Functional Gastrointestinal Disorders and the Joint Hypermobility Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GASTROMEGALY and CHRONIC DUODENAL ILEUS in CHILDREN by REGINALD MILLER, M.D., F.R.C.P., Physician, Paddington Green Children's Hospital, with H
Arch Dis Child: first published as 10.1136/adc.5.26.83 on 1 April 1930. Downloaded from GASTROMEGALY AND CHRONIC DUODENAL ILEUS IN CHILDREN BY REGINALD MILLER, M.D., F.R.C.P., Physician, Paddington Green Children's Hospital, with H. COURTNEY GAGE, L.R.C.P., M.R.C.S., Radiologist, St. Mary's Hospital, London. This paper is concerned with a series of nine children who exhibited enlargement of the stomach with visible gastric peristalsis or other signs of obstruction high in the alimentary tract. The similarity between the cases is sufficient to suggest that they all belong to one group originating in some form of duodenal obstruction. Two of the nine cases were submitted to operation and were found to be examples of chronic duodenal ileus, and it is suggested that the others of the series owe their origin to the same cause. Gastromegaly is a convenient term for the enlarged and hypertrophied stomach which is the most striking clinical feature of such cases as these. http://adc.bmj.com/ Such a condition implies obstruction to the evacuation of the stomach and may be due to various causes; and as the site and nature of the obstruction, and even its very presence, may be difficult to determine, it is useful to have a group name which covers all such cases and emphasizes their one most obvious clinical abnormality. Were, for instance, the diagnosis of chronic duodenal ileus in the present cases disputed (and the subject is one of great difficulty), they would remain as a type of gastromegaly of obscure origin. -

Thme CANADIAN MEDICAL ASSOCIATION JOURNAL 137
Aug. 1930] THmE CANADIAN MEDICAL ASSOCIATION JOURNAL 137 DYSPEPSIA By ROBERT HUTCHISON, M.D., F.R.C.P., Phystcian to the London Hospital, London, Eng. TIHE first duty of anyone who undertakes to may lead to error, as to that form, not so write about dyspepsia is to define what he very uncommon, in which vomiting and even means by the term, for it is a word which is some pain occurs after every meal; such used very loosely, as we all know, both by doc- symptoms when they occur in a young un- tors and by patients, and is often enough made married woman may easily deceive. Or take to cover any form of abdominal discomfort again the vomiting of the gastric crises in which a patient may experience. But accuracy tabes. When these crises occur, as they some- :of diagnosis and efficient treatment demand a times do, early in the disease and before more precise use than this, and I propose in the the deep reflexes have disappeared, the fact of present paper to include under the term only their nervous origin is easily overlooked, and such abdominal discomfort as is felt during the every physician and surgeon of experience progress of digestion, and which is due to organic must have known cases in which even a gastro- disease of the stomach or to a primary disorder jejunostomy has been performed for gastric of its functions. For the purposes of this defini- crises under the belief that the patient was tion the duodenum may be regarded as part of s-uffering from organic disease of the stomach. -

Digestive Conditions, Miscellaneous Examination (Tuberculous
Digestive Conditions, Miscellaneous Examination (Tuberculous peritonitis, Inguinal hernia, Ventral hernia, Femoral hernia, Visceroptosis, and Benign and Malignant new growths) Comprehensive Worksheet Name: SSN: Date of Exam: C-number: Place of Exam: A. Review of Medical Records: B. Medical History (Subjective Complaints): 1. State date of onset, and describe circumstances and initial manifestations. 2. Course of condition since onset. 3. Current treatment, response to treatment, and any side effects of treatment. 4. History of related hospitalizations or surgery, dates and location, if known, reason or type of surgery. 5. If there was hernia surgery, report side, type of hernia, type of repair, and results, including current symptoms. 6. If there was injury or wound related to hernia, state date and type of injury or wound and relationship to hernia. 7. History of neoplasm: a. Date of diagnosis, exact diagnosis, location. b. Benign or malignant. c. Types of treatment and dates. d. Last date of treatment. e. State whether treatment has been completed. 8. For tuberculosis of the peritoneum, state date of diagnosis, type(s) and dates of treatment, date on which inactivity was established, and current symptoms. C. Physical Examination (Objective Findings): Address each of the following and fully describe current findings: 1. For hernia, state: a. type and location (including side) b. diameter in cm. c. whether remediable or operable d. whether a truss or belt is indicated, and whether it is well- supported by truss or belt e. whether it is readily reducible f. whether it has been previously repaired, and if so, whether it is well-healed and whether it is recurrent g. -

Department of Veterans Affairs § 4.114
Department of Veterans Affairs § 4.114 DISEASES OF THE HEART—Continued § 4.111 Postgastrectomy syndromes. Rat- There are various postgastrectomy ing symptoms which may occur following anastomotic operations of the stom- With the following in affected parts: Arthralgia or other pain, numbness, ach. When present, those occurring or cold sensitivity plus two or during or immediately after eating and more of the following: tissue loss, known as the ‘‘dumping syndrome’’ are nail abnormalities, color changes, characterized by gastrointestinal com- locally impaired sensation, hyperhidrosis, X-ray abnormali- plaints and generalized symptoms sim- ties (osteoporosis, subarticular ulating hypoglycemia; those occurring punched out lesions, or osteo- from 1 to 3 hours after eating usually arthritis) ....................................... 30 present definite manifestations of Arthralgia or other pain, numbness, or cold sensitivity plus tissue hypoglycemia. loss, nail abnormalities, color changes, locally impaired sensa- § 4.112 Weight loss. tion, hyperhidrosis, or X-ray ab- normalities (osteoporosis, sub- For purposes of evaluating conditions articular punched out lesions, or in § 4.114, the term ‘‘substantial weight osteoarthritis) ............................... 20 loss’’ means a loss of greater than 20 Arthralgia or other pain, numbness, percent of the individual’s baseline or cold sensitivity ......................... 10 weight, sustained for three months or NOTE (1): Separately evaluate amputations of fingers or toes, and complications such as squamous cell longer; and the term ‘‘minor weight carcinoma at the site of a cold injury scar or pe- loss’’ means a weight loss of 10 to 20 ripheral neuropathy, under other diagnostic codes. percent of the individual’s baseline Separately evaluate other disabilities that have been diagnosed as the residual effects of cold in- weight, sustained for three months or jury, such as Raynaud’s phenomenon, muscle at- longer. -

Visceroptosis As a Cause of Stomach Trouble
VISCEROPTOSIS AS A CAUSE OF more physicians. In the writer's opinion, the "STOMACH TROUBLE." patient, and at times the family, may all be said to be in a state of neurasthenia. And small By William D. Reid, M.D., Boston. wonder, as they often have been given as many Visceroptosis has received a large share of opinions as they have consulted doctors,—some attention from orthopedists and internists dur- advising resort to surgery and others against. ing the past two decades, and medical literature This variation in the advice received generally is not lacking in excellent articles on the sub- has an upsetting effect. ject. Nevertheless, one continues to see cases At this point a few case reports will best serve not yet diagnosed, though they have passed to picture the type of patient to which the through the hands of one or more physicians. writer would draw attention. The type to which the writer refers is that in which the comes for relief of "stomach patient Case 1. Single woman. Seen June, 1915. not will trouble." It is held that this paper Aged 34 years. Canadian ; school teacher. Said present new facts, but it is hoped that it may to have gastric ulcer, but patient believes can- lay further emphasis on an important subject. cer to be the correct diagnosis. Family History The American Illustrated Dictionary defines —-Negative. Past History—Chicken-pox, scar- let fever and measles in childhood. "Sort of as "a or the falling down, visceroptosis prolapse, until 13 years old. Sore throat once a of " It is sometiues called Glenard 's puny" the viscera. -

Of Gastroptosis, Which, Though Only an Incidental Part Enteroptosis, Is
Dr. J. R. Pennington, Chicago : The general practitioner mobility of the stomach, which is affected by the posi¬ is entitled to the same information as the specialist; conse¬ tion of the individual, by the weight of the stomach quently, I intended that this paper should contain statistical contents and by the tension or relaxation of the abdom¬ information not obtained the and other readily by average inal muscles. We have endeavored to determine the physician. Dr. Hirschman is to be commended for his normal of the stomach in a of valuable suggestions, and were they put into practice "by position study 1,000 insurance companies and others they would do much for the cases, and have come to the conclusion that in the control of this dreaded disease. supine position the textbook teachings are correct ; but in the upright position there is a wide normal variation depending on the anatomic make-up of various types of individuals. there seems to be as much A CLINICAL AND ROENTGENOGRAPHIC Indeed, difference in the size, contour and position of the STUDY OF GASTROPTOSIS stomachs of men as there is of their mouths. come so as OBSERVATIONS IN ONE THOUSAND GASTRO- We have also to the conclusion that far is it matters INTESTINAL PATIENTS gastric digestion concerned, very little whether a stomach is in the high position or in the brim SEALE HARRIS, M.D. of the pelvis, so long as its muscular tonus is good and AND the intra-abdominal pressure is normal. We have J. P. CHAPMAN, M.D. repeatedly found patients whose stomachs in the BIRMINGHAM, ALA. -

The CLINICAL ASPECTS of VISCEROPTOSIS 213
CLINICSL A4SPECTS OF VISCEROPTOSIS 185 THE CLINICAL ASPECTS OF VISCEBOPTOSIS. BY ALBERT J. WALTON, LONDON. IT has been the experience of all surgeons to meet with cases presenting the symptoms of some acute or chronic abdominal lesion which at operation fail to show the expected pathological change. Until a few years ago it was cus- tomary to believe that an error of diagnosis had been made and that a laparo- tomg had been performed unjustifiably. For this reason but few of these cases were reported, and our knowledge of the cause of the symptoms remained uncertain. ‘ Gradually, however, it became clear that the majority could be grouped together in so far as they presented definite lesions, and increasing experience has shown that, although the symptoms might vary considerably, these pathological changes are remarkably constant. As soon as this fact became evident, attention was more fully directed to the subject, so that the existence of this group of cases is now well recognized. The conditions discovered at operation have been frequently described, and many terms have been applied to the changes found in one 01: more areas. WiIms24 believes that the symptoms are largely due to excessive mobility and dilatation of the caecum. Jackson13 has described fully an abnormal and characteristic membrane found on the anterior wall of the cccum, and has shown how this membrane, which had previously been de- scribed as the parietocolic membrane by Jonnesco and Juvara,l4 might be the cause of clinical symptoms. Payrl8 has given a detailed description of a somewhat similar membrane in the region of the splenic flexure. -
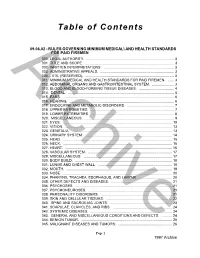
Table of Contents
Table of Contents 09.06.02 - RULES GOVERNING MINIMUM MEDICAL\ AND HEALTH STANDARDS FOR PAID FIREMEN 000. LEGAL AUTHORITY. ........................................................................................ 3 001. TITLE AND SCOPE. ......................................................................................... 3 002. WRITTEN INTERPRETATIONS. ...................................................................... 3 003 ADMINISTRATIVE APPEALS. .......................................................................... 3 004.-- 010. (RESERVED). ......................................................................................... 3 Archive011. MINIMUM MEDICAL AND HEALTH STANDARDS FOR PAID FIREMEN. ...... 3 012. ABDOMINAL ORGANS AND GASTROINTESTINAL SYSTEM. ...................... 3 013. BLOOD AND BLOOD-FORMING TISSUE DISEASES. ................................... 4 014. DENTAL. .......................................................................................................... 5 015. EARS. ............................................................................................................... 6 016. HEARING. ......................................................................................................... 6 017. ENDOCRINE AND METABOLIC DISORDERS. ............................................... 7 018. UPPER EXTREMITIES. .................................................................................... 7 019. LOWER EXTREMITIES. .................................................................................. -

Gastrointestinal Complications of the Ehlers- Danlos Syndrome
Gut: first published as 10.1136/gut.10.12.1004 on 1 December 1969. Downloaded from Gut, 1969, 10, 1004-1008 Gastrointestinal complications of the Ehlers- Danlos syndrome PETER H. BEIGHTON1, J. LAMONT MURDOCH2, AND THEODORE VOTTELER3 From Johns Hopkins Hospital, Baltimore, USA SUMMARY The gastrointestinal abnormalities encountered in 125 patients with the Ehlers-Danlos syndrome have been described. Spontaneous perforation of the intestine and massive gastrointestinal haemorrhage are uncommon but potentially lethal complications of the Ehlers-Danlos syndrome. Less dangerous abnormalities, such 'as external hernia, hiatus hernia, eventration of the diaphragm, intestinal diverticula, and rectal prolapse were all encountered in patients in the series. Abdominal surgery in affected patients may be made difficult by fragility of tissues and a bleeding tendency. In the postoperative period, tearing out of sutures and wound dehiscence may occur. Although the Ehleis-Danlos syndrome is uncommon, TABLE I affected individuals may be readily recognized by GASTROINTESTINAL COMPLICATIONS IN 125 PATIENTS WITH the hypermobility of the joints, the hyperexten- THE EHLERS-DANLOS SYNDROME sibility of the skin, and the wide, thin scars that Complication Number ofPatients frequently oveilie the bony prominences. Bleeding http://gut.bmj.com/ The fragility and laxity of tissue are not confined Severe haematemesis and melaena 6 to the dermis, and the gastrointestinal tract may Peptic ulceration 3 Hiatus hernia also be involved. These features, together with a No demonstrable lesion 2 bleeding tendency of variable severity, place patients Melaena from colonic diverticula 2 at risk from a variety of gastrointestinal compli- External haemorrhoids 8 Skin splitting at the anal margin 5 cations. -

Department of Veterans Affairs § 4.114
Department of Veterans Affairs § 4.114 anastomotic stoma are sufficiently rec- mental principle relating to ognized as to warrant two separate pyramiding as outlined in § 4.14. graduated descriptions. In evaluating the ulcer, care should be taken that § 4.114 Schedule of ratings—digestive the findings adequately identify the system. particular location. Ratings under diagnostic codes 7301 to 7329, inclusive, 7331, 7342, and 7345 to § 4.111 Postgastrectomy syndromes. 7348 inclusive will not be combined There are various postgastrectomy with each other. A single evaluation symptoms which may occur following will be assigned under the diagnostic anastomotic operations of the stom- code which reflects the predominant ach. When present, those occurring disability picture, with elevation to during or immediately after eating and the next higher evaluation where the known as the ‘‘dumping syndrome’’ are severity of the overall disability war- characterized by gastrointestinal com- rants such elevation. plaints and generalized symptoms sim- Rat- ulating hypoglycemia; those occurring ing from 1 to 3 hours after eating usually 7200 Mouth, injuries of. present definite manifestations of Rate as for disfigurement and impairment of hypoglycemia. function of mastication. 7201 Lips, injuries of. Rate as for disfigurement of face. § 4.112 Weight loss. 7202 Tongue, loss of whole or part: With inability to communicate by speech ............. 100 For purposes of evaluating conditions One-half or more .................................................. 60 in § 4.114, the term ‘‘substantial weight With marked speech impairment ......................... 30 loss’’ means a loss of greater than 20 7203 Esophagus, stricture of: percent of the individual’s baseline Permitting passage of liquids only, with marked impairment of general health ........................... -

Gastrointestinal Involvement in the Ehlers-Danlos Syndromes
American Journal of Medical Genetics Part C (Seminars in Medical Genetics) 175C:181–187 (2017) ARTICLE Gastrointestinal Involvement in the Ehlers–Danlos Syndromes ASMA FIKREE, GISELA CHELIMSKY, HEIDI COLLINS, KATCHA KOVACIC, AND QASIM AZIZ* Current evidence suggests that an association exists between non-inflammatory hereditary disorders of connective tissue such as the Ehlers–Danlos syndromes (EDS) and gastrointestinal (GI) symptoms. Patients with EDS can present with both structural problems such as hiatus hernias, visceroptosis, rectoceles, and rectal prolapse as well as functional problems such as disordered gut motility. It has recently been demonstrated that patients with hypermobile EDS (hEDS) present with GI symptoms related to the fore and hind-gut and these patients frequently meet the criteria for functional gastrointestinal disorders such as functional dyspepsia and irritable bowel syndrome. Presence of GI symptoms in EDS patients influences their quality of life. Specific evidence based management guidelines for the management of GI symptoms in EDS patients do not exist and these patients are often treated symptomatically. There is, however, recognition that certain precautions need to be taken for those patients undergoing surgical treatment. Future studies are required to identify the mechanisms that lead to GI symptoms in patients with EDS and more specific treatment guidelines are required. © 2017 Wiley Periodicals, Inc. KEY WORDS: Ehlers–Danlos syndrome; gut motility; abdominal pain; constipation; diarrhea How to cite this article: Fikree A, Chelimsky G, Collins H, Kovacic K, Aziz Q. 2017. Gastrointestinal involvement in the Ehlers–Danlos syndromes. Am J Med Genet Part C Semin Med Genet 175C:181–187. INTRODUCTION and each member should provide a list of and care guidelines for the management references relevant to specific areas. -

Hepatosplenomegaly.Pdf
HEPATO‐SPLENOMEGALY IAP UG Teaching slides 2015-16 1 NORMAL LIVER • <4yrs : Liver normally palpable 2cm below Rt costal margin in the mid clavicular line. • <12yrs : 1 cm • > 12 yrs : not palpable • Smooth surface, Non tender, Round border IAP UG Teaching slides 2015-16 2 • Upper border is made out by percussion and lower border by palpation. • Upper border of the normal liver corresponds to 5th intercostal space in the Rt mid clavicularLIVER line. SPAN IAP UG Teaching slides 2015-163 3 • At 1 wk of age ‐‐‐‐‐ 4.5‐5 cm • At 12 yrs boys‐‐‐‐‐ 7‐8 cm girls ‐‐‐‐‐‐ 6‐6.5 cm NORMAL LIVER SPAN The lower edge of the rt lobe extends downward and palpable as a broad mass in some normal people(Riedel lobe) • > 12 yrs – liver usually not palpable IAP UG Teaching slides 2015-164 4 ABNORMAL LIVER CLINICALLY Firm liver Cirrhosis, TB Hard liver Malignancy Sharp border Cirrhosis, liver Tender liver infection (hepatitis, abscess), ccf,trauma Nodular liver Cirrhosis,neoplasm Asymmetric Tumor/ cyst enlargement IAP UG Teaching slides 2015-165 5 DOWNWARD DISPLACEMENT OF THE LIVER • Emphysema • Pleural effusion/empyema • Subdiaphramatic abscess • Relaxation of the abdominal musculature Generalized visceroptosis & Rickets • Thoracic deformity like narrow costal angle IAP UG Teaching slides 2015-166 6 HEPATOMEGALY IN NEWBORN •Neonatal hepatitis •Extrahepatic Biliary atresia, choledocal cyst •Erythroblastosis Fetalis •Intrauterine infections •Septicemia •Metabolic disorders like Galactosemia,Alpha‐ 1Antitrypsin deficiency etc IAP UG Teaching slides 2015-167 7 HEPATOMEGALY