Hypothermia Signs, Symptoms, and Treatment
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Heat Stroke Heat Exhaustion
Environmental Injuries Co lin G. Ka ide, MD , FACEP, FAAEM, UHM Associate Professor of Emergency Medicine Board-Certified Specialist in Hyperbaric Medicine Specialist in Wound Care The Ohio State University Wexner Medical Center The Most Dangerous Drug Combination… Accidental Testosterone Hypothermia and Alcohol! The most likely victims… Photo: Ralf Roletschek 1 Definition of Blizzard Hypothermia of Subnormal T° when the body is unable to generate sufficient heat to sustain normal functions Core Temperature < 95°F 1979 (35°C) Most Important Temperatures Thermoregulation 95°F (35° C) Hyper/Goofy The body uses a Poikilothermic shell to maintain a Homeothermic core 90°F (32°C) Shivering Stops Maintains core T° w/in 1.8°F(1°C) 80°F (26. 5°C) Vfib, Coma Hypothalamus Skin 65°F (18°C) Asystole Constant T° 96.896.8-- 100.4° F 2 Thermoregulation The 2 most important factors Only 3 Causes! Shivering (10x increase) Decreased Heat Production Initiated by low skin temperature Increased Heat Loss Warming the skin can abolish Impaired Thermoregulation shivering! Peripheral vasoconstriction Sequesters heat Predisposing Predisposing Factors Factors Decreased Production Increased Loss –Endocrine problems Radiation Evaporation • Thyroid Conduction* • Adrenal Axis Convection** –Malnutrition *Depends on conducting material **Depends on wind velocity –Neuromuscular disease 3 Predisposing Systemic Responses CNS Factors T°< 90°F (34°C) Impaired Regulation Hyperactivity, excitability, recklessness CNS injury T°< 80°F (27°C) Hypothalamic injuries Loss of voluntary -

Title: Drowning and Therapeutic Hypothermia: Dead Man Walking
Title: Drowning and Therapeutic Hypothermia: Dead Man Walking Author(s): Angela Kavenaugh, D.O., Jamie Cohen, D.O., Jennifer Davis MD FAAP, Department of PICU Affiliation(s): Chris Evert Children’s Hospital, Broward Health Medical Center ABSTRACT BODY: Background: Drowning is the second leading cause of death in children and is associated with severe morbidity and mortality, most often due to hypoxic-ischemic encephalopathy. Those that survive are often left with debilitating neurological deficits. Therapeutic Hypothermia after resuscitation from ventricular fibrillation or pulseless ventricular tachycardia induced cardiac arrest is the standard of care in adults and has also been proven to have beneficial effects that persist into early childhood when utilized in neonatal birth asphyxia, but has yet to be accepted into practice for pediatrics. Objective: To present supportive evidence that Therapeutic Hypothermia improves mortality and morbidity specifically for pediatric post drowning patients. Case Report: A five year old male presented to the Emergency Department after pool submersion of unknown duration. He was found to have asphyxial cardiac arrest and received bystander CPR, which was continued by EMS for a total of 10 minutes, including 2 doses of epinephrine. CPR continued into the emergency department. Upon presentation to the ED, he was found to have fixed and dilated pupils, unresponsiveness, with a GCS of 3. Upon initial pulse check was found to have return of spontaneous circulation, with sinus tachycardia. His blood gas revealed 6.86/45/477/8/-25. He was intubated, given 2 normal saline boluses and 2 mEq/kg of Sodium Bicarbonate. The initial head CT was normal. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Resident Scholarly Work
RESIDENT SCHOLARLY WORK Process Improvement 2020-2021 CPIP Curriculum Ongoing Projects: Alexander Gavralidis, Stephanie tin, Matthew Macey, Allisa Alport, Beenish Furquan, Justin Byrne • Unnecessary laboratory draws in patients at a Community Hospital - evaluating whether inpatients at Salem Hospital staying overnight for a social reason undergo unnecessary laboratory draws Daria Ade, Mayuri Rapolu, Usman Mughal, Eva Kubrova, Barbara Lambl, Patrick Lee • Procalcitonin utilization to tailor antibiotic use at Salem Hospital- part of Antibiotic Stewardship program Sneha Lakshman, Arturo Castro, Ashley So, George Kavalam, Hassan Kazmi, Daniela Urma, Patrick Gordan • Development of a standardized ultrasound guided central venus catheter insertion curriculum Nupur Dandawate, Farideh Davoudi , Usama Talib, Patrick Lee • Inpatient Echo utilization – guidelines updates Anneris Estevez, Usmam Mughal, Zach Abbott, Evita Joseph, Caroline Cubbison, Faith Omede, Daniela Urma • Decrease health disparities for Hispanic community at Lynn NSPG by standardizing diabetes education referral patterns and patient education Imama Ahmad, Usama Talib, Muhammad Akash, Pablo Ledesma, Patrick Lee • Inpatient Telemetry Utilization Usman Mughal, Anneris Estevez, Patrick Lee, Barbara Lambl • Health Disparities & Covid-19 Impact on Minorities, sponsored by Dr. Patrick Lee, Chair of Medicine, Dr. Barb Lambl, Infectious Disease 2017-2020 Alexander Gavralidis, Emre Tarhan, Anneris Estevez, Daniela Urma, Austin Turner, Patrick Lee • Expanded Access to Convalescent Plasma for the Treatment of Patients with COVID-19 – 5/2020 implementing use of Convalescent Plasma to MGB Salem hospital in collaboration with research team. Arturo Castro-Diaz, Dr. Daniela Urma • Improving Hospital Care and Post - acute Care of SARS CoV2 patients 4/2020- 8/2020 Caroline Cubbison, Sohaib Ansari, Adam Matos • Code Status Documentation for admitted patients at Salem Hospital - Project accepted to SHM national meeting to be presented in April 2020 Caroline Cubbison, Coleen Reid, Dr. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Hypothermia – Signs and Symptoms Aside from the Cold That Is Felt and the Shivering That May Occur, Initially Mental Function Is Most Affected
December 2010 – ISSUE 123 DIRECTOR’S NOTE As we prepare to embark on a new year, I would like to take a moment to highlight a few of the forestry transportation safety improvements and initiatives that took place in BC in 2010; The establishment of District wide Road Safety Committees throughout the province. Provincial standardization of radio calling procedures and resource road signage. The expansion of the Council’s Trucksafe program to include issues relating to marine and air transportation safety. Moving forward into 2011, further gains in transportation safety awareness and improved results can be expected through the following initiatives; The identification and development of a Log Truck Driver training program. The establishment of provincial level Trucking Safety Technical Advisory Committees. The development of Passenger Safety Guides for helicopter, float plane and marine transportation of forestry workers. Research and development of programs targeted towards improving the health and wellness of drivers. We look forward to your continued interest and support of this publication and the other safety improvement initiatives carried out by the BC Forest Safety Council. Thank you and have a safe 2011 Chuck Carter, RPF Now that winter is in full force, ensuring preparedness and response for the cold and sometimes extreme conditions while working can make a big difference in your day. Vehicles and equipment are susceptible to break down in freezing temperatures. It’s necessary to ensure proper clothing is worn for the outside temperatures but also it is also important to ensure that there are the resources to keep warm for extended exposure within the vehicle. -

Failure of Hypothermia As Treatment for Asphyxiated Newborn Rabbits R
Arch Dis Child: first published as 10.1136/adc.51.7.512 on 1 July 1976. Downloaded from Archives of Disease in Childhood, 1976, 51, 512. Failure of hypothermia as treatment for asphyxiated newborn rabbits R. K. OATES and DAVID HARVEY From the Institute of Obstetrics and Gynaecology, Queen Charlotte's Maternity Hospital, London Oates, R. K., and Harvey, D. (1976). Archives of Disease in Childhood, 51, 512. Failure of hypothermia as treatment for asphyxiated newborn rabbits. Cooling is known to prolong survival in newborn animals when used before the onset of asphyxia. It has therefore been advocated as a treatment for birth asphyxia in humans. Since it is not possible to cool a human baby before the onset of birth asphyxia, experiments were designed to test the effect of cooling after asphyxia had already started. Newborn rabbits were asphyxiated in 100% nitrogen and were cooled either quickly (drop of 1 °C in 45 s) or slowly (drop of 1°C in 2 min) at varying intervals after asphyxia had started. When compared with controls, there was an increase in survival only when fast cooling was used early in asphyxia. This fast rate of cooling is impossible to obtain in a human baby weighing from 30 to 60 times more than a newborn rabbit. Further litters ofrabbits were asphyxiated in utero. After delivery they were placed in environmental temperatures of either 37 °C, 20 °C, or 0 °C and observed for spon- taneous recovery. The animals who were cooled survived less often than those kept at 37 'C. The results of these experiments suggest that hypothermia has little to offer in the treatment of birth asphyxia in humans. -
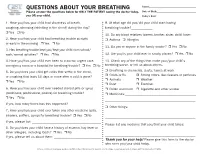
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 74th Oregon Legislative Assembly Oregon Health Services Commission Office for Oregon Health Policy and Research Department of Administrative Services 2007 TABLE OF CONTENTS List of Figures . iii Health Services Commission and Staff . .v Acknowledgments . .vii Executive Summary . ix CHAPTER ONE: A HISTORY OF HEALTH SERVICES PRIORITIZATION UNDER THE OREGON HEALTH PLAN Enabling Legislatiion . 3 Early Prioritization Efforts . 3 Gaining Waiver Approval . 5 Impact . 6 CHAPTER TWO: PRIORITIZATION OF HEALTH SERVICES FOR 2008-09 Charge to the Health Services Commission . .. 25 Biennial Review of the Prioritized List . 26 A New Prioritization Methodology . 26 Public Input . 36 Next Steps . 36 Interim Modifications to the Prioritized List . 37 Technical Changes . 38 Advancements in Medical Technology . .42 CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 47 Age-Related Macular Degeneration (AMD) . 47 Chronic Anal Fissure . 48 Comfort Care . 48 Complicated Hernias . 49 Diagnostic Services Not Appearing on the Prioritized List . 49 Non-Prenatal Genetic Testing . 49 Tuberculosis Blood Test . 51 Early Childhood Mental Health . 52 Adjustment Reactions In Early Childhood . 52 Attention Deficit and Hyperactivity Disorders in Early Childhood . 53 Disruptive Behavior Disorders In Early Childhood . 54 Mental Health Problems In Early Childhood Related To Neglect Or Abuse . 54 Mood Disorders in Early Childhood . 55 Erythropoietin . 55 Mastocytosis . 56 Obesity . 56 Bariatric Surgery . 56 Non-Surgical Management of Obesity . 58 PET Scans . 58 Prenatal Screening for Down Syndrome . 59 Prophylactic Breast Removal . 59 Psoriasis . 59 Reabilitative Therapies . 60 i TABLE OF CONTENTS (Cont’d) CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES (CONT’D) Practice Guidelines (Cont’d) Sinus Surgery . -

Thermoregulatory Correlates of Nausea in Rats and Musk Shrews
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 5, No. 6 Thermoregulatory correlates of nausea in rats and musk shrews Sukonthar Ngampramuan1, Matteo Cerri2, Flavia Del Vecchio2, Joshua J. Corrigan3, Amornrat Kamphee1, Alexander S. Dragic3, John A. Rudd4, Andrej A. Romanovsky3, and Eugene Nalivaiko5 1 Research Center for Neuroscience and Institute of Molecular Bioscience, Mahidol University, Bangkok, Thailand; 2 Department of Biomedical and Motor Sciences, University of Bologna, Bologna, Italy; 3 FeverLab, Trauma Research, St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA; 4 School of Biomedical Sciences, Chinese University of Hong Kong, Hong Kong, China; 5 School of Biomedical Sciences and Pharmacy, University of Newcastle, Newcastle, NSW, Australia. Correspondence to: Eugene Nalivaiko, email: [email protected] Correspondence to: Andrej A. Romanovsky, email: [email protected] Keywords: nausea, chemotherapy, temperature, hypothermia. Received: December 21, 2013 Accepted: February 21, 2014 Published: February 22 2014 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT: Nausea is a prominent symptom and major cause of complaint for patients receiving anticancer chemo- or radiation therapy. The arsenal of anti-nausea drugs is limited, and their efficacy is questionable. Currently, the development of new compounds with anti-nausea activity is hampered by the lack of physiological correlates of nausea. Physiological correlates are needed because common laboratory rodents lack the vomiting reflex. Furthermore, nausea does not always lead to vomiting. Here, we report the results of studies conducted in four research centers to investigate whether nausea is associated with any specific thermoregulatory symptoms. -

Near Drowning
Near Drowning McHenry Western Lake County EMS Definition • Near drowning means the person almost died from not being able to breathe under water. Near Drownings • Defined as: Survival of Victim for more than 24* following submission in a fluid medium. • Leading cause of death in children 1-4 years of age. • Second leading cause of death in children 1-14 years of age. • 85 % are caused from falls into pools or natural bodies of water. • Male/Female ratio is 4-1 Near Drowning • Submersion injury occurs when a person is submerged in water, attempts to breathe, and either aspirates water (wet) or has laryngospasm (dry). Response • If a person has been rescued from a near drowning situation, quick first aid and medical attention are extremely important. Statistics • 6,000 to 8,000 people drown each year. Most of them are within a short distance of shore. • A person who is drowning can not shout for help. • Watch for uneven swimming motions that indicate swimmer is getting tired Statistics • Children can drown in only a few inches of water. • Suspect an accident if you see someone fully clothed • If the person is a cold water drowning, you may be able to revive them. Near Drowning Risk Factor by Age 600 500 400 300 Male Female 200 100 0 0-4 yr 5-9 yr 10-14 yr 15-19 Ref: Paul A. Checchia, MD - Loma Linda University Children’s Hospital Near Drowning • “Tragically 90% of all fatal submersion incidents occur within ten yards of safety.” Robinson, Ped Emer Care; 1987 Causes • Leaving small children unattended around bath tubs and pools • Drinking