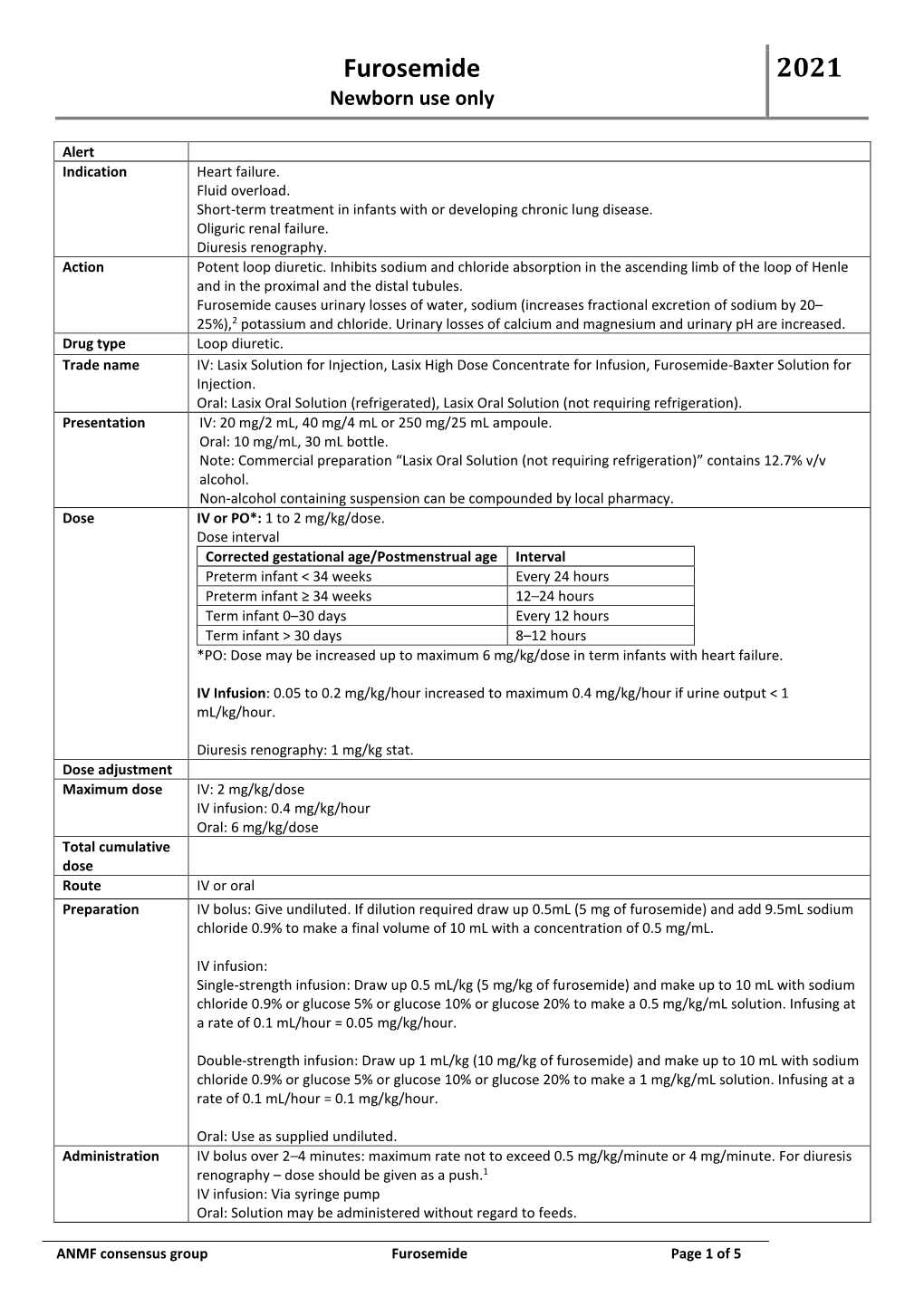
Furosemide 2021 Newborn Use Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Presentations September 23Rd - Rooms 1,2 and 3
Oral Presentations September 23rd - Rooms 1,2 and 3 Presentation Date Abstract Authors Presenter´s name - Theme Title Code indicated by the author 18498 Thomas Smits; Femke Gresnigt; Thomas Smits Clinical Toxicology/drugs of PERFORMANCE OF AN IMMUNOASSAY Eric Franssen; Milly Attema-de abuse METHOD FOR GAMMA-HYDROXYBUTYRIC Jonge ACID (GHB) IN PATIENTS PRESENTED AT THE EMERGENCY DEPARTMENT, A PROSPECTIVE STUDY 18499 Thomas Smits; Femke Gresnigt; Thomas Smits Clinical Toxicology/drugs of DO WE NEED POINT-OF-CARE TESTING OF Milly Attema-de Jonge; Eric abuse GAMMA-HYDROXYBUTYRIC ACID (GHB) AT Fransse THE EMERGENCY DEPARTMENT? September 23 18730 Lilian H.J. Richter; Julia Menges; Lea Wagmann Clinical Toxicology/drugs of NEW PSYCHOACTIVE SUBSTANCES: Lea Wagmann; Simon D. Brandt; abuse METABOLIC FATE, ISOZYME-MAPPING, 13:30 - 14:45 Folker Westphal; Veit Flockerzi; AND PLASMA PROTEIN BINDING OF 5-APB- ROOM 1 Markus R. Meyer NBOME, 2C-B-FLY-NB2ETO5CL, AND 2C-B- FLY-NBOME 18985 Annelies Cannaert; Marie Annelies Cannaert Clinical Toxicology/drugs of HIDE AND SEEK: OVERCOMING THE Deventer; Melissa Fogarty; abuse MASKING EFFECT OF OPIOID Amanda L.A. Mohr; Christophe P. ANTAGONISTS IN ACTIVITY-BASED Stove SCREENING TESTS 18740 Souleiman El Balkhi ; Roland Souleiman El Balkhi Clinical Toxicology/drugs of METABOLIC INTERACTIONS BETWEEN Lawson; Franck Saint-Marcoux abuse OXYCODONE, BENZODIAZEPINES OR DESIGNER BENZODIAZEPINES PLAY AN IMPORTANT ROLE IN OXYCODONE INTOXICATIONS 19050 Brenda de Winter F de Velde; MN Brenda de Winter Anti-infective drugs POPULATION -

Critical Access COVID-19 Drugs Shortages (156-40)
Resilient Drug Supply Project: Critical Acute Drug List & Critical COVID-19 Drug List Drug Shortages Reported by ASHP & FDA Shortages as of 8/22/2021 UMN RDSP UMN RDSP ASHP FDA Drug Critical Acute Drugs Drug Category List of 156 List of 40 Drug Drug # Generic Name Critical Acute Critical Shortage Shortage Drugs COVID-19 List List Drugs 1 Cisatracurium Paralytic X X Yes 2 Rocuronium Paralytic X X Yes 3 Vecuronium Paralytic X X Yes Yes 4 Succinylcholine Paralytic X X 5 Atracurium Paralytic X 6 Propofol Sedation X X Yes Yes 7 Midazolam Sedation X X Yes Yes 8 Lorazepam Sedation X X Yes Yes 9 Dexmedetomidine Sedation/Anesthesia X X Yes Yes 10 Phenobarbital Sedation X 11 Ketamine Sedation/Anesthesia X X Yes Yes 12 Diazepam Sedation X 13 Lidocaine Local Anesthetic X Yes Yes 14 Bupivacaine Local Anesthetic X Yes Yes 15 Fentanyl Pain X X Yes Yes 16 Hydromorphone Pain X X Yes Yes 17 Morphine Pain X X Yes Yes 18 Oxycodone Pain X X 19 Acetaminophen Pain & Fever X 20 Ketorolac Pain X Yes Yes 21 Anakinra Pain X 22 Oxygen Medical Gas X X 23 Nitric Oxide Medical Gas X 24 Sevoflurane Medical Gas X 25 Albuterol Bronchodilator X X Yes 26 Ipratropium (Inhaler) Bronchodilator X 27 Azithromycin Anti-infective X X 28 Piperacillin-Tazobactam Anti-infective X X 29 Cefepime Anti-infective X X Yes 30 Ceftriaxone Anti-infective X 31 Vancomycin Anti-infective X X Yes 32 Doxycycline Anti-infective X 33 Meropenem Anti-infective X X 34 Cefazolin Anti-infective X X Yes Yes 35 Levofloxacin Anti-infective X 36 Linezolid Anti-infective X 37 Ampicillin-Sulbactam Anti-infective -

268 Part 522—Implantation Or Injectable Dosage Form
§ 520.2645 21 CFR Ch. I (4–1–18 Edition) (ii) Indications for use. For the control 522.82 Aminopropazine. of American foulbrood (Paenibacillus 522.84 Beta-aminopropionitrile. larvae). 522.88 Amoxicillin. 522.90 Ampicillin injectable dosage forms. (iii) Limitations. The drug should be 522.90a Ampicillin trihydrate suspension. fed early in the spring or fall and con- 522.90b Ampicillin trihydrate powder for in- sumed by the bees before the main jection. honey flow begins, to avoid contamina- 522.90c Ampicillin sodium. tion of production honey. Complete 522.144 Arsenamide. treatments at least 4 weeks before 522.147 Atipamezole. main honey flow. 522.150 Azaperone. 522.161 Betamethasone. [40 FR 13838, Mar. 27, 1975, as amended at 50 522.163 Betamethasone dipropionate and FR 49841, Dec. 5, 1985; 59 FR 14365, Mar. 28, betamethasone sodium phosphate aque- 1994; 62 FR 39443, July 23, 1997; 68 FR 24879, ous suspension. May 9, 2003; 70 FR 69439, Nov. 16, 2005; 73 FR 522.167 Betamethasone sodium phosphate 76946, Dec. 18, 2008; 75 FR 76259, Dec. 8, 2010; and betamethasone acetate. 76 FR 59024, Sept. 23, 2011; 77 FR 29217, May 522.204 Boldenone. 17, 2012; 79 FR 37620, July 2, 2014; 79 FR 53136, 522.224 Bupivacaine. Sept. 8, 2014; 79 FR 64116, Oct. 28, 2014; 80 FR 522.230 Buprenorphine. 34278, June 16, 2015; 81 FR 48702, July 26, 2016] 522.234 Butamisole. 522.246 Butorphanol. § 520.2645 Tylvalosin. 522.275 N-Butylscopolammonium. 522.300 Carfentanil. (a) Specifications. Granules containing 522.304 Carprofen. 62.5 percent tylvalosin (w/w) as 522.311 Cefovecin. -

Sample Chapter
LCMS_Chap09 (JB-D) 8/5/06 3:14 pm Page 193 9 LC-MS in doping control Detlef Thieme Introduction adjacent fields with similar analytical prospects, like veterinary residue control (predominantly dealing with identification of growth promoters Definition of doping in various matrices), forensic sciences (the major- ity of doping-relevant substances are scheduled Doping analysis comprises a diversity of sub- as controlled substances in most countries), stance classes with different pharmaceutical and environmental analysis (e.g. steroids in waste chemical properties. Therefore, the discussion of water) or clinical chemistry (e.g. due to the the suitability of liquid chromatography-mass increasing relevance of steroid hormone replace- spectrometry (LC-MS) in doping analysis needs ment therapy). to distinguish various categories. This chapter describes the key fields of appli- According to its formal definition, a doping cation of LC-MS in routine doping control (i.e. violation in sports can be caused by various screening analysis, confirmation and quantifica- events, e.g.: tion of positive results) extra to particular • the detection of a prohibited substance or research activities. The latter are focused on the metabolites or markers of that substance (as intended technical improvements (e.g. extension defined by the recent document [1] of the of detection time windows, reduction of turn- World Anti-Doping Agency [WADA]) in the around times and costs) of conventional analyti- athlete’s specimen cal procedures and, in particular, on the detection • the use of prohibited substances or methods of prohibited substances that cannot be ade- • possession or trafficking prohibited substances quately identified so far (e.g. -

Subject Index to Abstracts
003 1-3998/84/1804-429ASO2.00 PEDIATRIC RESEARCH Vol. 18 No. 4, 1984 Copyright 0 1984 International Pediatric Research Foundation, Inc. Prinled in U.S.A. Subject Index to Abstracts Abortion 767 Adenosine 2 15, 389 Aminoglycoside 342, 1140 Arachidonic acid 295, 925, 1125, Absorption, gastrointestinal 7 15 Adenosine deaminase deficiency Aminonucleoside nephrosis 1598 1 139, 1254 Absorption, passive 706 888 Aminophylline 137 1, 1853 Arginine 134 1 Abstinence 140 1 Adenosine triphosphate 839 Aminopyrine 388 Arginine vasopressin 234,235,249 Abuse 24, 28, 37, 105 Adenovirus 542, 1044, 1073, 1133 Ammonia 1 397, 1707 Argininosuccinicaciduria 78 1 Abuse, sexual 1085 Adenylate kinase 1648 Amnesia 825 Argininosuccinate 742, 1 166 Abuse, substance 62 Adipocytes 44 1 Amniotic fluid 229, 618, 779, Arrhythmia 179, 195, 222, 223, Acanthosis 12 17 Adipose tissue 23 1, 69 1 1304, 1535 377,857,9 13, 1796 Accidents 5 1 1, 5 18 Adiposity 673 Amniotic leak, prolonged 1739 Arteriohepatic dysplasia 1642 Accretion 300 Admissions 825 Amoxicillin 8 19 Artery 1753 Acetaldehyde 777 Adolescence 1, 3, 4, 9, 10, 12, 16, Amphotericin 900, 1350, 1369 Artery, carotid 20 1 Acetaminophen 282, 297, 38 1, 19, 22, 24, 25 Ampicillin 11 14, 1147 Artery, mesenteric 372 390 Adrenal 14, 315,405,413,446 Amrinone 175,345 Artery, pulmonary 186, 2 17, 328, Acetylcholine 277 Adrenal hormones 18 Androgen 14,449, 465, 12 17 5 10 Acetyl-CoA 1200 Adrenal medulla 270 Anemia 20, 140, 143, 500, 545, Arthritis 1 167 N-Acetyl-P-D-glucosaminidase Adrenarche 4 13, 502 816, 835, 846, 888, 896, 904, -

DIURETICS Diuretics Are Drugs That Promote the Output of Urine Excreted by the Kidneys
DIURETICS Diuretics are drugs that promote the output of urine excreted by the Kidneys. The primary action of most diuretics is the direct inhibition of Na+ transport at one or more of the four major anatomical sites along the nephron, where Na+ reabsorption takes place. The increased excretion of water and electrolytes by the kidneys is dependent on three different processes viz., glomerular filtration, tubular reabsorption (active and passive) and tubular secretion. Diuretics are very effective in the treatment of Cardiac oedema, specifically the one related with congestive heart failure. They are employed extensively in various types of disorders, for example, nephritic syndrome, diabetes insipidus, nutritional oedema, cirrhosis of the liver, hypertension, oedema of pregnancy and also to lower intraocular and cerebrospinal fluid pressure. Therapeutic Uses of Diuretics i) Congestive Heart Failure: The choice of the diuretic would depend on the severity of the disorder. In an emergency like acute pulmonary oedema, intravenous Furosemide or Sodium ethacrynate may be given. In less severe cases. Hydrochlorothiazide or Chlorthalidone may be used. Potassium-sparing diuretics like Spironolactone or Triamterene may be added to thiazide therapy. ii) Essential hypertension: The thiazides usually sever as primary antihypertensive agents. They may be used as sole agents in patients with mild hypertension or combined with other antihypertensives in more severe cases. iii) Hepatic cirrhosis: Potassium-sparing diuretics like Spironolactone may be employed. If Spironolactone alone fails, then a thiazide diuretic can be added cautiously. Furosemide or Ethacrymnic acid may have to be used if the oedema is regractory, together with spironolactone to lessen potassium loss. Serum potassium levels should be monitored periodically. -

PRIMAXIN (Imipenem and Cilastatin)
• Known hypersensitivity to any component of PRIMAXIN (4) HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use ----------------------- WARNINGS AND PRECAUTIONS ---------------------- PRIMAXIN safely and effectively. See full prescribing information • Hypersensitivity Reactions: Serious and occasionally fatal for PRIMAXIN. hypersensitivity (anaphylactic) reactions have been reported in patients receiving therapy with beta-lactams. If an allergic reaction PRIMAXIN® (imipenem and cilastatin) for Injection, for to PRIMAXIN occurs, discontinue the drug immediately (5.1). intravenous use • Seizure Potential: Seizures and other CNS adverse reactions, such Initial U.S. Approval: 1985 as confusional states and myoclonic activity, have been reported during treatment with PRIMAXIN. If focal tremors, myoclonus, or --------------------------- RECENT MAJOR CHANGES -------------------------- seizures occur, patients should be evaluated neurologically, placed Indications and Usage (1.9) 12/2016 on anticonvulsant therapy if not already instituted, and the dosage of Dosage and Administration (2) 12/2016 PRIMAXIN re-examined to determine whether it should be decreased or the antibacterial drug discontinued (5.2). ----------------------------INDICATIONS AND USAGE --------------------------- • Increased Seizure Potential Due to Interaction with Valproic Acid: PRIMAXIN for intravenous use is a combination of imipenem, a penem Co-administration of PRIMAXIN, to patients receiving valproic acid antibacterial, and cilastatin, a renal dehydropeptidase inhibitor, or divalproex sodium results in a reduction in valproic acid indicated for the treatment of the following serious infections caused by concentrations. The valproic acid concentrations may drop below designated susceptible bacteria: the therapeutic range as a result of this interaction, therefore • Lower respiratory tract infections. (1.1) increasing the risk of breakthrough seizures. The concomitant use of • Urinary tract infections. -
Uniform Classification Guidelines for Foreign Substances and Recommended Penalties Model Rule
DRUG TESTING STANDARDS AND PRACTICES PROGRAM. Uniform Classification Guidelines for Foreign Substances And Recommended Penalties Model Rule. January, 2018 (V.13.4) Ó ASSOCIATION OF RACING COMMISSIONERS INTERNATIONAL – 2018. Association of Racing Commissioners International 1510 Newtown Pike, Lexington, Kentucky, United States www.arci.com Page 1 of 61 Preamble to the Uniform Classification Guidelines of Foreign Substances The Preamble to the Uniform Classification Guidelines was approved by the RCI Drug Testing and Quality Assurance Program Committee (now the Drug Testing Standards and Practices Program Committee) on August 26, 1991. Minor revisions to the Preamble were made by the Drug Classification subcommittee (now the Veterinary Pharmacologists Subcommittee) on September 3, 1991. "The Uniform Classification Guidelines printed on the following pages are intended to assist stewards, hearing officers and racing commissioners in evaluating the seriousness of alleged violations of medication and prohibited substance rules in racing jurisdictions. Practicing equine veterinarians, state veterinarians, and equine pharmacologists are available and should be consulted to explain the pharmacological effects of the drugs listed in each class prior to any decisions with respect to penalities to be imposed. The ranking of drugs is based on their pharmacology, their ability to influence the outcome of a race, whether or not they have legitimate therapeutic uses in the racing horse, or other evidence that they may be used improperly. These classes of drugs are intended only as guidelines and should be employed only to assist persons adjudicating facts and opinions in understanding the seriousness of the alleged offenses. The facts of each case are always different and there may be mitigating circumstances which should always be considered. -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -
Drug-Related Laboratory Test Interference
REFERENCES • Chun KY. Biotin Interference in Diagnostic Tests. Clinical Chemistry 2017; 63: 619-20. • da Silva-Colombeli AS, Falkenberg M. Analytical interfer- ASCLS Mission: ences of drugs in the chemical examination of urinary protein. Clinical Biochemistry 2007; 40: 1074-6. • Hart MH, de Vrieze H, Wouters D et al. Differential effect The mission of ASCLS is of drug interference in immunogenicity assays. Journal of Immunological Methods 2011; 372: 196-203. to make a positive impact • Lippi G, Daves M, Mattiuzzi C. Interference of medical contrast media on laboratory testing. Biochemia Medica Laboratory in health care through 2014; 24: 80-8. leadership that will • Nagase S, Kohguchi K, Tohyama K et al. Interference by Patient Safety Pralidoxime (PAM) salts in clinical laboratory tests. Clinica assure excellence in the Chimica Acta 2013; 416: 72-9. • Tsakiris DA. Direct Oral Anticoagulants-Interference With Tips: practice of laboratory Laboratory Tests and Mechanism of Action. Semin Hema- tol 2014; 51: 98-101. medicine. • Vasudevan S, Hirsch IB. Interference of Intravenous Vita- min C With Blood Glucose Testing. Diabetes Care 2014; 37: Drug-related E93-E4. • Williams GR, Cervinski MA, Nerenz RD. Assessment of Laboratory Test biotin interference with qualitative point-of-care hCG test devices. Clinical Biochemistry 2018; 53: 168-70. Interference • Amanatullah DF, Lopez MJ, Gosselin RC, Gupta MC. Case Report: Artificial Elevation of Prothrombin Time by Tela- For vancin. Clin Orthop Rel Res 2013; 471: 332-5. • Martin EL, Taylor HL. False-Positive Viral Serologies Due to Providers Intravenous Immunoglobulin Administration in a Case of Suspected Transfusion-Transmitted Disease. American Journal of Clinical Pathology 2012; 138: A256-A. -

Mechanisms of Sevoflurane-Induced Myocardial Preconditioning In
Anesthesiology 2003; 99:27–33 © 2003 American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Mechanisms of Sevoflurane-induced Myocardial Preconditioning in Isolated Human Right Atria In Vitro Alexandra Yvon, B.Sc.,* Jean-Luc Hanouz, M.D, Ph.D.,† Benoît Haelewyn, B.Sc.,* Xavier Terrien, B.Sc.,* Massimo Massetti, M.D.,‡ Gérard Babatasi, M.D., Ph.D.,‡ André Khayat, M.D.,§ Pierre Ducouret, Ph.D., Henri Bricard, M.D.,# Jean-Louis Gérard, M.D., Ph.D.** Background: The authors examined the role of adenosine postischemic contractile function,5–7 and metabolic triphosphate–sensitive potassium channels and adenosine A 7 1 function. Although the mechanisms involved in anes- receptors in sevoflurane-induced preconditioning on isolated thetic preconditioning remain incompletely understood, human myocardium. Methods: The authors recorded isometric contraction of hu- protein kinase C, adenosine triphosphate–sensitive po- man right atrial trabeculae suspended in oxygenated Tyrode’s tassium (KATP) channels, and adenosine A1 receptors Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/99/1/27/408853/0000542-200307000-00008.pdf by guest on 02 October 2021 solution (34°C; stimulation frequency, 1 Hz). In all groups, a seem to play a key role.1,2,5,6 However, recent studies 30-min hypoxic period was followed by 60 min of reoxygenation. suggest that volatile anesthetic–induced myocardial pre- Seven minutes before hypoxia reoxygenation, muscles were ex- posed to 4 min of hypoxia and 7 min of reoxygenation or 15 min conditioning may be dependent on species and experi- 5,8 of sevoflurane at concentrations of 1, 2, and 3%. In separate mental models. -

FAST FACTS and CONCEPTS #20 OPIOID DOSE ESCALATION in END-OF-LIFE CARE David E Weissman MD, Andrew Kamell MD Background a Comm
FAST FACTS AND CONCEPTS #20 OPIOID DOSE ESCALATION IN END-OF-LIFE CARE David E Weissman MD, Andrew Kamell MD Background A common question from trainees is “How fast, and by how much, can opioids be safely dose escalated in terminally ill patients?” Consider the analogy of furosemide (Lasix) when discussing this topic. An increase in Lasix from 10 mg to 11 mg is unheard of, yet that is precisely what often happens with opioids, especially parenteral infusions. For example, increasing a morphine infusion from 1 to 2 mg/hr is a 100% does increase; while going from 5 to 6 mg/hr is only a 20% increase. Yet, many orders are written, “increase drip by 1 mg/hr, titrate to comfort.” Some hospitals and nursing units even have this as a standing order or nursing policy. Such titration orders are unlikely to lead to be effective. Key clinical considerations for appropriate opioid escalation: 1. Is an opioid dose escalation appropriate? To answer that question, clinicians need to consider: a. Is the patient tolerating opioids well with little adverse effects? b. Is the pain or dyspnea expected to continue at a similar or progressive pattern (particularly relevant for scheduled medications or infusions) or might it be temporary? c. Is the source of discomfort opioid responsive? d. Is there evidence of hyperalgesia or neurotoxicity from opioids? See Fast Facts #57,58, and 142. e. Is the pain related to a chronic, non-malignant source in which the patient has an extended prognosis? If so, then aggressive opioid titrations may not be the best long-term solution.