Dnmt3a Haploinsufficiency Transforms Flt3-ITD Myeloproliferative Disease Into A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Characterization of BRCA1-Deficient Premalignant Tissues and Cancers Identifies Plekha5 As a Tumor Metastasis Suppressor
ARTICLE https://doi.org/10.1038/s41467-020-18637-9 OPEN Characterization of BRCA1-deficient premalignant tissues and cancers identifies Plekha5 as a tumor metastasis suppressor Jianlin Liu1,2, Ragini Adhav1,2, Kai Miao1,2, Sek Man Su1,2, Lihua Mo1,2, Un In Chan1,2, Xin Zhang1,2, Jun Xu1,2, Jianjie Li1,2, Xiaodong Shu1,2, Jianming Zeng 1,2, Xu Zhang1,2, Xueying Lyu1,2, Lakhansing Pardeshi1,3, ✉ ✉ Kaeling Tan1,3, Heng Sun1,2, Koon Ho Wong 1,3, Chuxia Deng 1,2 & Xiaoling Xu 1,2 1234567890():,; Single-cell whole-exome sequencing (scWES) is a powerful approach for deciphering intra- tumor heterogeneity and identifying cancer drivers. So far, however, simultaneous analysis of single nucleotide variants (SNVs) and copy number variations (CNVs) of a single cell has been challenging. By analyzing SNVs and CNVs simultaneously in bulk and single cells of premalignant tissues and tumors from mouse and human BRCA1-associated breast cancers, we discover an evolution process through which the tumors initiate from cells with SNVs affecting driver genes in the premalignant stage and malignantly progress later via CNVs acquired in chromosome regions with cancer driver genes. These events occur randomly and hit many putative cancer drivers besides p53 to generate unique genetic and pathological features for each tumor. Upon this, we finally identify a tumor metastasis suppressor Plekha5, whose deficiency promotes cancer metastasis to the liver and/or lung. 1 Cancer Centre, Faculty of Health Sciences, University of Macau, Macau, SAR, China. 2 Centre for Precision Medicine Research and Training, Faculty of Health Sciences, University of Macau, Macau, SAR, China. -

Table S1 the Four Gene Sets Derived from Gene Expression Profiles of Escs and Differentiated Cells
Table S1 The four gene sets derived from gene expression profiles of ESCs and differentiated cells Uniform High Uniform Low ES Up ES Down EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol 269261 Rpl12 11354 Abpa 68239 Krt42 15132 Hbb-bh1 67891 Rpl4 11537 Cfd 26380 Esrrb 15126 Hba-x 55949 Eef1b2 11698 Ambn 73703 Dppa2 15111 Hand2 18148 Npm1 11730 Ang3 67374 Jam2 65255 Asb4 67427 Rps20 11731 Ang2 22702 Zfp42 17292 Mesp1 15481 Hspa8 11807 Apoa2 58865 Tdh 19737 Rgs5 100041686 LOC100041686 11814 Apoc3 26388 Ifi202b 225518 Prdm6 11983 Atpif1 11945 Atp4b 11614 Nr0b1 20378 Frzb 19241 Tmsb4x 12007 Azgp1 76815 Calcoco2 12767 Cxcr4 20116 Rps8 12044 Bcl2a1a 219132 D14Ertd668e 103889 Hoxb2 20103 Rps5 12047 Bcl2a1d 381411 Gm1967 17701 Msx1 14694 Gnb2l1 12049 Bcl2l10 20899 Stra8 23796 Aplnr 19941 Rpl26 12096 Bglap1 78625 1700061G19Rik 12627 Cfc1 12070 Ngfrap1 12097 Bglap2 21816 Tgm1 12622 Cer1 19989 Rpl7 12267 C3ar1 67405 Nts 21385 Tbx2 19896 Rpl10a 12279 C9 435337 EG435337 56720 Tdo2 20044 Rps14 12391 Cav3 545913 Zscan4d 16869 Lhx1 19175 Psmb6 12409 Cbr2 244448 Triml1 22253 Unc5c 22627 Ywhae 12477 Ctla4 69134 2200001I15Rik 14174 Fgf3 19951 Rpl32 12523 Cd84 66065 Hsd17b14 16542 Kdr 66152 1110020P15Rik 12524 Cd86 81879 Tcfcp2l1 15122 Hba-a1 66489 Rpl35 12640 Cga 17907 Mylpf 15414 Hoxb6 15519 Hsp90aa1 12642 Ch25h 26424 Nr5a2 210530 Leprel1 66483 Rpl36al 12655 Chi3l3 83560 Tex14 12338 Capn6 27370 Rps26 12796 Camp 17450 Morc1 20671 Sox17 66576 Uqcrh 12869 Cox8b 79455 Pdcl2 20613 Snai1 22154 Tubb5 12959 Cryba4 231821 Centa1 17897 -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Clinical Utility of Recently Identified Diagnostic, Prognostic, And
Modern Pathology (2017) 30, 1338–1366 1338 © 2017 USCAP, Inc All rights reserved 0893-3952/17 $32.00 Clinical utility of recently identified diagnostic, prognostic, and predictive molecular biomarkers in mature B-cell neoplasms Arantza Onaindia1, L Jeffrey Medeiros2 and Keyur P Patel2 1Instituto de Investigacion Marques de Valdecilla (IDIVAL)/Hospital Universitario Marques de Valdecilla, Santander, Spain and 2Department of Hematopathology, MD Anderson Cancer Center, Houston, TX, USA Genomic profiling studies have provided new insights into the pathogenesis of mature B-cell neoplasms and have identified markers with prognostic impact. Recurrent mutations in tumor-suppressor genes (TP53, BIRC3, ATM), and common signaling pathways, such as the B-cell receptor (CD79A, CD79B, CARD11, TCF3, ID3), Toll- like receptor (MYD88), NOTCH (NOTCH1/2), nuclear factor-κB, and mitogen activated kinase signaling, have been identified in B-cell neoplasms. Chronic lymphocytic leukemia/small lymphocytic lymphoma, diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, Burkitt lymphoma, Waldenström macroglobulinemia, hairy cell leukemia, and marginal zone lymphomas of splenic, nodal, and extranodal types represent examples of B-cell neoplasms in which novel molecular biomarkers have been discovered in recent years. In addition, ongoing retrospective correlative and prospective outcome studies have resulted in an enhanced understanding of the clinical utility of novel biomarkers. This progress is reflected in the 2016 update of the World Health Organization classification of lymphoid neoplasms, which lists as many as 41 mature B-cell neoplasms (including provisional categories). Consequently, molecular genetic studies are increasingly being applied for the clinical workup of many of these neoplasms. In this review, we focus on the diagnostic, prognostic, and/or therapeutic utility of molecular biomarkers in mature B-cell neoplasms. -
Supplementary File 2A Revised
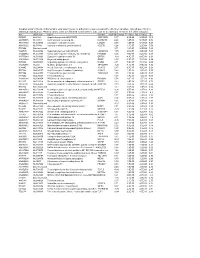
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -

Gene List HTG Edgeseq Immuno-Oncology Assay
Gene List HTG EdgeSeq Immuno-Oncology Assay Adhesion ADGRE5 CLEC4A CLEC7A IBSP ICAM4 ITGA5 ITGB1 L1CAM MBL2 SELE ALCAM CLEC4C DST ICAM1 ITGA1 ITGA6 ITGB2 LGALS1 MUC1 SVIL CDH1 CLEC5A EPCAM ICAM2 ITGA2 ITGAL ITGB3 LGALS3 NCAM1 THBS1 CDH5 CLEC6A FN1 ICAM3 ITGA4 ITGAM ITGB4 LGALS9 PVR THY1 Apoptosis APAF1 BCL2 BID CARD11 CASP10 CASP8 FADD NOD1 SSX1 TP53 TRAF3 BCL10 BCL2L1 BIRC5 CASP1 CASP3 DDX58 NLRP3 NOD2 TIMP1 TRAF2 TRAF6 B-Cell Function BLNK BTLA CD22 CD79A FAS FCER2 IKBKG PAX5 SLAMF1 SLAMF7 SPN BTK CD19 CD24 EBF4 FASLG IKBKB MS4A1 RAG1 SLAMF6 SPI1 Cell Cycle ABL1 ATF1 ATM BATF CCND1 CDK1 CDKN1B NCL RELA SSX1 TBX21 TP53 ABL2 ATF2 AXL BAX CCND3 CDKN1A EGR1 REL RELB TBK1 TIMP1 TTK Cell Signaling ADORA2A DUSP4 HES1 IGF2R LYN MAPK1 MUC1 NOTCH1 RIPK2 SMAD3 STAT5B AKT3 DUSP6 HES5 IKZF1 MAF MAPK11 MYC PIK3CD RNF4 SOCS1 STAT6 BCL6 ELK1 HEY1 IKZF2 MAP2K1 MAPK14 NFATC1 PIK3CG RORC SOCS3 SYK CEBPB EP300 HEY2 IKZF3 MAP2K2 MAPK3 NFATC3 POU2F2 RUNX1 SPINK5 TAL1 CIITA ETS1 HEYL JAK1 MAP2K4 MAPK8 NFATC4 PRKCD RUNX3 STAT1 TCF7 CREB1 FLT3 HMGB1 JAK2 MAP2K7 MAPKAPK2 NFKB1 PRKCE S100B STAT2 TYK2 CREB5 FOS HRAS JAK3 MAP3K1 MEF2C NFKB2 PTEN SEMA4D STAT3 CREBBP GATA3 IGF1R KIT MAP3K5 MTDH NFKBIA PYCARD SMAD2 STAT4 Chemokine CCL1 CCL16 CCL20 CCL25 CCL4 CCR2 CCR7 CX3CL1 CXCL12 CXCL3 CXCR1 CXCR6 CCL11 CCL17 CCL21 CCL26 CCL5 CCR3 CCR9 CX3CR1 CXCL13 CXCL5 CXCR2 MST1R CCL13 CCL18 CCL22 CCL27 CCL7 CCR4 CCRL2 CXCL1 CXCL14 CXCL6 CXCR3 PPBP CCL14 CCL19 CCL23 CCL28 CCL8 CCR5 CKLF CXCL10 CXCL16 CXCL8 CXCR4 XCL2 CCL15 CCL2 CCL24 CCL3 CCR1 CCR6 CMKLR1 CXCL11 CXCL2 CXCL9 CXCR5 -

The Role of Inhibitors of Differentiation Proteins ID1 and ID3 in Breast Cancer Metastasis
The role of Inhibitors of Differentiation proteins ID1 and ID3 in breast cancer metastasis Wee Siang Teo A thesis in fulfilment of the requirements for the degree of Doctor of Philosophy St Vincent’s Clinical School, Faculty of Medicine The University of New South Wales Cancer Research Program The Garvan Institute of Medical Research Sydney, Australia March, 2014 THE UNIVERSITY OF NEW SOUTH WALES Thesis/Dissertation Sheet Surname or Family name: Teo First name: Wee Siang Abbreviation for degree as given in the University calendar: PhD (Medicine) School: St Vincent’s Clinical School Faculty: Faculty of Medicine Title: The role of Inhibitors of Differentiation proteins ID1 and ID3 in breast cancer metastasis Abstract 350 words maximum: (PLEASE TYPE) Breast cancer is a leading cause of cancer death in women. While locally-confined breast cancer is generally curable, the survival of patients with metastatic breast cancer is very poor. Treatment for metastatic breast cancer is palliative not curative due to the lack of targeted therapies. Metastasis is a complex process that still remains poorly understood, thus a detailed understanding of the biological complexity that underlies breast cancer metastasis is essential in reducing the lethality of this disease. The Inhibitor of Differentiation proteins 1 and 3 (ID1/3) are transcriptional regulators that control many cell fate and developmental processes and are often deregulated in cancer. ID1/3 are required and sufficient for the metastasis of breast cancer in experimental models. However, the mechanisms by which ID1/3 mediate metastasis in breast cancer remain to be determined. Little is known about pathways regulated by ID1/3 in breast cancer as well as their functional role in the multiple steps of metastatic progression. -

Supplementary Data
SUPPLEMENTARY DATA Supplementary Figure 1. Expression of 84 genes associated with response to interferon extracted from RNA-seq data of isolated islets from subjects with recent T1D onset and islets from non-diabetic organ donors. The expression is displayed as fold up- or down regulation compared to the mean expression in the three non-diabetic controls. ©2016 American Diabetes Association. Published online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-0616/-/DC1 SUPPLEMENTARY DATA Supplementary Figure 2. Fold overexpression compared to controls of the ISGs in laser-captured T1D islets in this study (A) and what has been induced experimentally in isolated islets in other studies (B-E). The data in (B) was extracted from the RNA sequencing data of islets exposed to IL1 and IFN for 48 h, published by Eizirik et al. 2012 (1), Supporting information, Dataset S1, “table_RPKM.xls. The data in (C) and (D) were from microarray data on islets infected with Coxsackievirus B5 (C) or islets exposed to IL1 and IFN (D) for 48 h, published by Ylipaasto et al. 2005 (2), Electronic Supplementary Material 2 and 3. The data in (E) is from PCR array data of islets exposed to IFN for 6 h and published by Lind et al. 2013 (3), Supplemental file 1. In Ylipaasto et al, only genes considered significantly changed were reported and thus, in (C) and (D), genes that were not significantly changed are displayed as zero. Lind et al used an earlier version (QIAGEN, PAHS-016A) of the ISG PCR array used in this study (QIAGEN, PAHS-016ZC), and thus, only genes included in both arrays are shown in (E). -

Hematopathology
320A ANNUAL MEETING ABSTRACTS expression of ALDH1 was analyzed using mouse monoclonal ALDH1 antibody (BD Conclusions: Based on the present results we conclude that miR29ab1 ko’s have Biosciences, San Jose, CA). Correlations between ALDH1 expression and clinical and decreased hematopoietic stem cell population compared to the wild types and that histological parameters were assessed by Pearson’s Chi-square and M-L Chi-square miR29ab1 might have an important role in the maintenance of this cell population. tests. Survival curves were generated using the Kaplan-Meier method and statistical Also, miR29 genes might regulate immunity and life span, since both miR29ab1 and differences by log rank test. miR29ab1/b2c ko’s seem to have markedly decreased life spans. Results: Majority of the tumors (116, 63%) showed stromal staining only, 21 (11%) tumors showed both epithelial and stromal expression, 47 (26%) tumors did not show 1347 The Majority of Immunohistochemically BCL2 Negative FL Grade either epithelial or stromal staining. The normal salivary gland showed epithelial I/II Carry A t(14;18) with Mutations in Exon 1 of the BCL2 Gene and Can expression only. Statistical analyses did not show any correlation between tumor pattern, Be Identifi ed with the BCL2 E17 Antibody tumor size, the presence of perineural invasion and the patterns of ALDH1 expression. P Adam, R Baumann, I Bonzheim, F Fend, L Quintanilla-Martinez. Eberhard-Karls- The survival analysis using Kaplan-Meier method and log rank test did not show any University, Tubingen, Baden-Wurttemberg, Germany. signifi cant differences among the three patterns of ALDH1 expression with survival. -

Emerging Role of PYHIN Proteins As Antiviral Restriction Factors
viruses Review Emerging Role of PYHIN Proteins as Antiviral Restriction Factors Matteo Bosso and Frank Kirchhoff * Institute of Molecular Virology, Ulm University Medical Center, 89081 Ulm, Germany; [email protected] * Correspondence: frank.kirchhoff@uni-ulm.de; Tel.: +49-731-50065150 Academic Editor: Sébastien Nisole Received: 26 November 2020; Accepted: 16 December 2020; Published: 18 December 2020 Abstract: Innate immune sensors and restriction factors are cellular proteins that synergize to build an effective first line of defense against viral infections. Innate sensors are usually constitutively expressed and capable of detecting pathogen-associated molecular patterns (PAMPs) via specific pattern recognition receptors (PRRs) to stimulate the immune response. Restriction factors are frequently upregulated by interferons (IFNs) and may inhibit viral pathogens at essentially any stage of their replication cycle. Members of the Pyrin and hematopoietic interferon-inducible nuclear (HIN) domain (PYHIN) family have initially been recognized as important sensors of foreign nucleic acids and activators of the inflammasome and the IFN response. Accumulating evidence shows, however, that at least three of the four members of the human PYHIN family restrict viral pathogens independently of viral sensing and innate immune activation. In this review, we provide an overview on the role of human PYHIN proteins in the innate antiviral immune defense and on viral countermeasures. Keywords: PYHIN; DNA sensing; restriction factors; viral counteraction; immune evasion 1. Introduction Viruses strictly rely on their host cells for replication and spread. However, although viral pathogens are capable of exploiting numerous cellular factors and pathways, the cell does not provide a friendly environment. As a consequence of countless past encounters with viral pathogens, mammalian cells have evolved sensors of foreign invaders that alert and activate a large variety of antiviral effector proteins [1–5]. -

(12) Patent Application Publication (10) Pub. No.: US 2004/0225449 A1 Bevilacqua Et Al
US 20040225449A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0225449 A1 Bevilacqua et al. (43) Pub. Date: Nov. 11, 2004 (54) SYSTEMS AND METHODS FOR which is a continuation-in-part of application No. CHARACTERIZING A BIOLOGICAL 09/605,581, filed on Jun. 28, 2000, now abandoned. CONDITION OR AGENT USING SELECTED GENE EXPRESSION PROFILES (60) Provisional application No. 60/141,542, filed on Jun. 28, 1999. Provisional application No. 60/195,522, (76) Inventors: Michael P. Bevilacqua, Boulder, CO filed on Apr. 7, 2000. (US); John C. Cheronis, Conifer, CO (US); Victor Tryon, Loveland, CO Publication Classification (US); Danute M. Bankaitis-Davis, Longmont, CO (US) (51) Int. Cl." .......................... G06F 19/00; G01N 33/48; GO1N 33/50 Correspondence Address: (52) U.S. Cl. ................................................................ 702/20 Barbara J. Carter Bromberg & Sunstein LLP ABSTRACT 125 Summer Street (57) Boston, MA 02110-1618 (US) Methods are provided for evaluating a biological condition Appl. No.: 10/781,558 of a Subject using a calibrated profile data Set derived from (21) a data Set having a plurality of members, each member being (22) Filed: Feb. 17, 2004 a quantitative measure of the amount of a Subject's RNA or protein as distinct constituents in a panel of constituents. The Related U.S. Application Data biological condition may be a naturally occurring physi ological State or may be responsive to treatment of the (63) Continuation-in-part of application No. 09/821,850, Subject with one or more agents. Calibrated profile data Sets filed on Mar. 29, 2001, now Pat. -

Table S3. RAE Analysis of Well-Differentiated Liposarcoma
Table S3. RAE analysis of well-differentiated liposarcoma Model Chromosome Region start Region end Size q value freqX0* # genes Genes Amp 1 145009467 145122002 112536 0.097 21.8 2 PRKAB2,PDIA3P Amp 1 145224467 146188434 963968 0.029 23.6 10 CHD1L,BCL9,ACP6,GJA5,GJA8,GPR89B,GPR89C,PDZK1P1,RP11-94I2.2,NBPF11 Amp 1 147475854 148412469 936616 0.034 23.6 20 PPIAL4A,FCGR1A,HIST2H2BF,HIST2H3D,HIST2H2AA4,HIST2H2AA3,HIST2H3A,HIST2H3C,HIST2H4B,HIST2H4A,HIST2H2BE, HIST2H2AC,HIST2H2AB,BOLA1,SV2A,SF3B4,MTMR11,OTUD7B,VPS45,PLEKHO1 Amp 1 148582896 153398462 4815567 1.5E-05 49.1 152 PRPF3,RPRD2,TARS2,ECM1,ADAMTSL4,MCL1,ENSA,GOLPH3L,HORMAD1,CTSS,CTSK,ARNT,SETDB1,LASS2,ANXA9, FAM63A,PRUNE,BNIPL,C1orf56,CDC42SE1,MLLT11,GABPB2,SEMA6C,TNFAIP8L2,LYSMD1,SCNM1,TMOD4,VPS72, PIP5K1A,PSMD4,ZNF687,PI4KB,RFX5,SELENBP1,PSMB4,POGZ,CGN,TUFT1,SNX27,TNRC4,MRPL9,OAZ3,TDRKH,LINGO4, RORC,THEM5,THEM4,S100A10,S100A11,TCHHL1,TCHH,RPTN,HRNR,FLG,FLG2,CRNN,LCE5A,CRCT1,LCE3E,LCE3D,LCE3C,LCE3B, LCE3A,LCE2D,LCE2C,LCE2B,LCE2A,LCE4A,KPRP,LCE1F,LCE1E,LCE1D,LCE1C,LCE1B,LCE1A,SMCP,IVL,SPRR4,SPRR1A,SPRR3, SPRR1B,SPRR2D,SPRR2A,SPRR2B,SPRR2E,SPRR2F,SPRR2C,SPRR2G,LELP1,LOR,PGLYRP3,PGLYRP4,S100A9,S100A12,S100A8, S100A7A,S100A7L2,S100A7,S100A6,S100A5,S100A4,S100A3,S100A2,S100A16,S100A14,S100A13,S100A1,C1orf77,SNAPIN,ILF2, NPR1,INTS3,SLC27A3,GATAD2B,DENND4B,CRTC2,SLC39A1,CREB3L4,JTB,RAB13,RPS27,NUP210L,TPM3,C1orf189,C1orf43,UBAP2L,HAX1, AQP10,ATP8B2,IL6R,SHE,TDRD10,UBE2Q1,CHRNB2,ADAR,KCNN3,PMVK,PBXIP1,PYGO2,SHC1,CKS1B,FLAD1,LENEP,ZBTB7B,DCST2, DCST1,ADAM15,EFNA4,EFNA3,EFNA1,RAG1AP1,DPM3 Amp 1