Diphenhydramine (Systemic) Epinephrine (Systemic)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -
For Personal Use Only
SedatiWITH ANTIi ® Dowden Health Media CopyrightFor personal use only Initiate the antipsychotic at a reasonable, not overly high dose, then use a nonantipsychotic to help control insomnia, anxiety, and agitation For mass reproduction, content licensing and permissions contact Dowden Health Media. pSYCHIATRY i PSYCHOTICSon edation is a frequent side effect of antipsychot- ics, especially at relatively high doses. Antipsy- S chotics’ sedative effects can reduce agitation in acute psychosis and promote sleep in insomnia, but Manage, don’t long-term sedation may: • interfere with schizophrenia patients’ efforts to go accept adverse to work or school or engage in normal socialization • prevent improvement from psychosocial training, psychiatric rehabilitation, and other treatments. ‘calming’ eff ect This article discusses how to manage acute psycho- sis without oversedation and ways to address persistent sedation and chronic insomnia with less-sedating anti- Del D. Miller, PharmD, MD Professor of psychiatry psychotics or adjunctive medications. University of Iowa Carver College of Medicine Iowa City Neurobiology or psychopharmacology? Many patients experience only mild, transient som- nolence at the beginning of antipsychotic treatment, and most develop some tolerance to the sedating ef- fects with continued administration. Others may have persistent daytime sedation that interferes with nor- mal functioning. Sedation is especially common in elderly patients re- ceiving antipsychotics. Compared with younger patients, older patients receiving -

The Case of Ketamine Allergy
CASE REPORT The Case of Ketamine Allergy William Bylund, MD Department of Emergency Medicine, Naval Medical Center Portsmouth, Portsmouth, Virginia Liam Delahanty, MD Maxwell Cooper, MD Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 3, 2017; Revision received June 29, 2017; Accepted July 11, 2017 Electronically published October 3, 2017 Full text available through open access at http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.2017.7.34405 Ketamine is often used for pediatric procedural sedation due to low rates of complications, with allergic reactions being rare. Immediately following intramuscular (IM) ketamine administration, a three-year-old female rapidly developed facial edema and diffuse urticarial rash, with associated wheezing and oxygen desaturation. Symptoms resolved following treatment with epinephrine, dexamethasone and diphenhydramine. This case presents a clinical reaction to ketamine consistent with anaphylaxis due to histamine release, but it is uncertain whether this was immunoglobulin E mediated. This is the only case reported to date of allergic reaction to IM ketamine, without co- administration of other agents. [Clin Pract Cases Emerg Med.2017;1(4):323–325.] INTRODUCTION cardiac monitor, end tidal CO2 (ETCO2) and pulse oximetry Ketamine is a common medication, used in isolation as well (POx), in addition to being placed on two liters nasal cannula as with other agents, for pediatric sedation in the emergency (NC). No intravenous (IV) access was obtained prior to sedation. department (ED). It is often turned to because of its efficacy, ease Seventy milligrams (4.4mg/kg) of ketamine was administered IM of use, and favorable safety profile. Common side effects of into the right thigh. -

Diphenhydramine Dosage Sheet Concord Pediatrics, P.A
Diphenhydramine Dosage Sheet Concord Pediatrics, P.A. (603) 224-1929 BRAND NAMES: Benadryl INDICATIONS: Treatment of allergic reactions, nasal allergies, hives and itching. FREQUENCY: Repeat every 6 hours as needed. Don't give more than 4 times a day. DOSAGE: Determine by using the table below. Please speak with a medical provider before giving Diphenhydramine to a child under 1 year old. Child’s Dose in mg Children’s Liquid Chewable/Fastmelts Tabs/Caps/Gels Weight (lb) (12.5mg/ 5mL) 12.5mg tablets 25mg tablets *12-16 lbs 6.25 mg 2.5 mL *17-19 lbs 9.375 mg 3.75 mL *20-24 lbs 10 mg 4 mL 25-37 lbs 12.5 mg 5 mL 1 tab 38-49 lbs 18.75 mg 7.5 mL 1.5 tabs 50-69 lbs 25 mg 10 mL 2 tabs 1 tab 70-99 lbs 37.5 mg 15 mL 3 tabs 1.5 tabs >100 lbs 50 mg 20 mL 4 tabs 2 tabs Table Notes: *AGE LIMIT: For allergies, don't use under 1 year of age (Reason: it's a sedative). For colds, not recommended at any age (Reason: no proven benefits) and should be avoided if under 4 years old. Avoid multi-ingredient products in children under 6 years of age (Reason: FDA recommendations 10/2008). MEASURING the DOSAGE: Syringes and droppers are more accurate than teaspoons. If possible, use the syringe or dropper that comes with the medicine. If not, medicine syringes are available at pharmacies. Regular spoons are not reliable. ADULT DOSAGE: 50 mg Why use Diphenhydramine? Antihistamines can be used to treat your child’s runny nose, itchy eyes, and sneezing due to allergies. -

Cocaine Intoxication and Hypertension
THE EMCREG-INTERNATIONAL CONSENSUS PANEL RECOMMENDATIONS Cocaine Intoxication and Hypertension Judd E. Hollander, MD From the Department of Emergency Medicine, University of Pennsylvania, Philadelphia, PA. 0196-0644/$-see front matter Copyright © 2008 by the American College of Emergency Physicians. doi:10.1016/j.annemergmed.2007.11.008 [Ann Emerg Med. 2008;51:S18-S20.] with cocaine intoxication is analogous to that of the patient with hypertension: the treatment should be geared toward the Cocaine toxicity has been reported in virtually all organ patient’s presenting complaint. systems. Many of the adverse effects of cocaine are similar to When the medical history is clear and symptoms are mild, adverse events that can result from either acute hypertensive laboratory evaluation is usually unnecessary. In contrast, if the crisis or chronic effects of hypertension. Recognizing when the patient has severe toxicity, evaluation should be geared toward specific disease requires treatment separate from cocaine toxicity the presenting complaint. Laboratory evaluation may include a is paramount to the treatment of patients with cocaine CBC count; determination of electrolyte, glucose, blood urea intoxication. nitrogen, creatine kinase, and creatinine levels; arterial blood The initial physiologic effect of cocaine on the cardiovascular gas analysis; urinalysis; and cardiac marker determinations. system is a transient bradycardia as a result of stimulation of the Increased creatine kinase level occurs with rhabdomyolysis. vagal nuclei. Tachycardia typically ensues, predominantly from Cardiac markers are increased in myocardial infarction. Cardiac increased central sympathetic stimulation. Cocaine has a troponin I is preferred to identify acute myocardial13 infarction. cardiostimulatory effect through sensitization to epinephrine A chest radiograph should be obtained in patients with and norepinephrine. -

Chronic Pain Management Toolkit
Chronic Pain Management Urine Drug Testing Toolkit Screening (see chart on next page) Most guidelines recommend screening patients to determine risks of drug misuse and abuse and to mitigate those risks as much as possible. Unfortunately, there are no risk assessment tools that have been validated in multiple settings and populations. Screening is typically based on risk factors that can be identified through a thorough patient history, the use of prescription drug monitoring programs (PDMPs), the opioid risk tool (provided in this toolkit), and, on occasion, drug screening. However, it is important to standardize testing as cited risk factors (e.g. sociodemographic factors, psychological comorbidity, substance use disorders, etc.) might unfairly impact certain vulnerable populations. Involvement of the whole health care team and full disclosure and discussion of the screening protocol with patients is central to providing patient-centered and comprehensive pain management. Prior to drug testing, physicians should inform the patient of the reason(s) for testing, how often they will be tested, and what the results might mean. This gives patients an opportunity to disclose any additional drug or substance use which may help with identification of false positives and appropriate interpretation of test results. Physicians must understand the limitations of the urine and confirmatory tests available, including what substances are detected by a particular test, and the reasons for false-positive and false-negative tests. Changes in prescribing for a particular patient should not be based on the result of one abnormal screening test, but should only occur after looking at all available monitoring tools as well as repeating the drug screen with the most specific test available. -
Atopic Children and Use of Prescribed Medication: a Comprehensive Study in General Practice
RESEARCH ARTICLE Atopic children and use of prescribed medication: A comprehensive study in general practice David H. J. Pols1*, Mark M. J. Nielen2, Arthur M. Bohnen1, Joke C. Korevaar2, Patrick J. E. Bindels1 1 Department of General Practice, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 2 NIVEL, Netherlands Institute for Health Services Research, Utrecht, The Netherlands a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 Purpose A comprehensive and representative nationwide general practice database was explored to study associations between atopic disorders and prescribed medication in children. OPEN ACCESS Citation: Pols DHJ, Nielen MMJ, Bohnen AM, Korevaar JC, Bindels PJE (2017) Atopic children Method and use of prescribed medication: A All children aged 0±18 years listed in the NIVEL Primary Care Database in 2014 were comprehensive study in general practice. PLoS ONE 12(8): e0182664. https://doi.org/10.1371/ selected. Atopic children with atopic eczema, asthma and allergic rhinitis (AR) were journal.pone.0182664 matched with controls (not diagnosed with any of these disorders) within the same general Editor: Anthony Peter Sampson, University of practice on age and gender. Logistic regression analyses were performed to study the differ- Southampton School of Medicine, UNITED ences in prescribed medication between both groups by calculating odds ratios (OR); 93 dif- KINGDOM ferent medication groups were studied. Received: March 24, 2017 Accepted: July 13, 2017 Results Published: August 24, 2017 A total of 45,964 children with at least one atopic disorder were identified and matched with Copyright: © 2017 Pols et al. This is an open controls. Disorder-specific prescriptions seem to reflect evidence-based medicine guide- access article distributed under the terms of the lines for atopic eczema, asthma and AR. -

Children with Respiratory Disorders: Asthma and Allergies
Oral Health Fact Sheet for Dental Professionals Children with Respiratory Disorders: Asthma and Allergies Asthma is a chronic respiratory disease associated with airway obstruction, with recurrent attacks of paroxysmal dyspnea, and wheezing due to spasmodic contraction of the bronchi. (ICD 9 code 493.2) Allergy is a hypersensitivity to an agent caused by an immunologic response to an initial exposure. (ICD 9 code 995.3) Prevalence • Asthma affects 9.3% of the population, higher in females and African-Americans Manifestations Clinical • Constriction of bronchi, coughing, wheezing, chest tightness, and shortness of breath Oral • Increased caries risk, enamel defects • Increased gingivitis and periodontal disease risk; and more calculus • Higher rates of malocclusion and increased: overjet, overbite, posterior crossbite; high palatal vault • Oral candidiasis, xerostomia, decreased salivary flow rate and salivary pH Other Potential Disorders/Concerns • none Management Medication SYMPTOM MEDICATION SIDE EFFECTS Breathing difficulties A. Bronchodilators (Β2-agonists) A. Oral candidiasis, xerostomia, decreased salivary flow rate B. Corticosteroids B. Oral candidiasis, dental caries C. Antihistamines C. Xerostomia D. Decongestants D. Xerostomia Sedation • Hydroxyzine and benzodiazepines recommended; avoid narcotics and barbiturates due to their histamine releasing properties → bronchospasm and potentiated allergic response. Intravenous sedation • Use extreme caution due to limited control of the airway. Avoid • Aspirin, other salicylates and NSAIDS (due to allergies) may provoke a severe exacerbation of bronchoconstriction; use acetaminophen. Behavioral Stress-management techniques; may use nitrous oxide in mild to moderate asthmatics after medical consultation. Anxiety can cause acute exacerbation. Children with Respiratory Disorders: Asthma and Allergies continued Dental Treatment and Prevention • Assess child’s risk of acute exacerbation/anaphylaxis during dental treatment prior to examination. -
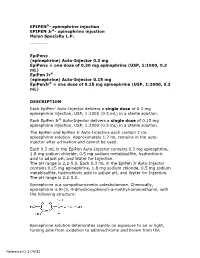
Epipen Injection Label
EPIPEN®- epinephrine injection EPIPEN Jr®- epinephrine injection Mylan Specialty L.P. ---------- EpiPen® (epinephrine) Auto-Injector 0.3 mg EpiPen® = one dose of 0.30 mg epinephrine (USP, 1:1000, 0.3 mL) EpiPen Jr® (epinephrine) Auto-Injector 0.15 mg EpiPenJr® = one dose of 0.15 mg epinephrine (USP, 1:2000, 0.3 mL) DESCRIPTION Each EpiPen® Auto-Injector delivers a single dose of 0.3 mg epinephrine injection, USP, 1:1000 (0.3 mL) in a sterile solution. Each EpiPen Jr® Auto-Injector delivers a single dose of 0.15 mg epinephrine injection, USP, 1:2000 (0.3 mL) in a sterile solution. The EpiPen and EpiPen Jr Auto-Injectors each contain 2 mL epinephrine solution. Approximately 1.7 mL remains in the auto- injector after activation and cannot be used. Each 0.3 mL in the EpiPen Auto-Injector contains 0.3 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Each 0.3 mL in the EpiPen Jr Auto-Injector contains 0.15 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Epinephrine is a sympathomimetic catecholamine. Chemically, epinephrine is B-(3, 4-dihydroxyphenyl)-a-methyl-aminoethanol, with the following structure: Epinephrine solution deteriorates rapidly on exposure to air or light, turning pink from oxidation to adrenochrome and brown from the Reference ID: 3176782 formation of melanin. -

Ketamine and Serotonin Syndrome: a Case Report
Residents’ Voices Ketamine and serotonin syndrome: A case report Clay Gueits, MD, and Martin Witkin, DO ong utilized as a rapid anesthetic, ket- with haloperidol (dose unknown) with amine has been increasingly used in reportedly good effect. On Day 7, she was Lsub-anesthetic doses for several psy- discharged home. chiatric indications, including depression, Upon returning home, she experienced suicidality, and chronic pain. Recently, persistent altered mental status. Her signifi- an intranasal form of esketamine—the cant other brought her to our hospital for fur- S-enantiomer of ketamine—was FDA- ther workup. Ms. O’s body temperature was Clay Gueits, MD approved for treatment-resistant depression. 37.6°C, and she was diaphoretic. Her blood Previously, researchers believed ketamine pressure was 154/100 mm Hg, and her heart mediated its analgesic and psychotropic rate was 125 bpm. On physical examination, effects solely via N-methyl-d-aspartate she had 4+ patellar and Achilles reflexes (NMDA) receptor antagonism, but emerg- with left ankle clonus and crossed adductors. ing research has described a seemingly more Her mental status exam showed increased complex receptor profile.1 One such ancillary latency of thought and speech, with bizarre pharmacologic mechanism is occupation of affect as evidenced by illogical mannerisms Martin Witkin, DO the serotonin receptor.1,2 However, there and appearance. She said she was “not feel- is sparse literature describing the possible ing myself” and would stare at walls for pro- Dr. Gueits is a PGY-2 Psychiatry extent of ketamine’s involvement in sero- longed periods of time, appearing internally Resident, Department of Psychiatry, tonin syndrome.3 Here, we describe a case preoccupied and confused. -
Patients on Beta-Blockers
Systemic Allergic & Immunoglobulin Disorders Bryan L. Martin, DO, MMAS, FACAAI, FAAAAI, FACP, FACOI Emeritus Professor of Medicine and Pediatrics President, American College of Allergy, Asthma & Immunology Disclosures . None 2 Objectives . Pass the boards! . Recognize anaphylaxis and understand the new guidelines for the treatment of anaphylaxis . Compare and contrast anaphylactic and anaphylactoid reactions 3 The Patient . 45 year old woman goes to lunch with her friends . While eating she develops GI upset, dizziness, shortness of breath and hives . Her friends drive her to your nearby clinic Initial Evaluation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating a shrimp salad. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Anaphylaxis presentation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating lunch. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Initial Response to anaphylaxis . -

Xylocaine® (Lidocaine Hcl and Epinephrine Injection, USP) for Infiltration and Nerve Block Rx Only
XYLOCAINE MPF- lidocaine hydrochloride injection, solution XYLOCAINE - lidocaine hydrochloride injection, solution XYLOCAINE MPF- lidocaine hydrochloride,epinephrine bitartrate injection, solution XYLOCAINE - lidocaine hydrochloride,epinephrine bitartrate injection, solution Fresenius Kabi USA, LLC ---------- Xylocaine® (lidocaine HCl Injection, USP) Xylocaine® (lidocaine HCl and epinephrine Injection, USP) For Infiltration and Nerve Block Rx only DESCRIPTION Xylocaine (lidocaine HCl) Injections are sterile, nonpyrogenic, aqueous solutions that contain a local anesthetic agent with or without epinephrine and are administered parenterally by injection. See INDICATIONS AND USAGE section for specific uses. Xylocaine solutions contain lidocaine HCl, which is chemically designated as acetamide, 2- (diethylamino)-N-(2,6-dimethylphenyl)-, monohydrochloride and has the molecular wt. 270.8. Lidocaine HCl (C 14H 22N 2O • HCl) has the following structural formula: Epinephrine is (-) -3, 4-Dihydroxy-α-[(methylamino) methyl] benzyl alcohol and has the molecular wt. 183.21. Epinephrine (C 9H 13NO 3) has the following structural formula: Dosage forms listed as Xylocaine-MPF indicate single dose solutions that are Methyl Paraben Free (MPF). Xylocaine MPF is a sterile, nonpyrogenic, isotonic solution containing sodium chloride. Xylocaine in multiple dose vials: Each mL also contains 1 mg methylparaben as antiseptic preservative. The pH of these solutions is adjusted to approximately 6.5 (5.0 to 7.0) with sodium hydroxide and/or hydrochloric acid. Xylocaine MPF with Epinephrine is a sterile, nonpyrogenic, isotonic solution containing sodium chloride. Each mL contains lidocaine hydrochloride and epinephrine, with 0.5 mg sodium metabisulfite as an antioxidant and 0.2 mg citric acid as a stabilizer. Xylocaine with Epinephrine in multiple dose as an antioxidant and 0.2 mg citric acid as a stabilizer.