Mathematical Programming for the Optimisation of Ambulances Deployment
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Abano Terme Acerra Aci Castello Acqualagna Acquanegra
Abano Terme Alzano Scrivia Azzano San Paolo Belvedere Marittimo Acerra Amelia Azzate Benevento Aci Castello Anagni Bagnaria Benna Acqualagna Ancarano Bagnatica Bentivoglio Acquanegra Cremonese Ancona Bagno A Ripoli Berchidda Adro Andezeno Bagnoli Di Sopra Beregazzo Con Figliaro Affi Angiari Bagnolo Cremasco Bereguardo Afragola Anguillara Veneta Bagnolo Di Po Bergamo Agliana Annicco Bairo Bernareggio Agliano Annone Di Brianza Baone Bertinoro Agliè Antrodoco Baranzate Besana in Brianza Agna Anzola D’Ossola Barasso Besenello Agordo Aosta Barbarano Vicentino Besnate Agrate Brianza Appiano Gentile Barberino Di Mugello Besozzo Agugliano Appiano sulla strada del vino Barberino Val D’Elsa Biassono Agugliaro Aprilia Barbiano Biella Aicurzio Arce Barchi Bientina Ala Arcene Bardello Bigarello Alano Di Piave Arco Bareggio Binago Alba Arconate Bariano Bioglio Alba Adriatica Arcore Barlassina Boara Pisani Albairate Arcugnano Barone Canavese Bolgare Albano Laziale Ardara Barzago Bollate Albaredo Arnaboldi Ardea Barzanò Bollengo Albaredo D’Adige Arese Basaluzzo Bologna Albavilla Arezzo Baselga Di Pinè Bolsena Albese Con Cassano Argelato Basiano Boltiere Albettone Ariccia Basiliano Bolzano Albiano Arluno Bassano Bresciano Bolzano Vicentino Albiate Arquà Petrarca Bassano Del Grappa Bomporto Albignasego Arquà Polesine Bassano In Teverina Bonate Sotto Albino Arre Bastida Pancarana Bonemerse Albiolo Arsago Seprio Bastiglia Bonorva Albisola Superiore Artegna Battaglia Terme Borghetto S. Spirito Albuzzano Arzachena Battuda Borgo San Dalmazzo Aldeno Arzano Baveno -

Trasferimenti
********************************************************************************** * SI-13-SM-PDO2B * * * * SISTEMA INFORMATIVO MINISTERO DELLA PUBBLICA ISTRUZIONE * * * * * * SCUOLA SECONDARIA DI PRIMO GRADO * * * * * * UFFICIO SCOLASTICO REGIONALE PER IL VENETO * * * * * * UFFICIO SCOLASTICO PROVINCIALE : VICENZA * * * * * * ELENCO DEI TRASFERIMENTI E PASSAGGI DEL PERSONALE DOCENTE DI RUOLO * * * * * * ANNO SCOLASTICO 2012/2013 * * * * * * ATTENZIONE: PER EFFETTO DELLA LEGGE SULLA PRIVACY QUESTA STAMPA NON * * CONTIENE ALCUNI DATI PERSONALI E SENSIBILI CHE CONCORRONO ALLA * * COSTITUZIONE DELLA STESSA. AGLI STESSI DATI GLI INTERESSATI O I * * CONTROINTERESSATI POTRANNO EVENTUALMENTE ACCEDERE SECONDO LE MODALITA' * * PREVISTE DALLA LEGGE SULLA TRASPARENZA DEGLI ATTI AMMINISTRATIVI. * * * * * ********************************************************************************** POSTI DI SOSTEGNO PER MINORATI PSICO-FISICI ***** TRASFERIMENTI NELL'AMBITO DEL COMUNE 1. DE MATTEIS PAOLO . 5/ 1/62 (NA) TIT. SU POSTI DI SOSTEGNO (MIN. PSICO-FIS.) DA : VIMM86601P - SMS VIA PRATI VICENZA ( VICENZA ) A : VIMM86701E - SMS VIA CARTA VICENZA ( VICENZA ) PUNTI 78 2. GAIANIGO MARTA . 25/ 5/73 (VI) TIT. SU POSTI DI SOSTEGNO (MIN. PSICO-FIS.) DA : VIMM869016 - SMS VIA L.ANTONINI VICENZA ( VICENZA ) A : VIMM86601P - SMS VIA PRATI VICENZA ( VICENZA ) PUNTI 24 3. PASCALI SIMONA . 13/ 3/69 (LE) TIT. SU POSTI DI SOSTEGNO (MIN. PSICO-FIS.) DA : VIMM88801G - SMS P.LE TRENTO -BASSANO DEL G. ( BASSANO DEL GRAPPA ) A : VIMM88101R - SMS"BELLAVITIS" BASSANO DEL GR. ( BASSANO DEL GRAPPA ) SOPRANNUMERARIO TRASFERITO A DOMANDA CONDIZIONATA PUNTI 64 4. PERROTTA CHIARA . 9/ 8/81 (LE) TIT. SU POSTI DI SOSTEGNO (MIN. PSICO-FIS.) DA : VIMM84001E - IC VICENZA 3 - "SCAMOZZI" ( VICENZA ) A : VIMM87001A - SMS " A.GIURIOLO" VICENZA ( VICENZA ) PUNTI 23 5. TROMBETTA LUCIA PIA . 21/ 9/78 (FG) TIT. SU POSTI DI SOSTEGNO (MIN. PSICO-FIS.) DA : VIMM88801G - SMS P.LE TRENTO -BASSANO DEL G. ( BASSANO DEL GRAPPA ) A : VIMM88101R - SMS"BELLAVITIS" BASSANO DEL GR. -

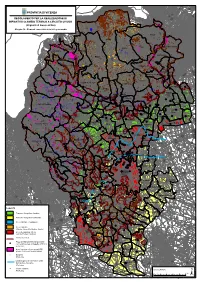
P.A.T.I. Provincia Di Vicenza
COMUNE DI BRESSANVIDO COMUNE DI POZZOLEONE P.A.T.I. PROVINCIA DI VICENZA Elaborato Scala 4 REGIONE VENETO PROVINCIA DI VICENZA Settore Urbanistica Norme Tecniche COMUNE DI BRESSANVIDO Il Sindaco Il Responsabile Area Tecnica ADEGUATE ALLA CONFERENZA DI SERVIZI COMUNE DI POZZOLEONE Il Sindaco Il Responsabile Area Tecnica PROGETTISTA COORDINAMENTO ATTIVITA’ SPECIALISTICHE DOTT.PIAN.TER.LE ALICE ZANELLA STUDIO ASSOCIATO ZANELLA Noventa Vicentina (VI) Collaboratori: arch. Aldo Marangon arch Claudio Seno ANALISI AGRONOMICHE, GEOLOGICHE E COMPATIBILITA’ IDRAULICA STUDIO MASTELLA San Pietro in Cariano (VR) Dott. Geol. Cristiano Mastella V.A.S. e V.INC.A. STUDIO LOTTO Montegalda (VI) Dott. Agr. Riccardo Lotto via Roma 5, 36026 Pojana Maggiore (VI) www.abitat.it – [email protected] DATA: 28/09/2012 Norme Tecniche Comuni di Bressanvido e Pozzoleone P.A.T.I. INDICE TITOLO I° - DISPOSIZIONI GENERALI ............................................................... 7 Art. 1 - Contenuti del PATI .................................................................................. 7 Art. 2 - Elaborati del PATI ................................................................................... 8 Art. 3 - Efficacia ed attuazione del PATI ................................................................ 9 Art. 4 - Disposizioni transitorie ........................................................................... 10 TITOLO II° - ASSETTO DEL TERRITORIO .......................................................... 11 Art. 5 - Assetto del territorio e definizione degli -

DIRITTO ALLO STUDIO Ufficio Scolastico Provinciale Di VI
Ufficio Scolastico Regionale per il Veneto Graduatoria permessi DIRITTO ALLO STUDIO Ufficio Scolastico Provinciale di VI Anagrafica Richiesta Scuola Stato pr. pos. ID nome nascita qualifica chiede Codice Denominazione Ore richieste scuola VI 1 22868 LA SPADA ANTONINO 14/09/1972 SecII Rinnovo VIIS01700L Istituto Superiore (St.) Remondini di 75 BASSANO DEL GRAPPA VI 2 23741 GIUNGATO MARIA 06/10/1972 SecII Rinnovo VIRF020004 I.P. per i Servizi Sociali (St.) B. Montagna di 100 VICENZA VI 3 22118 TARANTINO GRAZIELLA 07/05/1980 SecI Rinnovo VIIC88600V Istituto Comprensivo (St.) di ASIAGO 100 VI 4 23111 LICARI ROSALBA 01/07/1980 SecI Rinnovo VIIC877004 Istituto Comprensivo (St.) 2° Loc. Alte 90 Ceccato di MONTECCHIO MAGGIORE VI 5 21857 LAIACONA GIUSEPPE 08/04/1982 SecII Rinnovo VIIS00400E Istituto Superiore (St.) Umberto Masotto di 125 NOVENTA VICENTINA VI 6 23669 SAVONE GAETANO 08/08/1980 SecII Rinnovo VIIS00400E Istituto Superiore (St.) Umberto Masotto di 125 NOVENTA VICENTINA VI 7 22172 COSTENARO PAMELA 07/04/1974 Pri Rinnovo VIIC83800D Istituto Comprensivo (St.) T. Vecellio di 125 SARCEDO VI 8 21994 SALZILLO GIUSEPPE 14/10/1976 SecI Rinnovo VIIC87900Q Istituto Comprensivo (St.) 2 G.Parise di 150 ARZIGNANO VI 9 23790 MORACCHIATO SARA 30/09/1965 Pri Rinnovo VIIC83600T Istituto Comprensivo (St.) Monte Pasubio di 125 TORREBELVICINO VI 10 22004 BRIGANTE NUNZIO BIAGIO 27/03/1986 SecI Rinnovo VIIC87900Q Istituto Comprensivo (St.) 2 G.Parise di 150 ARZIGNANO VI 11 21833 CRACCO ANNA OFELIA 29/01/1986 SecII Rinnovo VIIS00300P Istituto Superiore (St.) Luzzatti di VALDAGNO 125 VI 12 21863 MARCHIOTTO CHIARA 25/08/1984 SecII Rinnovo VIIS00400E Istituto Superiore (St.) Umberto Masotto di 125 NOVENTA VICENTINA VI 13 22635 SCATTOLA DANIELA 13/05/1973 SecI Rinnovo VIIC82200X Istituto Comprensivo (St.) P. -

New Hexapodid Crabs from the Eocene of Vicenza (NE Italy) (Crustacea, Decapoda, Brachyura, Hexapodidae)
Atti Soc. it. Sci. nat. Museo civ. Stor. nat. Milano, 151 (I): 51-75, Gennaio 2010 Antonio De Angeli *, Danièle Guinot ** & Alessandro Garassino *** New hexapodid crabs from the Eocene of Vicenza (NE Italy) (Crustacea, Decapoda, Brachyura, Hexapodidae) Abstract - The Hexapodidae was known to date from the Cenozoic of Veneto by Stevea cesarii Beschin, Busulini, De Angeli & Tessier, 1994, from the middle Eocene of Chiampo Valley (Vicenza), and Palaeopinnixa sp. from the upper Eocene of Possagno (Treviso). Recent discoveries from the Eocene of Vicenza area allowed to describe three new genera and four new species of hexapodids. Bellhexapus granulatus n. gen., n. sp., Eohexapus albertii n. gen., n. sp., and Eurohexapus lobatus n. gen., n. sp. from the middle Eocene of “Albanello” quarry at Nogarole Vicentino (Vicenza), and Palaeopinnixa alontensis n. sp. from the upper Eocene of Alonte (Vicenza). Bellhexapus granulatus n. gen., n. sp. and Eurohexapus lobatus n. gen., n. sp. preserve the carapace, the ventral and abdominal male parts, while Eohexapus albertii n. gen., n. sp. preserves the carapace, the ventral and abdominal female parts. Palaeopinnixa alontensis n. sp. preserves instead only the carapace. Key words : Crustacea, Decapoda, Hexapodidae, Eocene, NE Italy. Riassunto - Nuovi crostacei hexapodidi dell’Eocene di Vicenza (NE Italia) (Crustacea, Decapoda, Brachyura, Hexapodidae). La famiglia Hexapodidae era fi nora conosciuta nel Terziario del Veneto con Stevea cesarii Beschin, Busulini, De Angeli & Tessier, 1994 dell’Eocene medio della Valle del Chiampo (Vicenza) e Palaeo- pinnixa sp. dell’Eocene superiore di Possagno (Treviso). Recenti ritrovamenti nelle rocce eoceniche del Vicentino hanno permesso di descrivere tre nuovi generi e quattro nuove specie di hexapodidi. -

Corpo Elettorale Attivo Al 31/10/2018 Allegato N
PROVINCIA DI VICENZA - CORPO ELETTORALE ATTIVO AL 31/10/2018 ALLEGATO N. 1 PROVINCIA DI VICENZA ELEZIONI DEL PRESIDENTE DELLA PROVINCIA CORPO ELETTORALE ATTIVO AL 31/10/2018 CARICA FASCIA COMUNE COGNOME NOME (SINDACO / CONSIGLIERE) 1 1 A AGUGLIARO ANDRIOLO ROBERTO SINDACO 2 2 A AGUGLIARO VIERO LUCIANO CONSIGLIERE 3 3 A AGUGLIARO GNESIN ALESSANDRO CONSIGLIERE 4 4 A AGUGLIARO GOBBATO PAOLO CONSIGLIERE 5 5 A AGUGLIARO GRAZIAN SIMONE CONSIGLIERE 6 6 A AGUGLIARO SILLO ZEFFERINO CONSIGLIERE 7 7 A AGUGLIARO BOROTTO MIRCO CONSIGLIERE 8 8 A AGUGLIARO DI BARTOLOMEO NICOLA CONSIGLIERE 9 9 A AGUGLIARO BORGHETTINI MASSIMO CONSIGLIERE 10 10 A AGUGLIARO RAPPO GIOVANNI CONSIGLIERE 11 11 A AGUGLIARO CAMPESATO PAOLO CONSIGLIERE 12 1 A ALBETTONE FORMAGGIO JOE SINDACO 13 2 A ALBETTONE ZUECCO IVO CONSIGLIERE 14 3 A ALBETTONE TRISSINO RICCARDO CONSIGLIERE 15 4 A ALBETTONE MEGGIORIN SILVIA CONSIGLIERE 16 5 A ALBETTONE FONTANA FRANCESCO CONSIGLIERE 17 6 A ALBETTONE CAROTTA PATRIZIO CONSIGLIERE 18 7 A ALBETTONE BOGGIAN MASSIMO CONSIGLIERE 19 8 A ALBETTONE CURIELE FIORELLA CONSIGLIERE 20 9 A ALBETTONE CORRADIN ANGELICA CONSIGLIERE 21 10 A ALBETTONE PERDONCIN DAVIDE CONSIGLIERE 22 1 A ALONTE ADAMI LEONARDO SINDACO 23 2 A ALONTE COQUINATI MARCO CONSIGLIERE 24 3 A ALONTE BIASIN ANNA CONSIGLIERE 25 4 A ALONTE BRUN STEFANIA CONSIGLIERE 26 5 A ALONTE BELLINI MAURIZIO CONSIGLIERE 27 6 A ALONTE AMBROSINI ENRICO CONSIGLIERE 28 7 A ALONTE VIALE GABRIELE CONSIGLIERE 29 8 A ALONTE BOLLA PAOLO CONSIGLIERE 30 9 A ALONTE VIANELLO ARIOSTO CONSIGLIERE 31 1 D ALTAVILLA VICENTINA -

Consorzio Di Vicenza Nord
Castelnovo Gambugliano Villaverla CONSORZIO DI Monteviale An exciting Villaverla discovery of VICENZA NORD our territory Costabissara Caldogno Isola Vicentina Monteviale Isola Vicentina Caldogno Costabissara Castelnovo Gambugliano ITALY VENETO Veneto Vicenza Venice VICENZA Caldogno Costabissara Gambugliano Vicenza Isola Vicentina / Castelnovo Monteviale Villaverla Index INTRODUCTION 01 PRO LOCO CALDOGNO 02 PRO LOCO COSTABISSARA 10 PRO LOCO GAMBUGLIANO 18 PRO LOCO ISOLA VICENTINA / CASTELNOVO 22 PRO LOCO MONTEVIALE 34 PRO LOCO VILLAVERLA 44 Every year the Consorzio Pro Loco Vicenza Nord [Association of Pro Locos of northern Vicenza N.d.T.] collaborates with UNPLI (National Civil Service) and contributes to the project PROTECTION AND PROMOTION OF LINGUISTIC AND CULTURAL PATRIMONY OF VENETO REGION. Samira De Solda is a volunteer at UNPLI and is an extremely motivated and interesting resource in this field. With her precious help the Consorzio created, planned and developed this brochure. The aim of our brochure is to promote Sites of Interest as well as local products and in particular De.Co. Castelnovo Products (Denominazione Comunale products) which are local G products that are typical of each municipality. Samira, with her enthusiasm and perseverance, was able to collect and organize a lot of information such as stories and curiosities about the villas, churches, oratories, Villaverla CONSORZIO DI locations and traditions. Through her wonderful dedication to this project Meviale she was able to put together various pieces of information and make them Villaverla accessible to a general audience. The fruit of this project is this brochure that will be distributed in the local territories of Caldogno, Castelnovo, An exciting Costabissara, Gambugliano, Isola Vicentina, Monteviale and discovery of VICENZA NORD Villaverla, in order to keep the rich linguistic and cultural patrimony alive. -
Elementi Conoscitivi Ai Fini Del Geoscambio
%%% % % %%%%%%%%% %% %%% % % %%%%%%%%%%%% %%%% %%%% % %%%% % %%%%%%%% % %%%% % %%%%% %% %%%%%%%%%%%%%%%%%% % PROVINCIA DI VICENZA %%%%% % %% %%% %% % % % %% % %%%%%%% % %%%%%% % %%%%% % % %%%%%% %% %%% %%% %% % %%%%%%% % % %%% % %%%%%%%%%%%B% % % % % %% %%%%%%%%%% %%%%%%%% %% % %%%%%%%% % % %% %%%%%%%%%%% %%%% %%%%%% B %%%%% REGOLAMENTO PER LA REALIZZAZIONE DI %%%%%%%%%%%%%%% %%%% %%%%% % % %B% % % %%%%%% %% %% % %% %%% % % %% %%% %%%%%%%%%% %% % %% %%% %%% % % %%%%%%%%%%%%%%%% % % %%%%%%%%%%%%%% %%%%%% %% %%%% %%%%%%%%%%%%%%%% % % % %%%%%%%%%%% %% IMPIANTI DI SCAMBIO TERMICO A CIRCUITO CHIUSO % %%% % %%%% %% %%% % %% %%%%%% % %%%% %% % % %%%% %%%%%%% %%% % % % %%% %%%% % %%% % % %%%%%%%%%%%%%% %% % % % % %%%%%%% % %%%%%%%%%%% % % % %%%%%% %%%%%%%%%% % %%%%%% %% % !( (Impianti di Geoscambio) % %%%%%%%%%%%%%%%%%%%%%% %%%% % % %%% %% %%%% %%%%%% % %%%%%%% % % % %%%%%%% %% % % % % % % % %% %%% %%%%%%%%%% % %%%%% %%% B % B % %% % % %B% % %%%% % B BBBB % %% % % %% % B % Allegato 1b - Elementi conoscitivi ai fini del geoscambio BB %% % %%% %%%%% B B % %% BB % %%%% %% %%%%%%% % B % % %%%%% %%%%%% %% %%%% % % % % %%%%% % %%%%% B% %%% %% B % % % %%%% % %%%%%% % % %%%%% %%%% % %% %%% %%% % % %%%% %% %%%%% %% % %% % %%%%%%% % % %%%%% % %% %% % Enego %%%% %%% % %%% % % %% % %% % %% % % % %% B % % %%% % B % % % % % % % %% B % %%% % %%%%%%%%%%%%% %% %% % % % Asiago%%%% %%%%%%%%%%%%%%%% % % %%%% % % %%%%%%%%% % % % %%%% %% %%%%%% %%%%% % % %% %%%% %%% %% % % % % % %% % %% %%%% %% % % % % % % %%%%% % % B % % % % B% % % % % % % % %%%%%% % % % %% % % %% -

Comune Di Marano Vicentino
Protocollo p_vi/aooprovi GE/2020/0042665 del 12/10/2020 - Pag. 1 di 162 REGIONE VENETO PROVINCIA DI VICENZA COMUNE DI MARANO VICENTINO PROCEDURA DI VERIFICA DI ASSOGGETTABILITÀ AI SENSI DEL L'ART. 19 DEL D.Lgs 152/06 e ss.mm.ii. PER L'INSTALLAZIONE DEL NUOVO IMPIANTO DI GESTIONE E RECUPERO RIFIUTI SITO NEL COMUNE DI MARANO VICENTINO (VI) STUDIO PRELIMINARE AMBIENTALE Committente: Vallortigara Servizi Ambientali S.p.A. Sede legale: Via dell'Artigianato n°21 36036 TORREBELVICINO cod. fisc. e P.I. 02427080243 Oggetto: Elaborato: STUDIO PRELIMINARE AMBIENTALE: RELAZIONE GENERALE S1 Progettisti: Scala: - Data: OTTOBRE 2020 Direttore tecnico: Ing. Antonio Colella File: Collaboratori: Ing. Francesco Bertoncin s1907bk91-2.docx Ing. Gianluca Notarrigo Ing. Alberto Colella Sost. il: Ing. Giovanni Stocco s1907bk91-1.docx IL PRESENTE DISEGNO E' DI NOSTRA PROPRIETA' ED E' SOTTO LA PROTEZIONE DELLA LEGGE SULLA PROPRIETA' LETTERARIA, NE E' QUINDI VIETATA, PER QUALSIASI MOTIVO, LA RIPRODUZIONE E CONSEGNA A TERZI rev. data descrizione oper. verif. R.C. approv. D.T. rev. 1 04/08/2020 SECONDA EMISSIONE 123 117 113 rev. 2 02/10/2020 TERZA EMISSIONE 123 117 113 Protocollo p_vi/aooprovi GE/2020/0042665 del 12/10/2020 - Pag. 2 di 162 Vallortigara Servizi Ambientali spa - Studio Preliminare Ambientale Premessa INDICE 1. PREMESSA ....................................................................................................................... 5 1.1 Iter autorizzativo procedura di Verifica di assoggettabilità a V.I.A. .............................. 8 1.2 -

Verbale Della Commissione Del 25/11/2020
PROVINCIA DI VICENZA Domicilio fisc.: C.trà Gazzolle, 1 - 36100 VICENZA - C. Fisc. P. IVA 00496080243 Prot. vedasi file di segnatura Oggetto: BANDO PER L’ASSEGNAZIONE DI CONTRIBUTI FINALIZZATI AL RECUPERO DEI VALORI PAESAGGISTICI E RIQUALIFICAZIONE DI SITI DEGRADATI. ANNO 2020 VERBALE DELLA COMMISSIONE Il giorno 25 Novembre 2020, alle ore 12.00 nella sede della Provincia di Vicenza, Contrà Gazzolle n. 1, si è riunita la Commissione istituita con nota dirigenziale prot. 49466 del 20/11/2020 per la selezione dei Comuni assegnatari del contributo ed i relativi muri sui quali dovranno essere realizzate le opere di Street Art . Sono presenti i signori: Arch. Roberto Josè Bavaresco, presidente; Arch. Chiara Zorzan, componente; Arch. Laura Pellizzari, componente; Arch. Simone Picelli, componente; geom. Nicoletta Frosi, verbalizzante. Premesso che ► Con decreto del Presidente della Provincia n. 86 del 15/09/2020 è stato approvato un bando per l’assegnazione dei contributi per il recupero dei valori paesaggistici e la riqualificazione di siti degradati nel territorio dei Comuni nei quali viene esercitata la delega in materia di paesaggio. ► La somma da destinare a contributo è pari a € 40.000. ► Il bando ha previsto che la somma è indirizzata alla riqualificazione di spazi urbani degradati attraverso la realizzazione di opere di street art su muri di immobili, individuati dalle amministrazioni comunali e ricadenti in ambiti degradati che necessitano di interventi di riqualificazione urbana, secondo quanto enunciato dall’art. 167 comma 6 del dlgs 42/2004, nonché l’attribuzione di € 4.000 per muro, per un massimo di n. 2 muri per comune dando priorità ai comuni che non sono stati assegnatari del contributo nella precedente edizione. -

Tartufo Nero Pregiato Veneto
COMELICO SUPERIORE O S. NICOLO DI COMELICO O S. PETRO DI CADORESAPPADA DANTA O O O S. STEFANO DI CADORE AURONZO DI CADOROE O OAURONZO DI CADORE CORTINA D'AMPEZZO O VIGO DI CADOREVIGO DI CADORE O LOZZO DI CADORE LIVINALLONGO DEL COL DI LANA LIVINALLONGO DEL COL DI LANA O LORENZAGO DI CADORE O O O DOMEGGE DI CADORE S. VITO DI CADORE O O CALALZO DI CADORE COLLE S. LUCIA O O OSELVA DI CADORE BORCA DI CADORE PIEVE DI CADORE ROCCA PIETORE O O O VODO CADORE OVALLE DI CADORE O O VALLE DI CADORE ALLEGHE PERAROLO DI CADORE O CIBIANA O ZOPPE DI CADORE O ZOLDO ALTOO VALOLADA AGORDINA O O S. TOMASO AGORDINO FALCADE CANALE D'AGORDO O O OCENCENIGHE AGORDINO FORNO DI ZOLDO O OSPITALE DI CADORE O TAIBON AGORDINO O CASTELLO LAVAZZO AGORDO O LONGARONE VOLOTAGO AOGORDINO O O RIVAMONTE AGORDINO O GOSALDO O SOVERZENE O PONTE NELLE ALPI O PIEVE D'ALPAGOCHIES D'ALPAGO OPIEVE OD'ALPAGO PUOS D'ALPAGO SOSPIROLO BELLUNO O O O TAMBRE FARRA D'ALOPAGO O SEDICO S. GREGORIOO NELLE ALPI O LIMANA CESIOMAGGIORE O O S. GIUSTINA OSANTA GIUSTINA TRICHIANA O MEL O SOVRAMONTE LENTIAI LAMONO PEDAVENA O O O FELTRE FONZASO O O REVINE LAGO O VITTORIO VENETOSARMEDE SEREN DEL GRAPPA O O ARSIE O TARZO CAPPELLA MAGGIORE O CISON DI VALMARINOO O O CORDIGNANO FOLLINA O COLLE UMBEROTO MIANE ORSAGO O GODEGAO DI SANT'URBANO ENEGO VAS O O O O REFROONTOLO QUERO O S. PIETRO DI FELETTO S. FIOR CISMON DEL GRAPPA O OOSEGUSINO O O ALANO DI PIAVE OSEGUSINO FARRA DI SOLIGO SEGUSINO O PIEVE DI SOLIGO S. -

COMUNE DI SALCEDO (Provincia Di Vicenza)
COMUNE DI SALCEDO (Provincia di Vicenza) __________ VERBALE DI DELIBERAZIONE DEL CONSIGLIO COMUNALE __________ COPIA ANNO 2018 N. 24 del Reg. Delibere OGGETTO: ADESIONE AL PARTENARIATO DEL GRUPPO DI AZIONE LOCALE (G.A.L.) MONTAGNA VICENTINA S.C.A.R.L. L'anno 2018 , il giorno 28 del mese di Novembre alle ore 20:30 nella sala consigliare si è riunito il Consiglio Comunale. Fatto l'appello nominale risultano: Presente/Assente p.i. Gasparini Giovanni Sindaco Presente Antonio Carli Michele Vice Sindaco Presente Xausa Rudy Consigliere Presente Lazzaretti Antonio Consigliere Assente Lazzaretti Walter Consigliere Presente Pavan Aldo Consigliere Presente Lavarda Davide Consigliere Presente Tura Carlo Consigliere Assente Valle Giulia Consigliere Presente Pasquale Federico Consigliere Assente Azzolin Umberto Consigliere Presente Galvan Giada Assessore Esterno Presente N. Presenti 8 N. Assenti 3 Assiste il Segretario Comunale Dott.ssa Antonietta Michelini. Constatato il numero degli intervenuti, assume la presidenza il Sig. p.i. Giovanni Antonio Gasparini nella sua qualità Sindaco ed espone gli oggetti inscritti all'ordine del giorno e su questi il Consiglio Comunale adotta la seguente deliberazione: Comune di Salcedo – Deliberazione n. 24 del 28/11/2018 1 OGGETTO: ADESIONE AL PARTENARIATO DEL GRUPPO DI AZIONE LOCALE (G.A.L.) MONTAGNA VICENTINA S.C.A.R.L. IL CONSIGLIO COMUNALE PREMESSO CHE: - il gruppo di azione locale (GAL) Montagna Vicentina, secondo quanto dall’art. 34 del Reg. (UE) 1303/2013, è un gruppo composto da rappresentanti degli interessi socio-economici locali, sia pubblici che privati, che si riuniscono in un partenariato con lo scopo di elaborare ed attuare strategie di sviluppo locale di tipo partecipativo (art.