Anthropomorphic Phantom Developments for the Characterization and Evaluations of Mri Rf Coils
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

The Survival of American Silent Feature Films: 1912–1929 by David Pierce September 2013
The Survival of American Silent Feature Films: 1912–1929 by David Pierce September 2013 COUNCIL ON LIBRARY AND INFORMATION RESOURCES AND THE LIBRARY OF CONGRESS The Survival of American Silent Feature Films: 1912–1929 by David Pierce September 2013 Mr. Pierce has also created a da tabase of location information on the archival film holdings identified in the course of his research. See www.loc.gov/film. Commissioned for and sponsored by the National Film Preservation Board Council on Library and Information Resources and The Library of Congress Washington, D.C. The National Film Preservation Board The National Film Preservation Board was established at the Library of Congress by the National Film Preservation Act of 1988, and most recently reauthorized by the U.S. Congress in 2008. Among the provisions of the law is a mandate to “undertake studies and investigations of film preservation activities as needed, including the efficacy of new technologies, and recommend solutions to- im prove these practices.” More information about the National Film Preservation Board can be found at http://www.loc.gov/film/. ISBN 978-1-932326-39-0 CLIR Publication No. 158 Copublished by: Council on Library and Information Resources The Library of Congress 1707 L Street NW, Suite 650 and 101 Independence Avenue, SE Washington, DC 20036 Washington, DC 20540 Web site at http://www.clir.org Web site at http://www.loc.gov Additional copies are available for $30 each. Orders may be placed through CLIR’s Web site. This publication is also available online at no charge at http://www.clir.org/pubs/reports/pub158. -

Marijuana Business Licenses Approved
OREGON LIQUOR & CANNABIS COMMISSION Marijuana Business Licenses Approved as of 9/9/2021 Retail Medical LICENSE NUMBER LICENSEE NAME BUSINESS NAME LICENSE TYPE ACTIVE COUNTY Delivery Grade Hemp 050 100037147CC Hotbox Farms LLC Hotbox Farms Recreational Retailer Yes Baker Yes 050 10011127277 Scott, Inc 420VILLE Recreational Retailer Yes Baker 020 10017768FC7 Burnt River Farms, LLC Burnt River Farms LLC. Recreational Producer Yes Baker 030 10031846B25 Burnt River Farms, LLC Burnt River Farms LLC. Recreational Processor Yes Baker 060 1003692E356 Burnt River Farms, LLC Burnt River Farms LLC. Recreational Wholesaler Yes Baker 050 1003713A8A4 The Coughie Pot, LLC The Coughie Pot Recreational Retailer Yes Baker 050 10047883377 Sumpter Nugget, LLC Sumpter Nugget Recreational Retailer Yes Baker Yes 030 10071310CDB Nugget Candy Co, LLC Nugget Candy Co, LLC/Bad Rabbit Recreational Processor Yes Baker Yes Solventless 060 10079080A50 420BUNKERVILLE LLC 420 Bunkerville Recreational Wholesaler Yes Baker Yes 020 1007910A67C 420BUNKERVILLE LLC 420 Bunkerville Recreational Producer Yes Baker 020 1008998100D Burnt River Farms, LLC Burnt River Farms LLC Recreational Producer Yes Baker 060 1010135EC04 Hotbox Farms LLC Hotbox Farms Recreational Wholesaler Yes Baker 020 10104590FEE Bad Rabbit Farms LLC Bad Rabbit Farms LLC Recreational Producer Yes Baker 020 10001223B25 Fire Creek Farms LLC. Fire Creek Farms Recreational Producer Yes Benton 020 1000140D286 Bosmere Farms, Inc. Bosmere Farms, Inc. Recreational Producer Yes Benton 020 10004312ECD Grasshopper Farm, -

The Phantom of the Opera | October 24 – November 4, 2018 TPAC’S Jackson Hall
’ ’ The Phantom of the Opera | October 24 – November 4, 2018 TPAC’s Jackson Hall WHAT’S NEXT? – TPAC.ORG • 615-782-4040 Irving Berlin’s The Hip Hop Peter Pan and Tinker Bell: On Your Feet! White Christmas Nutcracker A Pirate’s Christmas JAN 15-20 NOV 13-18 NOV 24 DEC 13-23 Hand-Crafted Cocktails Fine Dining World Class Magicians “Best Ambiance” “Most Romantic” “Best Vibrant Bar Scene” “Most Booked” “Best for Special Occasions” For more information visit HOCNashville.com or call 615.730.8326 Hand-Crafted Cocktails Fine Dining World Class Magicians “Best Ambiance” “Most Romantic” “Best Vibrant Bar Scene” “Most Booked” “Best for Special Occasions” For more information visit HOCNashville.com or call 615.730.8326 SY19-NashvilleMG-7.25x11.125-V1.pdf 1 8/27/2018 3:30:40 PM DISCOVER PROFOUND WISDOM & DIVINE BEAUTY C M “A Must See!” Y — Broadway World CM MY CY CMY K “Inspired…These “There is a massive power “This is the highest “I was uplifted, I was beautiful, gifted people in this that can embrace the and the best of filled with hope... The are expressing something world. It brings great hope… what humans can world is a better place that’s both pure and good.” It is truly a touch of heaven.” produce.” because of Shen Yun.” — Philadelphia Weekly — Daniel Herman, Former Minister of — Olevia Brown-Klahn, singer — Richard Swett, former U.S. Culture of the Czech Republic and musician Congressman JANUARY 22 – 23, 2019 Tickets: 615-721-2999 Tennessee Performing Arts Center ShenYun.com/Nashville ENTIRELY NEW 2019 PRODUCTION • WITH LIVE ORCHESTRA SY19-NashvilleMG-7.25x11.125-V1.pdf 1 8/27/2018 3:30:40 PM DISCOVER PROFOUND WISDOM & DIVINE BEAUTY C M “A Must See!” Y — Broadway World CM MY CY CMY K “Inspired…These “There is a massive power “This is the highest “I was uplifted, I was beautiful, gifted people in this that can embrace the and the best of filled with hope.. -

Court Green Publications
Columbia College Chicago Digital Commons @ Columbia College Chicago Court Green Publications 3-1-2015 Court Green: Dossier: On the Occasion Of Columbia College Chicago Follow this and additional works at: https://digitalcommons.colum.edu/courtgreen Part of the Poetry Commons This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Columbia College Chicago, "Court Green: Dossier: On the Occasion Of" (2015). Court Green. 12. https://digitalcommons.colum.edu/courtgreen/12 This Book is brought to you for free and open access by the Publications at Digital Commons @ Columbia College Chicago. It has been accepted for inclusion in Court Green by an authorized administrator of Digital Commons @ Columbia College Chicago. For more information, please contact [email protected]. “Read good poetry!” —William Carlos Williams COURT GREEN 12 COURT 12 EDITORS CM Burroughs and Tony Trigilio MANAGING EDITOR Cora Jacobs SENIOR EDITORIAL ASSISTANT Jacob Victorine EDITORIAL ASSISTANTS Cameron Decker, Patti Pangborn, Taylor Pedersen, and Andre Price Court Green is published annually in association with Columbia College Chicago, Department of Creative Writing. Our thanks to Matthew Shenoda, Interim Chair, Department of Creative Writing; Suzanne Blum-Malley, Interim Dean, School of Liberal Arts and Sciences; Stanley T. Wearden, Provost; and Kwang-Wu Kim, President and CEO of Columbia College Chicago. Court Green was founded in 2004 by Arielle Greenberg, Tony Trigilio, and David Trinidad. Acknowledgments for this issue can be found on page 209. Court Green is distributed by Ingram Periodicals and Media Solutions. Copyright © 2015 by Columbia College Chicago. ISSN 1548-5242. Magazine cover design by Hannah Rebernick, Columbia College Chicago Creative Services. -
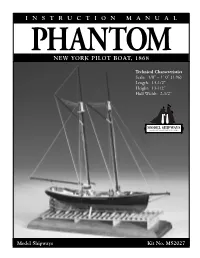
PHANTOM Instr. LAYOUT
INSTRUCTION MANUAL PHANTOM NEW YORK PILOT BOAT, 1868 Technical Characteristics Scale: 1/8” = 1’ 0” (1:96) Length: 13-1/2” Height: 13-1/2” Hull Width: 2-1/2” Model Shipways Kit No. MS2027 Model Shipways Kit No. 2027 PHANTOM New York Pilot Boat, 1868 By George F. Campbell, 1960 Updated Instruction Manual By Ben Lankford Incorporating suggestions by model builder, Arthur Glaser The Model Shipways plans for Phantom were prepared in 1960 by Mr. George F. Campbell, who passed away several years ago. Mr. Campbell was a noted British marine artist, author, naval architect, and historian. He was a member of the Royal Institute of Naval Architects. One of his most noteworthy publications is China Tea Clippers. He also developed the drawings for the Cutty Sark restoration in England, developed the Model Shipways kit of Rattlesnake, and authored Model Shipways’ model handbook, Neophyte Shipmodeler's Jackstay. The Model Shipways plans for Phantom are based on hull lines provided by Howard I. Chapelle, taken from a builder’s half-model in the Smithsonian Institute. Deck details and rigging are based on photo information from the Peabody Museum of Salem, Massachusetts. ©2006 MODEL SHIPWAYS, INC. Sold & distributed by Model Expo, a division of Model Shipways, Inc. • Hollywood, FL 33020 www.modelexpo-online.com A Brief History The Phantom and Pet, sister schooners, were built in 1868-69 at the Phantom was sold to the Sandy Hook (New York) pilots and operated Lawlor yard in East Boston, Massachusetts for the Boston port pilots. out of New York for several years. On March 14, 1886, Phantom was the Dennison J. -

"G" S Circle 243 Elrod Dr Goose Creek Sc 29445 $5.34
Unclaimed/Abandoned Property FullName Address City State Zip Amount "G" S CIRCLE 243 ELROD DR GOOSE CREEK SC 29445 $5.34 & D BC C/O MICHAEL A DEHLENDORF 2300 COMMONWEALTH PARK N COLUMBUS OH 43209 $94.95 & D CUMMINGS 4245 MW 1020 FOXCROFT RD GRAND ISLAND NY 14072 $19.54 & F BARNETT PO BOX 838 ANDERSON SC 29622 $44.16 & H COLEMAN PO BOX 185 PAMPLICO SC 29583 $1.77 & H FARM 827 SAVANNAH HWY CHARLESTON SC 29407 $158.85 & H HATCHER PO BOX 35 JOHNS ISLAND SC 29457 $5.25 & MCMILLAN MIDDLETON C/O MIDDLETON/MCMILLAN 227 W TRADE ST STE 2250 CHARLOTTE NC 28202 $123.69 & S COLLINS RT 8 BOX 178 SUMMERVILLE SC 29483 $59.17 & S RAST RT 1 BOX 441 99999 $9.07 127 BLUE HERON POND LP 28 ANACAPA ST STE B SANTA BARBARA CA 93101 $3.08 176 JUNKYARD 1514 STATE RD SUMMERVILLE SC 29483 $8.21 263 RECORDS INC 2680 TILLMAN ST N CHARLESTON SC 29405 $1.75 3 E COMPANY INC PO BOX 1148 GOOSE CREEK SC 29445 $91.73 A & M BROKERAGE 214 CAMPBELL RD RIDGEVILLE SC 29472 $6.59 A B ALEXANDER JR 46 LAKE FOREST DR SPARTANBURG SC 29302 $36.46 A B SOLOMON 1 POSTON RD CHARLESTON SC 29407 $43.38 A C CARSON 55 SURFSONG RD JOHNS ISLAND SC 29455 $96.12 A C CHANDLER 256 CANNON TRAIL RD LEXINGTON SC 29073 $76.19 A C DEHAY RT 1 BOX 13 99999 $0.02 A C FLOOD C/O NORMA F HANCOCK 1604 BOONE HALL DR CHARLESTON SC 29407 $85.63 A C THOMPSON PO BOX 47 NEW YORK NY 10047 $47.55 A D WARNER ACCOUNT FOR 437 GOLFSHORE 26 E RIDGEWAY DR CENTERVILLE OH 45459 $43.35 A E JOHNSON PO BOX 1234 % BECI MONCKS CORNER SC 29461 $0.43 A E KNIGHT RT 1 BOX 661 99999 $18.00 A E MARTIN 24 PHANTOM DR DAYTON OH 45431 $50.95 -

Viennavienna Wellbeingwellbeing Pagepage 88
and Oakton ViennaVienna WellbeingWellbeing PagePage 88 Classifieds, Page 14 Classifieds, ❖ Directly from the Board: County Sports, Page 12 ❖ Budget Approved News, Page 3 Mother’s Day Photo Gallery Entertainment, Page 10 Photo Gallery ❖ News, Page 4 Opinion, Page 6 A Career-High Performance Sports, Page 12 Madison pitcher Katie Vannicola struck out 21 batters in 10 innings during a 2-1 victory over South Lakes on Friday. Photo by Craig Sterbutzel/The Connection www.ConnectionNewspapers.comMay 4-10, 2016 online atVienna/Oakton www.connectionnewspapers.com Connection ❖ May 4-10, 2016 ❖ 1 2 ❖ Vienna/Oakton Connection ❖ May 4-10, 2016 www.ConnectionNewspapers.com Vienna/Oakton Connection Editor Kemal Kurspahic News 703-778-9414 or [email protected] Bulova calls the budget Directly from the Board a “booster shot.” By Ken Moore priorities and more importantly, I believe it The Connection “This budget provides a needed advances the priorities we heard from our constituents,” said Foust. “I think it repre- hen the Board of Supervi- booster shot to support our sents the board’s commitment to our county sors approved the budget on excellent school system and to employees who have made tremendous sac- WTuesday, April 26, they in- rifices over the past eight years. It reflects creased taxes by about $300 ensure the quality services our our commitment to preserving essential for the average homeowner and increased services and the things that make Fairfax funding for schools by 5 percent. residents expect and rely upon. county great, from parks and libraries to The property tax rate will increase four mental health and transit and housing.” cents from $1.09 to $1.13, per $100 of the Our board heard from thousands He said the budget shows the board’s assessed value of a home. -

Ambrose Bierce - Poems
Classic Poetry Series Ambrose Bierce - poems - Publication Date: 2012 Publisher: Poemhunter.com - The World's Poetry Archive Ambrose Bierce(24 June 1842 - 26 December 1913) Ambrose Gwinnett Bierce was an American editorialist, journalist, short story writer, fabulist and satirist. Today, he is probably best-known for his short story "An Occurrence at Owl Creek Bridge" and his satirical lexicon The Devil's Dictionary. His vehemence as a critic, his motto "Nothing matters" and the sardonic view of human nature that informed his work all earned him the nickname "Bitter Bierce". Despite his reputation as a searing critic, Bierce was known to encourage younger writers, including poet George Sterling and fiction writer W. C. Morrow. Bierce employed a distinctive style of writing, especially in his stories. His style often embraces an abrupt beginning, dark imagery, vague references to time, limited descriptions, impossible events and the theme of war. In 1913, Bierce traveled to Mexico to gain first-hand experience of the Mexican Revolution. While traveling with rebel troops, he disappeared without a trace. <b>Biography</b> Bierce was born at Horse Cave Creek in Meigs County, Ohio to Marcus Aurelius Bierce (1799–1876) and Laura Sherwood Bierce. His mother was a descendant of William Bradford. His parents were a poor but literary couple who instilled in him a deep love for books and writing. The boy grew up in Kosciusko County, Indiana, attending high school at the county seat, Warsaw. He was the tenth of thirteen children whose father gave all of them names beginning with the letter "A". In order of birth, the Bierce siblings were Abigail, Amelia, Ann, Addison, Aurelius, Augustus, Almeda, Andrew, Albert, Ambrose, Arthur, Adelia, and Aurelia. -

2019 Unclaimed Funds Accounts
MahoningX County County 2019 Unclaimed Funds Accounts A Message from Ohio Department of Commerce Director Sheryl Maxfield: The Ohio Department of Commerce’s Division of Unclaimed Funds has returned more than $1 billion to Ohioans since its creation. Could you be the next person to find your missing money? I invite you to take a few minutes to review this insert and see if you or someone you know has a lost treasure just waiting to be claimed. But your search shouldn’t stop here. New accounts are coming in every day, so I invite you to visit missingmoney.com regularly to see if your name appears on the list. Good luck on your search! I hope we have some funds for you or someone in your life. Forgotten Money Unclaimed funds are money or the right to money that has been dormant or forgotten, usually for five years. Each year, the Division of Unclaimed Funds receives accounts that include inactive checking and savings accounts, safe deposit box items, forgotten rent and utility deposits, uncashed payroll checks, undelivered stock certificates and uncashed insurance policies. Enclosed is a list of current or former county residents who had unclaimed funds worth $50 or more reported to the division within the past year. Safe deposit box items received within the past year are listed first. Check your name, as well as family and friends’ names in this year’s list. Names are listed under the hometown of the last known address reported to the division. See a possible match? If you see a possible match, go to missingmoney.com to locate the property or properties as listed. -

Elanor F. Williams CURRICULUM VITAE
Elanor F. Williams CURRICULUM VITAE OFFICE ADDRESS OFFICE PHONE Kelley School of Business 812-856-0835 Indiana University 1309 E. 10th St, Hodge Hall 2100 Bloomington, IN 47405 WEBSITE EMAIL http://elanor-williams.squarespace.com [email protected] EXPERIENCE 2016 – present: Assistant Professor, Marketing Department, Kelley School of Business, Indiana University 2014 – 2016: Assistant Research Scientist, Rady School of Management, University of California, San Diego 2012 – 2014: Postdoctoral Scholar, Rady School of Management, University of California, San Diego 2008 – 2012: Postdoctoral Fellow, Warrington School of Business, University of Florida EDUCATION CORNELL UNIVERSITY PhD Social Psychology, 2008; Graduate advisor: Thomas Gilovich Dissertation: “The dynamic self: The use of ideals and intentions in understanding self and others” YALE UNIVERSITY BA Psychology, 2001; Undergraduate advisor: Geoffrey L. Cohen Distinction in the Major Thesis: “The accuracy of lay theories about gender differences in the fundamental attribution error” RESEARCH INTERESTS I study the social consumer. Consumer decisions are often interactive and are becoming ever more social in nature—for example, people can learn about new products, review and share experiences, and get feedback from others in ways that were unimaginable even 10 years ago. My research examines how consumers make decisions on behalf of and with the help of other people. I also investigate how consumers come to know themselves and others, and how that knowledge (or lack thereof) influences the choices they make. In my work, I strive to unravel how consumers’ choices, struggles, and triumphs are influenced by the company that they keep. PUBLICATIONS AND MANUSCRIPTS ARTICLES AND CHAPTERS Steffel, Mary, Elanor F. -

Liner Notes, No. 22
ARCHIVES OF AFRICAN AMERICAN MUSIC AND CULTURE liner notesNO. 22 / 2017-2018 featuring Bootsy Collins & Dr. Scot Brown aaamc mission From the Desk of the Director The AAAMC is devoted to the collection, preservation, and dissemination of materials for Greetings, repository recognized and utilized the purpose of research and by multiple constituencies within the study of African American When I began my new role as Director university and beyond. Much gratitude is music and culture. of the AAAMC on January 1, 2018, it owed to these two prestigious scholars in aaamc.indiana.edu was evident to me that the past directors, Black music who carried the torch as past Drs. Portia Maultsby and Mellonee directors. Burnim, established a firm foundation As current Director of the AAAMC, Table of Contents and legacy for me to extend upon. Dr. my vision is to increase our collection Maultsby founded AAAMC in 1991 acquisitions and visibility in ways that From the Desk of working tirelessly for over two decades foster unique interactions amongst and the Director .........................2 while collecting a treasure trove of vital between the academy, industry and information representing our current community sectors. With this broad In the Vault: holdings on Black music and culture, vision in mind, I have initiated a few Recent Donations .................3 which include both published and strategies for success. First, during unpublished materials in a variety of spring 2018, I developed a new forum formats: A/V time-based media, paper, series called “Groovin’ Black” where Bootsy Collins Comes photographs, memorabilia (wood, metal, students, premiere scholars, acclaimed to Campus ...........................4 plastic, cloth, etc.). -

Locked Up, Shut Up: Why Speech in Prison Matters Evan Bianchi
St. John's Law Review Volume 92 Article 2 Number 1 Volume 92, Spring 2018, Number 1 September 2018 Locked Up, Shut Up: Why Speech in Prison Matters Evan Bianchi David Shapiro Follow this and additional works at: https://scholarship.law.stjohns.edu/lawreview Recommended Citation Evan Bianchi and David Shapiro (2018) "Locked Up, Shut Up: Why Speech in Prison Matters," St. John's Law Review: Vol. 92 : No. 1 , Article 2. Available at: https://scholarship.law.stjohns.edu/lawreview/vol92/iss1/2 This Article is brought to you for free and open access by the Journals at St. John's Law Scholarship Repository. It has been accepted for inclusion in St. John's Law Review by an authorized editor of St. John's Law Scholarship Repository. For more information, please contact [email protected]. FINAL_SHAPIRO 9/10/2018 1:57 PM ARTICLES LOCKED UP, SHUT UP: WHY SPEECH IN PRISON MATTERS EVAN BIANCHI† & DAVID SHAPIRO† INTRODUCTION On January 18, 2017, Michael D. Williams, an Alabama prisoner, received notice from Holman Correctional Facility that his mail had been rejected.1 The prison was blocking his receipt of the San Francisco Bay View, a 40-year-old national black newspaper covering political and cultural issues in the Bay Area and beyond.2 The newspaper publishes articles and op-eds on topics such as the childcare crisis,3 the need for multi-unit smoke-free housing policies,4 net neutrality and free speech,5 and police response to crimes involving black victims.6 Writings by prisoners are often featured in the publication as well.7 † Law Clerk, United States District Court for the Southern District of Texas.