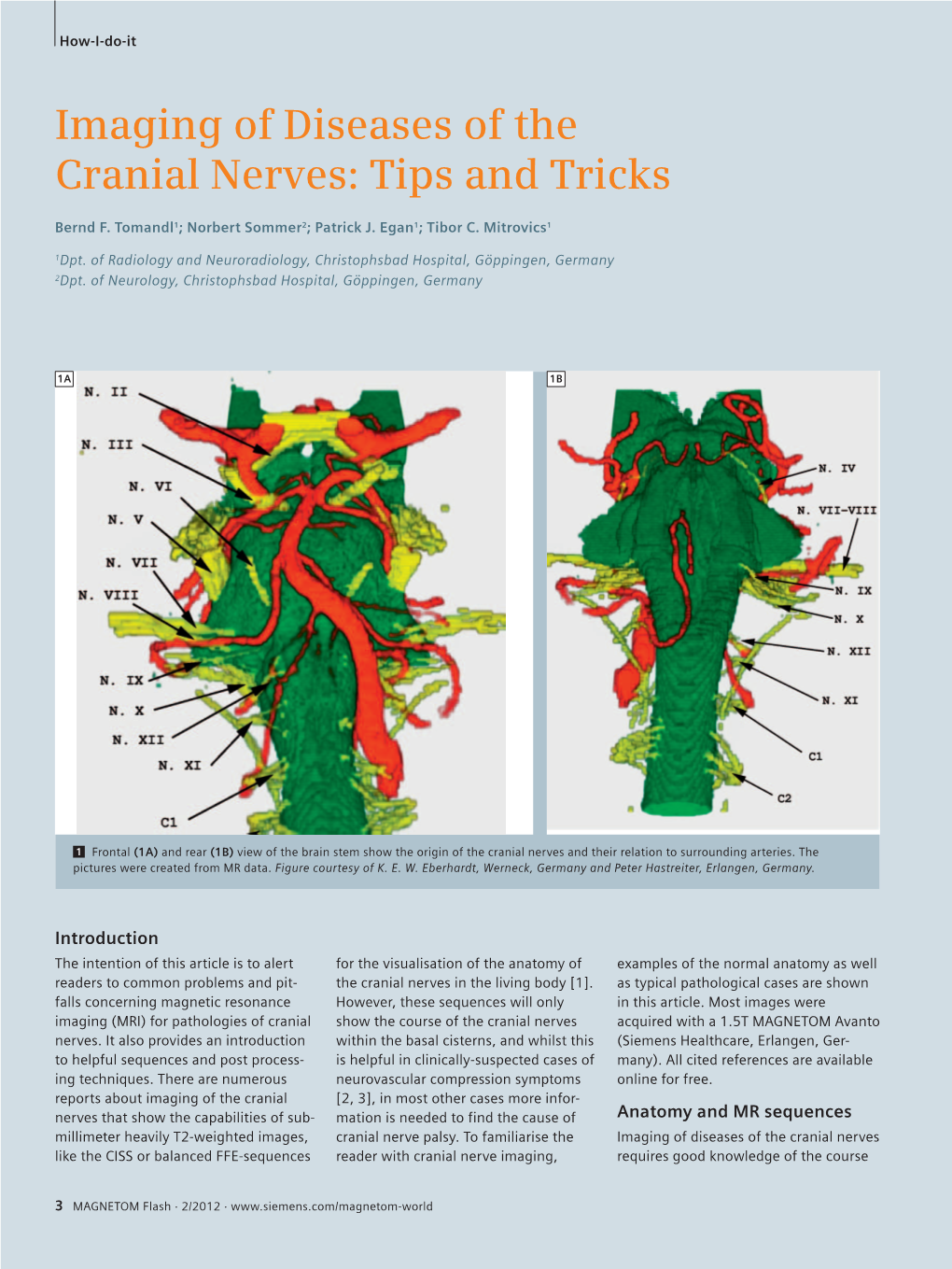
Imaging of Diseases of the Cranial Nerves: Tips and Tricks
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerves
Cranial Nerves Cranial nerve evaluation is an important part of a neurologic exam. There are some differences in the assessment of cranial nerves with different species, but the general principles are the same. You should know the names and basic functions of the 12 pairs of cranial nerves. This PowerPage reviews the cranial nerves and basic brain anatomy which may be seen on the VTNE. The 12 Cranial Nerves: CN I – Olfactory Nerve • Mediates the sense of smell, observed when the pet sniffs around its environment CN II – Optic Nerve Carries visual signals from retina to occipital lobe of brain, observed as the pet tracks an object with its eyes. It also causes pupil constriction. The Menace response is the waving of the hand at the dog’s eye to see if it blinks (this nerve provides the vision; the blink is due to cranial nerve VII) CN III – Oculomotor Nerve • Provides motor to most of the extraocular muscles (dorsal, ventral, and medial rectus) and for pupil constriction o Observing pupillary constriction in PLR CN IV – Trochlear Nerve • Provides motor function to the dorsal oblique extraocular muscle and rolls globe medially © 2018 VetTechPrep.com • All rights reserved. 1 Cranial Nerves CN V – Trigeminal Nerve – Maxillary, Mandibular, and Ophthalmic Branches • Provides motor to muscles of mastication (chewing muscles) and sensory to eyelids, cornea, tongue, nasal mucosa and mouth. CN VI- Abducens Nerve • Provides motor function to the lateral rectus extraocular muscle and retractor bulbi • Examined by touching the globe and observing for retraction (also tests V for sensory) Responsible for physiologic nystagmus when turning head (also involves III, IV, and VIII) CN VII – Facial Nerve • Provides motor to muscles of facial expression (eyelids, ears, lips) and sensory to medial pinna (ear flap). -

Radiation-Related Vocal Fold Palsy in Patients with Head and Neck Carcinoma
Radiation-Related Vocal Fold Palsy in Patients with Head and Neck Carcinoma Pariyanan Jaruchinda MD*, Somjin Jindavijak MD**, Natchavadee Singhavarach MD* * Department of Otolaryngology, Phramongkutklao College of Medicine, Bangkok, Thailand ** Department of Otolaryngology, Nation Cancer Institute of Thailand, Bangkok, Thailand Objective: Recurrent laryngeal nerve damage is a rare complication after receiving conventional radiotherapy for treatment of head and neck cancers and will always be underestimated. The purpose of the present study was to focus on the prevalence of vocal cord paralysis after irradiation and the natural history in those patients. Material and Method: All patients who received more than 60 Gy radiation dose of convention radiotherapy for treatment of head and neck carcinoma from Phramongkutklao Hospital and Nation Cancer Institute of Thailand were recruited in the present study during follow-up period between May 2006-December 2007. The subjects had to have good mobility of bilateral vocal cords with no recurrence or persistent tumor before the enrollment. Baseline characteristic and the associated symptoms of the recurrent laryngeal nerve paralysis were recorded. Laryngeal examinations were done by fiberoptic laryngoscope and in suspicious cases; stroboscope and/or laryngeal electromyography were also performed. The vocal fold paralysis was diagnosed by reviewing recorded VDO by 2 laryngologist who were not involved in the present study. Results: 70 patients; 51 male and 19 female were recruited. 5 patients (7.14%) were diagnosed to have vocal cord paralysis and 2 patients (2.86%) were found to have vocal cord paresis confirmed by electromyography. Most of them were the patients with nasopharyngeal cancers (6/7) with the only one had oropharyngeal cancer (1/7). -

Neurovascular Relationship Between Abducens Nerve and Anterior Inferior Cerebellar Artery
Folia Morphol. Vol. 69, No. 4, pp. 201–203 Copyright © 2010 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl Neurovascular relationship between abducens nerve and anterior inferior cerebellar artery A.F. Esmer1, T. Sen1, B. Bilecenoglu2, E. Tuccar1, A. Uz1, S.T. Karahan1 1Ankara University, Faculty of Medicine, Department of Anatomy, Ankara, Turkey 2Ufuk University, Faculty of Medicine, Department of Anatomy, Ankara, Turkey [Received 1 September 2010; Accepted 13 October 2010] We aimed to study the neurovascular relationships between the anterior infe- rior cerebellar artery (AICA) and the abducens nerve to help determine the pathogenesis of abducens nerve palsy which can be caused by arterial com- pression. Twenty-two cadaveric brains (44 hemispheres) were investigated af- ter injected of coloured latex in to the arterial system. The anterior inferior cerebellar artery originated as a single branch in 75%, duplicate in 22.7%, and triplicate in 2.3% of the hemispheres. Abducens nerves were located between the AICAs in all hemispheres when the AICA duplicated or triplicated. Addi- tionally, we noted that the AICA or its main branches pierced the abducens nerve in five hemispheres (11.4%). The anatomy of the AICA and its relation- ship with the abducens nerve is very important for diagnosis and treatment. (Folia Morphol 2010; 69, 4: 201–203) Key words: abducens nerve palsy, neuroanatomy, vascular compression INTRODUCTION latex. The brains were embalmed in 10% formalin Vascular disorders, infections, tumours, diabe- solution after injection. The dissections were per- tes mellitus, and traumas are the most common formed using a surgical microscope (Opmi 99; Carl causes of abducens nerve palsy, occasionally accom- Zeiss, Gottingen, Germany). -

What Causes Microvascular Cranial Nerve Palsy? It Is Not Always Clear What Causes the Blockage in the Tiny Blood Vessels to the Cranial Nerves
MICROVASCULAR CRANIAL NERVE PALSEY Microvascular Cranial Nerve Palsy (MCNP) is one of the most common causes of acute double vision in the older population. It occurs more often in patients with diabetes and high blood pressure. MCNP is sometimes referred to as a “diabetic” palsy. This condition almost always resolves on its own without leaving any double vision. Six muscles move your eyes. Four of these muscles attach to the front part of your eye (just behind the iris, or the colored portion of the eye). The two muscles that attach to the back of your eye are responsible for some of the up-and-down (vertical) movement and most of the twisting movement of each eye. These six muscles receive their signals from three cranial nerves that begin in the brain stem. What is Microvascular Cranial Nerve Palsy? A nerve cannot function properly when its blood flow is blocked. If the 6th cranial nerve (also called the abducens nerve) is affected, your eye will not be able to move to the outside and you will be aware of double vision, seeing side-by-side images. If the 4th cranial nerve (also called the trochlear nerve) is affected, you will be aware of vertical double vision (one image on top of another). You may be able to eliminate or decrease the double vision by tilting your head towards the opposite shoulder. The 3rd cranial nerve (also called the oculomotor nerve) supplies four of the six eye muscles. These are some of the muscles that control the eyelid and the size of the pupil. -

Vocal Cord Palsy As a Complication of Epidural Anaesthesia
Hindawi Case Reports in Otolaryngology Volume 2018, Article ID 6543656, 3 pages https://doi.org/10.1155/2018/6543656 Case Report Vocal Cord Palsy as a Complication of Epidural Anaesthesia Laura Mc Loughlin and Orla Young Department of Otorhinolaryngology Head & Neck Surgery, Galway University Hospital, Galway, Ireland Correspondence should be addressed to Laura Mc Loughlin; [email protected] Received 8 July 2018; Revised 1 October 2018; Accepted 14 October 2018; Published 25 October 2018 Academic Editor: Rong-San Jiang Copyright © 2018 Laura Mc Loughlin and Orla Young. )is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Cranial nerve palsy is a rare but recognised complication of epidural anaesthesia, most commonly presenting as diplopia secondary to abducens nerve palsy. While upper cranial nerve palsies have been documented on numerous occasions, lower cranial nerve palsies, including recurrent laryngeal nerve palsy, are exceedingly rare. )is case describes a 37-year-old female who, following epidural anaesthesia for spontaneous vaginal delivery of her first child, presented with dysphonia. Flexible laryngoscopy confirmed a left vocal cord palsy, and computed tomography ruled out any mass lesions along the course of the recurrent laryngeal nerve. Here, we discuss a case of vocal cord palsy secondary to epidural anaesthesia, an extremely rare complication. We also discuss the proposed etiology, treatment, and outcomes in patients with this condition. Cranial nerve palsy should be an important differential in patients presenting with dysphonia following spinal or epidural anaesthesia. 1. Introduction only for a recent diagnosis of mild hemochromatosis, and she was on no regular medication. -

Acquired Palsy of the Oculomotor, Trochlear and Abducens Nerves
ACQUIRED PALSY OF THE OCULOMOTOR, TROCHLEAR AND ABDUCENS NERVES l 2 P. A. C. TIFFIN\ C. J. MacEWEN\ E. A. CRAIG and G. CLAYTON Dundee SUMMARY commonly than trochlear nerve palsy. In addition, There have been few studies primarily concerned with although the major cause of ocular palsy was the relative frequencies, aetiologies and prognoses of consistently classified as undetermined (25%), a ocular motor palsies. Those published have emanated relatively high proportion of cases were recorded as largely from neurological tertiary referral centres rather secondary to sinister pathology: neoplasia (18%) and than primary ophthalmology departments. We have aneurysm (7%). performed a retrospective study of all patients with There have been several studies relating to series acquired III, IV or VI cranial nerve palsy who were of patients seen in the more general setting of both s 9 seen in the orthoptic department at Ninewells Hospital, orthoptic and ophthalmic clinics. - However, these Dundee, over the 9 year period from 1984 to 1992. A have concentrated on groups of patients presenting total of 165 cases were identified. VI nerve palsies with the somewhat broader diagnosis of diplopia accounted for the majority of patients (57%), with IV rather than only those with acquired nerve palsies nerve palsies (21%) occurring more frequently than III per se. Acquired ocular motor nerve palsy accounted nerve palsies (17%) and multiple palsies (5%). Thirty for 40-60% of patients presenting with binocular five per cent of cases were of unknown aetiology and diplopia. Although abducens nerve palsy occurred 6 8 9 32% of vascular aetiology. The incidence of sinister most frequently in most of these reports, , , oculo s pathology - neoplasia (2%) and aneurysm (1%) - was motor nerve palsy was found most often in one and surprisingly low. -

Isolated Abducens Nerve Palsy Due to Internal Carotid Artery Aneurysm
IMAGES IN CLINICAL NEUROPHYSIOLOGY Ann Clin Neurophysiol 2020;22(1):46-47 https://doi.org/10.14253/acn.2020.22.1.46 ANNALS OF CLINICAL NEUROPHYSIOLOGY Isolated abducens nerve palsy due to internal carotid artery aneurysm Byung Joon Kim, Kang Min Park Department of Neurology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea Key words: Abducens nerve; Aneurysm; Ophthalmoplegia Received: August 12, 2019 Revised: September 17, 2019 An 80-year-old female was admitted to our hospital with diplopia that had first appeared Accepted: September 19, 2019 3 weeks previously. She did not complain of headache, ocular pain, or tinnitus. A neuro- logic examination revealed limitations in lateral gaze in the left eye, which suggested left abducens nerve palsy (Fig. 1A). No other abnormalities were found in cranial nerve ex- aminations, such as in pupil size or light reflex. We performed serologic testing, including complete blood count, hemoglobin A1C, and the thyroid function test, and the results Correspondence to were within the normal limits. The patient underwent brain magnetic resonance imaging, Kang Min Park which revealed a large cavernous aneurysm in the left internal carotid artery (ICA) origi- Department of Neurology, Haeundae Paik nating at the left cavernous sinus (Fig. 1B). This aneurysm compressed the cavernous sinus Hospital, Inje University College of Medicine, 875 Haeundae-ro, Haeundae-gu, Busan segment of the left abducens nerve, causing abducens nerve palsy. Digital subtraction 48108, Korea angiography confirmed a 2.37 × 1.71 cm aneurysm in the cavernous portion of the left ICA Tel: +82-51-797-1195 (Fig. 1C). The patient underwent coil embolization using the stent-assisted technique, and Fax: +82-51-797-1196 her gaze symptom had improved 4 months later. -

Neuroanatomy, Cranial Nerve 6 (Abducens) - Statpearls - NCBI Bookshelf
12/17/2018 Neuroanatomy, Cranial Nerve 6 (Abducens) - StatPearls - NCBI Bookshelf NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Neuroanatomy, Cranial Nerve 6 (Abducens) Authors Van Nguyen; Matthew Varacallo1. Affilations 1 Department of Orthopaedic Surgery, University of Kentucky School of Medicine Last Update: October 27, 2018. Introduction Cranial nerve six (CN VI), also known as the abducens nerve, is one of the nerves responsible for the extraocular motor functions of the eye, along with the oculomotor nerve (CN III) and the trochlear nerve (CN IV). Structure and Function Unlike the oculomotor nerve and the trochlear nerve, the abducens nerve is a purely somatic nerve, meaning the nerve has no sensory function. Its main function is to carry general somatic efferent nerve axons to innervate the lateral rectus muscle which then abducts the eye on the ipsilateral side. It is also secondarily involved in innervation of the contralateral medial rectus muscle by way of the medial longitudinal fasciculus so that both eyes move laterally in a coordinated manner. Nerves The nerve itself can be divided into four distinct portions: the nucleus, the cisternal portion, the cavernous sinus portion, and the orbital portion. The abducens nucleus resides in the dorsal pons, ventral to the floor of the fourth ventricle, and just lateral to the medial longitudinal fasciculus. About forty percent of the axons project through the ipsilateral medial longitudinal fasciculus to cross over to the contralateral medial rectus subnucleus to eventually innervate the contralateral medial rectus muscle. -

Human Anatomy Lab - Examination of the Cranial Nerves
Utah State University DigitalCommons@USU Undergraduate Honors Capstone Projects Honors Program 5-1993 Human Anatomy Lab - Examination of the Cranial Nerves Jeanne Falk Utah State University Follow this and additional works at: https://digitalcommons.usu.edu/honors Part of the Nervous System Commons Recommended Citation Falk, Jeanne, "Human Anatomy Lab - Examination of the Cranial Nerves" (1993). Undergraduate Honors Capstone Projects. 296. https://digitalcommons.usu.edu/honors/296 This Thesis is brought to you for free and open access by the Honors Program at DigitalCommons@USU. It has been accepted for inclusion in Undergraduate Honors Capstone Projects by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. JEANNE FALK SENIOR PROJECT HUMANANATOMY LAB - EXAMINATIONOF THE CRANIALNERVES The peripheral nervous system consists of twelve pairs of cranial nerves, 31 pairs of spinal nerves, and the nerves of the autonomic nervous system. The cranial nerves are the nerves that leave the brain directly. These nerves control various actions and sensations such as sight, smell, .chewing, and swallowing, and will be the focus of this week's lab. Of the twelve pairs of cranial nerves, two pairs arise from the forebrain, ten pairs arise from the midbrain and brain stem, and all but the Vagus nerve innervates the structures in the head and neck. Each cranial nerve pair is designated with a Roman nwneral in reference to the order in which the nerves are positioned from the front to the back of the brain. The names given to the nerves indicate the structures innervated or the principle functions of the nerves. -

The 12 Cranial Nerves
The 12 Cranial Nerves Nerve # Name Function 1st Olfactory Relays smell 2nd Optic Transmits visual information 3rd Oculomotor External muscles of the eye 4th Trochlear Also supplies muscles of the eye 5th Trigeminal Chewing and sensation in the face 6th Abducent Controls lateral eye movement 7th Facial Muscles of facial expression, taste buds, sensation in fingers and toes, blinking 8th Auditory Hearing and balance 9th Glossopharyngeal Sensation, taste and swallowing 10th Vagus Organs in chest and abdomen 11th Accessory Supplies two neck muscles, the sternomastoid and trapezius 12th Hypoglossal Muscles of the tongue and neck The 12 Cranial Nerves—Detail Cranial Nerve 1 Sensory nerve – Olfactory Nerve – controls sense of smell Cranial Nerve 2 Sensory nerve- Optic Nerve- controls vision by sending information from retina Cranial Nerve 3 Motor nerve- Oculomotor Nerve-Controls most eye muscles. Works closely with Cranial Nerves 4 & 6. Controls eye movement, pupil dilation, and pupillary constriction. It also controls the muscles that elevate the upper eyelids. Cranial Nerve 4 Motor nerve- Trochlear Nerve- Controls the downward and outward movement of the eye. Works closely with Cranial Nerves 3 & 6. Can cause vertical Diplopia (double vision). Weakness of downward gaze can cause difficulty in descending stairs. Cranial Nerve 5 Motor and sensory nerve-Trigeminal Nerve-Carries sensory information from most of the head, neck, sinuses, and face. Also carries sensory information for ear and tympanic membrane. Provides motor supply to the muscles of masticulation (chewing), and to some of the muscles on the floor of the mouth. Also provides motor supply to tensor tympani (small muscle in the middle ear which tenses to protect the eardrum). -

Topography and Cytoarchitecture of the Motor Nuclei in the Brainstem of Salamanders
THE JOURNAL OF COMPARATIVE NEUROLOGY 278:181-194 (1988) Topography and Cytoarchitecture of the Motor Nuclei in the Brainstem of Salamanders GERHARD ROTH, RIISA NISHIKAWA, URSULA DICKE, AND DAVID B. WAKE Department of Biology, University of Bremen, 2800 Bremen 33, Federal Republic of Germany (G.R., U.D.); Museum of Vertebrate Zoology and Department of Zoology, University of California, Berkeley, California 94720 (K.N., D.B.W.) ABSTRACT The organization of the motor nuclei of cranial nerves V (including mesencephalic nucleus), VI, VII, IX, and X is described from HRP-stained material (whole mounts and sections) for 25 species representing five fami- lies of salamanders, and the general topology of the brainstem is considered. Location and organization of the motor nuclei, cytoarchitecture of each nucleus, and target organs for nuclei and subnuclei are described. The trigeminal nucleus is separated distinctly from the facial and abducens nuclei and consists of two subnuclei. The abducens nucleus consists of two distinct subnuclei, one medial in location, the abducens proper, and the other lateral, the abducens accessorius. The facial nucleus has two subnu- clei, and in all but one species it is posterior to the genu facialis. The facial nucleus completely overlaps the glossopharyngeal nucleus and partially overlaps that of the vagus. In bolitoglossine plethodontid salamanders, all of which have highly specialized projectile tongues, the glossopharyngeal and vagus nuclei have moved rostrally to overlap extensively and intermin- gle with the anterior and posterior subnuclei of the facial nerve. In the bolitoglossines there is less organization of the cells of the brainstem nuclei: dendritic trunks are less parallel and projection fields are wider than in other salamanders. -

14 Motor Nucleus of Cranial Nerve Vii (Motor Vii)
263 Brain stem Motor VII 14 MOTOR NUCLEUS OF CRANIAL NERVE VII (MOTOR VII) Before turning to the motor VII, you should note that the pons consists of two zones, a dorsal portion called the tegmentum of the pons and a ventral zone called the basilar pons. The tegmentum contains cranial nerve nuclei and ascending pathways such as the medial lemniscus, lateral lemniscus, ALS (spinothalamic tract), STT (solitariothalamic tract) and TTT (trigeminothalamic tract). The basilar region contains the pontine grey nuclei and massive groups of descending fibers, including the corticospinal, corticobulbar, and corticopontine tracts. Brain stem 264 Motor VII The motor nucleus VII contains motor neurons (branchiomotor) that innervate the muscles of facial expression including the orbicularis oculi (CLOSES eyelid), the stapedius, the stylohyoid and the posterior belly of the digastric. Neurons comprising motor VII possess axons that pursue a rather circuitous route in order to exit the brain stem. Initially they pass dorsally and medially to loop over the abducens nucleus. The fibers then course ventrally and laterally to exit the brain stem. The bump in the floor of the fourth ventricle caused by the motor fibers of C.N. VII looping over the abducens nucleus is called the FACIAL COLLICULUS. A unilateral lesion interrupting the axons of C.N. VII results in the following: On the ipsilateral side, the forehead is immobile, the corner of the mouth sags, the nasolabial folds of the face are flattened, facial lines are lost, and saliva may drip from the corner of the mouth. The patient is unable to whistle or puff the cheek because the buccinator muscle is paralyzed.