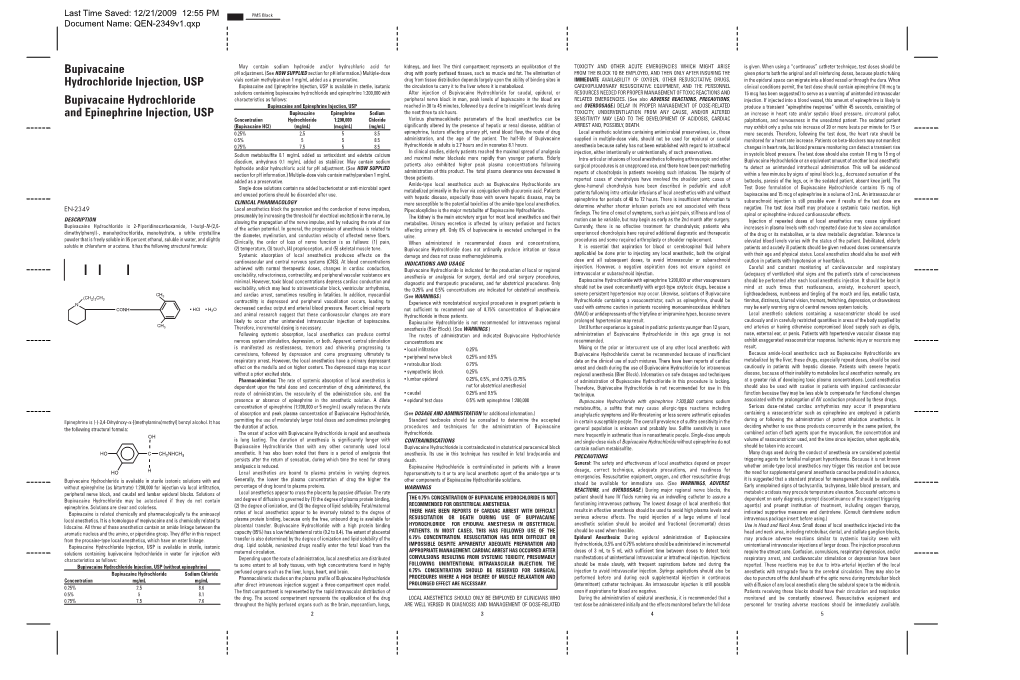
Bupivacaine Hydrochloride Injection, USP Is Available in Sterile, Isotonic Drug
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bupivacaine Injection Bp
PRODUCT MONOGRAPH INCLUDING CONSUMER INFORMATION BUPIVACAINE INJECTION BP Bupivacaine hydrochloride 0.25% (2.5 mg/mL) and 0.5% (5 mg/mL) Local Anaesthetic SteriMax Inc. Date of Preparation: 2770 Portland Dr. July 10, 2015 Oakville, ON, L6H 6R4 Submission Control No: 180156 Bupivacaine Injection Page 1 of 28 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .................................................................... 3 SUMMARY PRODUCT INFORMATION ................................................................................... 3 INDICATIONS AND CLINICAL USE ......................................................................................... 3 CONTRAINDICATIONS .............................................................................................................. 3 WARNINGS AND PRECAUTIONS ............................................................................................. 4 ADVERSE REACTIONS ............................................................................................................... 9 DRUG INTERACTIONS ............................................................................................................. 10 DOSAGE AND ADMINISTRATION ......................................................................................... 13 OVERDOSAGE ........................................................................................................................... 16 ACTION AND CLINICAL PHARMACOLOGY ....................................................................... 18 STORAGE -

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -

Epidural Analgesia Guidelines for the Rhw
LOCAL OPERATING PROCEDURE CLINICAL POLICIES, PROCEDURES & GUIDELINES Approved by Quality & Patient Care Committee 2 June 2016 EPIDURAL ANALGESIA GUIDELINES FOR THE RHW SECTION 1 RATIONAL SECTION 2 EDUCATION OF NURSING/MIDWIFERY STAFF SECTION 3 INDICATIONS/DOSING/OBSERVATIONS SECTION 4 PROCEDURE SECTION 5 MANAGEMENT GUIDELINES SECTION 6 COMPLICATIONS & MANAGEMENT SECTION 7 REMOVAL OF EPIDURAL CATHETER SECTION 8 CONCURRENT USE OF ANTICOAGULANTS APPENDIX 1 EPIDURAL DISCHARGE ADVICE APPENDIX 2 PATIENT DISCHARGE INSTRUCTIONS AFTER EPIDURAL BLOOD PATCH …./2 2. LOCAL OPERATING PROCEDURE CLINICAL POLICIES, PROCEDURES & GUIDELINES Approved by Quality & Patient Care Committee 2 June 2016 EPIDURAL ANALGESIA GUIDELINES FOR THE RHW cont’d SECTION 1 – RATIONAL • The blockade of transmission of pain impulses by the use of local anaesthetic medication can reduce the body’s physiological response to the stress of pain. • Systemic opioids only, although a strong pain reliever, may cause respiratory depression, sedation, nausea, vomiting, confusion, lightheadedness, constipation and immobilisation. • The goal of regional axial blockade (epidural analgesia) in moderate to severe pain is to diminish the development of an efficient pain pathway, by blocking conduction along pain nerve fibers. • Epidural infusions however, requires constant assessment and at times intervention in order to provide this level of pain control. • Vigilance is required as tolerance to local anaesthetic can develop which can require more agent be infused in order to maintain the level of block. • Other factors such as patient position and movement will influence the effectiveness of the infusion, as will the precision of the pump and time spent when changing infusions. • Opioids added to an epidural infusion can augment the analgesic effect of the local anaesthetic block. -

Bupivacaine Hcl Rx Only 0.5% with Epinephrine 1:200,000 (As Bitartrate) (Bupivacaine Hydrochloride and Epinephrine Injection, USP)
Bupivacaine HCl Rx only 0.5% with epinephrine 1:200,000 (as bitartrate) (bupivacaine hydrochloride and epinephrine injection, USP) THIS SOLUTION IS INTENDED FOR DENTAL USE. DESCRIPTION Bupivacaine hydrochloride is (±) -1-Butyl-2´,6´-pipecoloxylidide monohydrochloride, monohydrate, a white crystalline powder that is freely soluble in 95 percent ethanol, soluble in water, and slightly soluble in chloroform or acetone. It has the following structural formula: Epinephrine is (-)-3,4-Dihydroxy-α-[(methylamino)methyl] benzyl alcohol. It has the following structural formula: BUPIVACAINE HCl is available in a sterile isotonic solution with epinephrine (as bitartrate) 1:200,000. Solutions of BUPIVACAINE HCl containing epinephrine may not be autoclaved. BUPIVACAINE HCl is related chemically and pharmacologically to the aminoacyl local anesthetics. It is a homologue of mepivacaine and is chemically related to lidocaine. All three of these anesthetics contain an amide linkage between the aromatic nucleus and the amino or piperidine group. They differ in this respect from the procaine-type local anesthetics, which have an ester linkage. CLINICAL PHARMACOLOGY BUPIVACAINE HCl stabilizes the neuronal membrane and prevents the initiation and transmission of nerve impulses, thereby effecting local anesthesia. The onset of action following dental injections is usually 2 to 10 minutes and anesthesia may last two or three times longer than lidocaine and mepivacaine for dental use, in many patients up to 7 hours. The duration of anesthetic effect is prolonged by the addition of epinephrine 1:200,000. It has also been noted that there is a period of analgesia that persists after the return of sensation, during which time the need for strong analgesic is reduced. -

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice. -

Cocaine Intoxication and Hypertension
THE EMCREG-INTERNATIONAL CONSENSUS PANEL RECOMMENDATIONS Cocaine Intoxication and Hypertension Judd E. Hollander, MD From the Department of Emergency Medicine, University of Pennsylvania, Philadelphia, PA. 0196-0644/$-see front matter Copyright © 2008 by the American College of Emergency Physicians. doi:10.1016/j.annemergmed.2007.11.008 [Ann Emerg Med. 2008;51:S18-S20.] with cocaine intoxication is analogous to that of the patient with hypertension: the treatment should be geared toward the Cocaine toxicity has been reported in virtually all organ patient’s presenting complaint. systems. Many of the adverse effects of cocaine are similar to When the medical history is clear and symptoms are mild, adverse events that can result from either acute hypertensive laboratory evaluation is usually unnecessary. In contrast, if the crisis or chronic effects of hypertension. Recognizing when the patient has severe toxicity, evaluation should be geared toward specific disease requires treatment separate from cocaine toxicity the presenting complaint. Laboratory evaluation may include a is paramount to the treatment of patients with cocaine CBC count; determination of electrolyte, glucose, blood urea intoxication. nitrogen, creatine kinase, and creatinine levels; arterial blood The initial physiologic effect of cocaine on the cardiovascular gas analysis; urinalysis; and cardiac marker determinations. system is a transient bradycardia as a result of stimulation of the Increased creatine kinase level occurs with rhabdomyolysis. vagal nuclei. Tachycardia typically ensues, predominantly from Cardiac markers are increased in myocardial infarction. Cardiac increased central sympathetic stimulation. Cocaine has a troponin I is preferred to identify acute myocardial13 infarction. cardiostimulatory effect through sensitization to epinephrine A chest radiograph should be obtained in patients with and norepinephrine. -
Atopic Children and Use of Prescribed Medication: a Comprehensive Study in General Practice
RESEARCH ARTICLE Atopic children and use of prescribed medication: A comprehensive study in general practice David H. J. Pols1*, Mark M. J. Nielen2, Arthur M. Bohnen1, Joke C. Korevaar2, Patrick J. E. Bindels1 1 Department of General Practice, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 2 NIVEL, Netherlands Institute for Health Services Research, Utrecht, The Netherlands a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 Purpose A comprehensive and representative nationwide general practice database was explored to study associations between atopic disorders and prescribed medication in children. OPEN ACCESS Citation: Pols DHJ, Nielen MMJ, Bohnen AM, Korevaar JC, Bindels PJE (2017) Atopic children Method and use of prescribed medication: A All children aged 0±18 years listed in the NIVEL Primary Care Database in 2014 were comprehensive study in general practice. PLoS ONE 12(8): e0182664. https://doi.org/10.1371/ selected. Atopic children with atopic eczema, asthma and allergic rhinitis (AR) were journal.pone.0182664 matched with controls (not diagnosed with any of these disorders) within the same general Editor: Anthony Peter Sampson, University of practice on age and gender. Logistic regression analyses were performed to study the differ- Southampton School of Medicine, UNITED ences in prescribed medication between both groups by calculating odds ratios (OR); 93 dif- KINGDOM ferent medication groups were studied. Received: March 24, 2017 Accepted: July 13, 2017 Results Published: August 24, 2017 A total of 45,964 children with at least one atopic disorder were identified and matched with Copyright: © 2017 Pols et al. This is an open controls. Disorder-specific prescriptions seem to reflect evidence-based medicine guide- access article distributed under the terms of the lines for atopic eczema, asthma and AR. -

Summary of Product Characteristics
Summary of Product Characteristics 1. NAME OF THE MEDICINAL PRODUCT /…/ 2 mg/ml solution for injection /…/ 7.5 mg/ml solution for injection /…/ 10 mg/ml solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION /…/ 2 mg/ml solution for injection: 1 ml contains 2.12 mg ropivacaine hydrochloride monohydrate, equivalent to 2 mg of ropivacaine hydrochloride. Excipient with know effect: sodium 3.6 mg/ml 10 ml amp. contains 21.2 mg ropivacaine hydrochloride monohydrate, equivalent to 20 mg of ropivacaine hydrochloride. 20 ml amp. contains 42.3 mg ropivacaine hydrochloride monohydrate, equivalent to 40 mg of ropivacaine hydrochloride. /…/ 7.5 mg/ml solution for injection: 1 ml contains 7.94 mg ropivacaine hydrochloride monohydrate, equivalent to 7.5 mg of ropivacaine hydrochloride. Excipient with known effect: sodium 3.0 mg/ml 10 ml amp. contains 79.4 mg ropivacaine hydrochloride monohydrate, equivalent to 75 mg of ropivacaine hydrochloride. 20 ml amp. contains 158.7 mg ropivacaine hydrochloride monohydrate, equivalent to 150 mg of ropivacaine hydrochloride. /…/ 10 mg/ml solution for injection: 1 ml contains 10.58 mg ropivacaine hydrochloride monohydrate, equivalent to 10 mg of ropivacaine hydrochloride. Excipient with known effect: sodium 2.9 mg/ml 10 ml amp. contains 105.8 mg ropivacaine hydrochloride monohydrate, equivalent to 100 mg of ropivacaine hydrochloride. 20 ml amp. contains 211.6 mg ropivacaine hydrochloride monohydrate, equivalent to 200 mg of ropivacaine hydrochloride. For thefull list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection Clear, colourless solution with a pH of 3.5 – 6 and an osmolality of 280 – 320 mosmol/kg. -
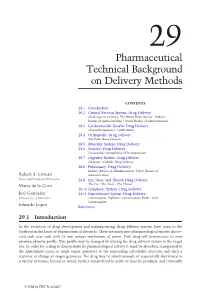
Biomedical Technology and Devices Handbook
1140_bookreps.fm Page 1 Tuesday, July 15, 2003 9:47 AM 29 Pharmaceutical Technical Background on Delivery Methods CONTENTS 29.1 Introduction 29.2 Central Nervous System: Drug Delivery Challenges to Delivery: The Blood Brain Barrier • Indirect Routes of Administration • Direct Routes of Administration 29.3 Cardiovascular System: Drug Delivery Chronotherapeutics • Grafts/Stents 29.4 Orthopedic: Drug Delivery Metabolic Bone Diseases 29.5 Muscular System: Drug Delivery 29.6 Sensory: Drug Delivery Ultrasound • Iontophoresis/Electroporation 29.7 Digestive System: Drug Delivery GI Stents • Colonic Drug Delivery 29.8 Pulmonary: Drug Delivery Indirect Routes of Administration • Direct Routes of Robert S. Litman Administration Nova Southeastern University 29.9 Ear, Nose, and Throat: Drug Delivery Maria de la Cova The Ear • The Nose • The Throat 29.10 Lymphatic System: Drug Delivery Icel Gonzalez 29.11 Reproductive System: Drug Delivery University of Memphis Contraceptive Implants • Contraceptive Patch • Male Contraceptive Eduardo Lopez References 29.1 Introduction In the evolution of drug development and manufacturing, drug delivery systems have risen to the forefront in the latest of pharmaceutical advances. There are many new pharmacological entities discov- ered each year, each with its own unique mechanism of action. Each drug will demonstrate its own pharmacokinetic profile. This profile may be changed by altering the drug delivery system to the target site. In order for a drug to demonstrate its pharmacological activity it must be absorbed, transported to the appropriate tissue or target organ, penetrate to the responding subcellular structure, and elicit a response or change an ongoing process. The drug may be simultaneously or sequentially distributed to a variety of tissues, bound or stored, further metabolized to active or inactive products, and eventually © 2004 by CRC Press LLC 1140_bookreps.fm Page 2 Tuesday, July 15, 2003 9:47 AM 29-2 Biomedical Technology and Devices Handbook excreted from the body. -

A New Technique of Epidural and Intrathecal Catheterization to Evaluate Pharmacokinetics of Epidural Administration in Dogs: a Prospective Study
A new technique of epidural and intrathecal catheterization to evaluate pharmacokinetics of epidural administration in dogs: a prospective study Myoung Hoon Kong Korea University Guro Hospital Sang Sik Choi ( [email protected] ) Korea University Guro Hospital https://orcid.org/0000-0002-0260-9886 Jung Eun Kim Korea University Guro Hospital Mi Kyoung Lee Korea University Guro Hospital Chung Hun Lee Korea University Guro Hospital Yeon Joo Lee Korea University Guro Hospital Technical advance Keywords: Canine; Epidural catheterization; Epidural drug administration; Intrathecal catheterization; Yaksh’s model Posted Date: April 19th, 2019 DOI: https://doi.org/10.21203/rs.2.9257/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/10 Abstract Background: Compared to the conventional oral or intravenous drug administration, epidural administration of drugs has signicantly higher ecacy and safety. Experimental research on animals should be performed before applying to humans. Unlike the existing canine model, we describe a new and alternative technique of epidural and intrathecal catheterization to investigate the ecacy and safety of epidural drug administration in dogs. Methods: Twelve adult dogs were used in this study. The procedures were performed with dogs in sternal recumbency under deep sedation. Epidural catheterization was performed at the T1–T2 intervertebral space with C-arm uoroscopy guidance. After conrming loss of resistance, a exible epidural catheter was passed cranially to the C2–C3 level. Intrathecal catheterization was performed through the cisterna magna with the neck slightly exed. An 18-gauge Tuohy needle was inserted into the subarachnoid space through the atlanto-occipital space. -

EXPAREL Briefing Document: 14-15 February 2018
EXPAREL Briefing Document: 14-15 February 2018 FDA Advisory Committee Meeting FDA ADVISORY COMMITTEE MEETING BRIEFING DOCUMENT ® EXPAREL (bupivacaine liposome injectable suspension) MEETING OF THE ANESTHETIC AND ANALGESIC DRUG PRODUCTS ADVISORY COMMITTEE MEETING DATE: 14-15 February 2018 AVAILABLE FOR PUBLIC RELEASE EXPAREL Briefing Document: 14-15 February 2018 FDA Advisory Committee Meeting TABLE OF CONTENTS Table of Contents ............................................................................................................................ 2 List of Tables .................................................................................................................................. 5 List of Figures ................................................................................................................................. 6 1 Executive Summary ................................................................................................................ 9 1.1 Rationale for the Use of EXPAREL as a Nerve Block .................................................. 10 1.2 Regulatory History ......................................................................................................... 12 1.3 Clinical Pharmacology ................................................................................................... 13 1.4 Efficacy Findings ........................................................................................................... 14 1.5 Safety Findings .............................................................................................................. -

Redalyc.Antinociceptive Effects of Epidural Tramadol Administration In
Acta Scientiae Veterinariae ISSN: 1678-0345 [email protected] Universidade Federal do Rio Grande do Sul Brasil Côrrea Natalini, Cláudio; da Silva Polydoro, Alexandre; Crosignani, Nadia Antinociceptive effects of epidural tramadol administration in dogs as an analgesic technique for experimental stifle surgery Acta Scientiae Veterinariae, vol. 35, núm. 2, 2007, pp. 189-195 Universidade Federal do Rio Grande do Sul Porto Alegre, Brasil Available in: http://www.redalyc.org/articulo.oa?id=289021845008 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Acta Scientiae Veterinariae. 35(2): 189-195, 2007. ORIGINAL ARTICLE ISSN 1678-0345 (Print) Pub. 725 ISSN 1679-9216 (Online) Antinociceptive effects of epidural tramadol administration in dogs as an analgesic technique for experimental stifle surgery Efeitos antinociceptivos da administração epidural de tramadol em cães como técnica analgésica para cirurgia experimental do joelho Cláudio Côrrea Natalini1, Alexandre da Silva Polydoro2 & Nadia Crosignani2 ABSTRACT Tramadol is a centrally acting analgesic with µ-opioid and monoaminergic agonist effect. Ten healthy adult dogs were studied (mean ± SEM body weight 17.3 ± 3.8 kg), premedicated with acepromazine (0.05 mg/kg, IM), induced with thiopental (10 mg/kg, IV) and maintained under anesthesia with halothane in oxygen. Twenty minutes after starting halothane anesthesia, tramadol (1.0 mg/kg in 0.22 ml/kg of sterile water) was administered epidurally at the lumbo-sacral space. Surgery began 15 minutes later.