KRZYSZTOF GRZEGORCZYK2 1 Medical University of Łódź, Łódź, Poland Department of Clinical Chemistry and Biochemistry 2 Wł. Biegański Memorial Regional Specialistic Hospital, Łódź, Poland Department of Endoscopy and One Day Gastroenterology Abstract High doses of synthetic antioxidative vitamins: A, E, C and β-carotene are often used on long-term basis in numerous preventive and therapeutic medical applications. Instead of expected health effects, the use of those vitamins may however lead to cases of hypervitaminosis and even to intoxication. The article points out main principles of safety which are to be observed during supplementation with antioxidative vitamins. Toxic effects resulting from erroneous administration of high doses of those substances on organs and systems of the organism are also discussed. Attention is drawn to interactions of antioxidative vitamins with concomitantly used drugs, as well as intensification of adverse effects caused by various exo- genous chemical factors. Moreover, the article presents the evaluation of supplementation with these vitamins, which was performed in large studies. Key words: Vitamins A, E and C, β-carotene, Supplementation, Side actions, Toxic effects INTRODUCTION pharmaceutical drugs, and their preparations are gener- ally sold over the counter. However, it is commonly disre- Supplementation with synthetic antioxidative vitamins: garded that the excessive intake of antioxidative vitamins A, β-carotene (provitamin A), E and C, is widely propa- may be in fact harmful. Enthusiasts of at-home vitamin gated to-day, both as an adjunct to the applied pharma- supplementation, who blindly believe in newspaper rev- cotherapy and as one of factors to provide ”health and elations and advertisements, are therefore vulnerable to beauty”. -

The Interactions Between Selenium and Iodine Deficiencies in Man And
Nutrition Research Reviews (1999), 12, 55±73 55 The interactions between selenium and iodine de®ciencies in man and animals John R. Arthur1*, Geoffrey J. Beckett2 and Julie H. Mitchell1 1Division of Micronutrient and Lipid Metabolism, Rowett Research Institute, Greenburn Road, Bucksburn, Aberdeen AB21 9SB, UK 2University Department of Clinical Biochemistry, The Royal In®rmary, Edinburgh EH3 9YW, UK Abstract Up to one billion people live in areas where they may be at risk from I de®ciency. Many of the debilitating effects of the de®ciency may be irreversible, consequently it is essential to understand the mechanisms whereby lack of I can cause disease 0 through decreased thyroxine and 3,3 ,5-triiodothyronine (T3) synthesis. Since Se has an essential role in thyroid hormone metabolism, it has the potential to play a major part in the outcome of I de®ciency. These effects of Se derive from two aspects of its biological function. First, three Se-containing deiodinases regulate the synthesis and degradation of the biologically active thyroid hormone, T3. Second, selenoperoxidases and possibly thioredoxin reductase (EC 1.6.4.5) protect the thyroid gland from H2O2 produced during the synthesis of thyroid hormones. The mechanisms whereby Se de®ciency exacerbates the hypothyroidism due to I de®ciency have been elucidated in animals. In contrast to these adverse effects, concurrent Se de®ciency may also cause changes in deiodinase activities which can protect the brain from low T3 concentrations in I de®ciency. Animals with Se and I de®ciency have changes in serum thyroid hormone concentrations that are similar to those observed in patients with I de®ciency disease. -

Vitamin E Nicotinate
antioxidants Review Vitamin E Nicotinate Kimbell R. Duncan and Yuichiro J. Suzuki * Department of Pharmacology and Physiology, Georgetown University Medical Center, 3900 Reservoir Road NW, Washington, DC 20057, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-202-687-8090; Fax: +1-202-687-8825 Academic Editor: Adrianne Bendich Received: 27 December 2016; Accepted: 7 March 2017; Published: 13 March 2017 Abstract: Vitamin E refers to a family of compounds that function as lipid-soluble antioxidants capable of preventing lipid peroxidation. Naturally occurring forms of vitamin E include tocopherols and tocotrienols. Vitamin E in dietary supplements and fortified foods is often an esterified form of α-tocopherol, the most common esters being acetate and succinate. The vitamin E esters are hydrolyzed and converted into free α-tocopherol prior to absorption in the intestinal tract. Because its functions are relevant to many chronic diseases, vitamin E has been extensively studied in respect to a variety of diseases as well as cosmetic applications. The forms of vitamin E most studied are natural α-tocopherol and the esters α-tocopheryl acetate and α-tocopheryl succinate. A small number of studies include or focus on another ester form, α-tocopheryl nicotinate, an ester of vitamin E and niacin. Some of these studies raise the possibility of differences in metabolism and in efficacy between vitamin E nicotinate and other forms of vitamin E. Recently, through metabolomics studies, we identified that α-tocopheryl nicotinate occurs endogenously in the heart and that its level is dramatically decreased in heart failure, indicating the possible biological importance of this vitamin E ester.