Hidden Leprosy Cases in Tribal Population Groups and How to Reach Them Through a Collaborative Effort
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Environmental Impact Assessment of Krishnapatnam Industrial North Node
Andhra Pradesh Industrial National Industrial Corridor Development Infrastructure Corporation Corporation (NICDC) Limited. ENVIRONMENTAL IMPACT ASSESSMENT OF KRISHNAPATNAM INDUSTRIAL NORTH NODE Executive Summary August 2020 SUBMITTED BY L&T Infra Engineering C11811311 RP005, Rev. 0 L&T Infrastructure Engineering Ltd. Client: National Industrial Corridor Development Corporation Limited NICDC Project: Project No.: EIA Krishnapatnam North Node C1181311 Title: Document No.: Rev.: Executive Summary RP005 0 This document is the property of L&T Infrastructure Engineering Ltd. and File path: must not be passed on to any person or body not authorised by us to receive it l:\ports\2018\c1181311 - eia krishnapatnam node\working\reports\executive nor be copied or otherwise made use of either in full or in part by such person or summary\executive summmary english.docx body without our prior permission in writing. Notes: 1. Revision Details: IRR 0 31.08.2020 First Submission VHR SAP TKSS SNV Sign Init. Sign. Init. Init. Sign. Rev. Date Details . Prepared Checked Approved Table of Contents EIA Krishnapatnam North Node C1181311 Executive Summary RP005 rev. 0 TABLE OF CONTENTS 1 Introduction .....................................................................................................................................1 2 Project Site ......................................................................................................................................1 3 Justification of the Project ............................................................................................................3 -

Notice 50A Notice for Declaration of the Containment Zone
Notice 50A Notice for declaration of the Containment zone - Startino of Containment Ooerations Dt: 01.06.2020 I, M.V. Seshagiri Babu, District Collector and Magistrate, SPS Nellore District am of the considered opinion that the prevention and spread of COVID 19 infection is of paramount impoftance, in view of the public safety and the need to ensuring no loss to human/animal life due to spread of COVID 19 infection. Therefore, it is hereby notified that the following areas are immediately notified as containment zones and all activities which are permitted previously shall be restricted under the ambit of the National Disaster Management Act,2005. Strict Perimeter control shall be under enforcement in the core area while restricted movements inside the buffer area. Name of the Containment Areas falling within Areas falling with in Sl.No Mandal Containment Zone lD Core Area the Buffer Area Zone 1 Tada ArundatiWada NLR 57 Tada Kalluru Village Tada Mittalu Village Tada Appasamudram Appasamudram Appasamudram 2. Udayagiri NLR 58 Villaqe Villaqe Villaqe The above orders are promulgated in exercise of the powers conferred upon me as the Chairperson of the District Disaster management Authority under the Disaster management Act 2005. Any Violation of the above orders will be prosecuted under the relevant provisions of the Disaster Management Act 2005 and Sec 188 of the Indian Penal 1860. w Collector & SPS Nellore District ,w Copy to: All the District Heads in the District. The Hon'ble District Judge, Nellore for kind information. The DD, I & -

Zilla Parishad / Mandal Parishad Management - 04-06-2011
NELLORE > School Assistant > TELUGU>PHYSICAL SCIENCES - ZILLA PARISHAD / MANDAL PARISHAD MANAGEMENT - 04-06-2011 Working Category Is 8Years DOJ In in Maritial Rationali Achivem Noof Yrs Retireme Union Spouse Participat Achivem Total IsPrefCat S.No. Appl.No Emp Name EmpCode Date of Birth DateofJoining Name Of School Mandal Of Complete MobileNo Service present Status zationPoi entSSCP Disease Completed nt Points Points Points ionPoint entPoint Points Yes School d points School points nts oint Points 1 264217 G.VIJAYA LAKSHMI 111-01086388-115 01/08/1963 14/03/1986 ZPHS(G) KOVUR KOVUR I Yes 01/11/2002 9985363924 5 8 0 0 0 0 0 0 0 0 13 Widow MPUPS VENKATACHAL Legally 2 322538 PARNA.PRAMEELA 111-27107196-116 27/10/1971 06/11/1996 III No -- 9849379884 2.8 3 0 0 0 0 0 0 0 0 5.8 Seperate THATIPARTHIPALEM AM d woman If he/she ZPHS(G) DARGAMITTA is 3 324948 shaik zakira khanam 111-10086286-115 10/08/1962 16/09/1985 NELLORE I Yes 31/10/2002 9703848033 5 8 0 0 0 0 0 0 0 0 13 suffering Cancer NELLOR with the diseases Parents of Mentally 4 369957 VASANTHA KALYANI 111-01056589-115 01/05/1965 14/08/1986 ZPHS(Girls) SULLURPET III No -- 9951304302 4.8 15 0 0 0 0 0 0 0 0 19.8 Retarede d children Parents of ANUMASAMUD Mentally 5 334515 MABBU MURALI 816464 01/07/1969 27/03/1998 ZPHS A S PETA III No -- 9848992340 2.6 3 0 0 0 0 0 0 0 6 11.6 RAMPET Retarede d children Parents of children 6 354458 KUNDA ARUNAMMA 111-15067396-134 15/06/1973 13/11/1996 ZPHS MUNGAMUR BOGOLE IV No -- 9010356547 2.8 5 0 0 0 0 0 0 0 0 7.8 with juvenile diabeties GUDURU SUDHAKAR 7 292928 -
Ddos Nellore.Pdf
Name of DDO Mobile EMAIL ddodesg ddodesc OLD DDO CODE 9949911508 [email protected] M.P.D.O MPDO 8042202047 ATMAKUR B. VIJAY SUKUMAR 9573696378 [email protected] SPL.DY.COL SPL. DY 8011217005 L.TGP( LA) COLLECTO nellore unit R PANGULURU 9505517213 [email protected] AD AD 8010104001 ANITHA KUMARI MARKETING NLR B.Muralidhar 9848775361 PRL I.T.I Principal 8091502001 SANGAM [email protected] B.Ravindra Babu 8374449052; [email protected] AD AD 8010103001 HORTICULT URE NLR BALASANI 8374449053; [email protected] A.D OF AD 08012403001 SRINIVASULU HORTICULT URE NO.II,ATMAK URU P.Praharaju 9550785637 [email protected] SC BH NO.5 hostel welfar 0801-2402-006 M.Thirupathaiah 9705346067 [email protected] Office of the AAO 8030703001 Assistant Audit Officer, State Audit, Gudur Sri D.Simhadri 9705346057 [email protected] Office of the AAO 8010703004 Assistant Audit Officer, State Audit, Nellore G.VIJAYA LAKSHMI 9963694222; [email protected] Office of the DAO 8010703002 Assistant Audit Officer, State Audit (MANDAL PARISHAD), Nellore G.VIJAYA LAKSHMI 9963694222; [email protected] Office of the DAO 8010703003 Assistant Audit Officer, State Audit (ZP), Nellore T.Venkateswarlu 9849904497 [email protected] ABCWO ASST.BC 08012403001 NELLORE WELFARE OFFICER KAPARAPU 9494938251; [email protected] ASST CANE AST. CANE 8011308001 LOKESWAR COMMISSIO COMMISSIO NER NER ,PAPPULU STREET ,STONEHOU SEPET,NELL ORE K.Omkar Rao 9492555116 [email protected] ASS COMM ACL 8031503002 OF LABOUR GUDUR Sri P. Venkata 9492555115 [email protected] ASST ACL 8011503008 Narayana COMM OF LABOUR NELLORE Prabhu Kumar [email protected] AC.LEGAL AD 8011609001 Rayana METROLOG Y NELLORE Moldireddy.Sudhakar 9440902265; [email protected] A.C. -

2020052621.Pdf
COVID-lg - MOST URGENT PROCEEDINGS OF THE COLLECTOR & DISTRICT MAGISTRATE SPS NELLORE DISTRICT PRESENT: Sri M.V.SESHAGIRI BABU, t.A.S., Rc.D2.627/2020 Dated:23.05.2020 Sub: COVID-lg - Containment, Control & Prevention of COVID 19 - SPS Nellore District - Re defining of Containment Zones in the District - Staft and Stop of Coqtainment Operation - Orders - Ispued. Read: 1. Government of India, Ministry of Home Affairs, Order No.40-3I2020-DM-I(A), dt.L7.05.2020. 2. G.O.Rt.No: 274 of Health, Medical & Family Welfare (82) Department, Government of A.P., Velagapudi, dt.17.05.2020. 3. Order No: 50/COVID-1912O2O, COVID INSTANT ORDER - 50 of Special Chief Secretary, Health Medical & Family Welfare Department, Government of A. P., Vela gapudi, dt. 18.05. 2020. This office proceedi n gs Rc.D2/ 627 I 2020, dt: 21.05.2020. 4. This office proceedings Rc.D2162712020, dt: 21.05.2020. 5. Notice 50 B of Sub Collector, Kavali and Gudur and RDO, Naidupet and Nellore, dt22.05.2020, 6, Notice 50 A of RDO, Nellore and Atmakur, dt:22,05,2020, *x*** ORDER: In the reference 4th read above, 59 Containment Clusters have been notified in the District as per Instant Order - 50. In the reference 5th read above, the Sub Collector, Kavali and Gudur and the RDO, Naidupet and Nellore have reported that 33 Containment Clusters in their respective divisions can be de-notified from all containment operations as no fresh cases have been registered in the last 28 days. In the reference 6$ read above, the RDO, Nellore and Atmakur have reported that as new Corona positive cases -

List of Teachers Working in Sri Potti Sriramulu Nellore District - Mp/Zp Management - Community - Sc
LIST OF TEACHERS WORKING IN SRI POTTI SRIRAMULU NELLORE DISTRICT - MP/ZP MANAGEMENT - COMMUNITY - SC S.N o district subject) Surname Sub-Caste Community which DSC) which Date of Birth Date present cadre In which cadre In which Placeofworking specify the subject) specify GO orGO other than the Name of the Mandal Date of joining in the in of joining Date Date of joining in this this in of joining Date Treasury Authorities) Name of the Teacher Management which in By promotion orBy direct He/She first appointed He/She Year of Year recruitment (in Designation (if SA / LP. / LP. (if SA Designation Employee ID (Givern ID by Employee present post(Specify the present post(Specify Transfer made was under Inter District InterTransfer District / 610 Appointed in which District which in Appointed 1 S.R.PURAM 0831801 GOLLAPALLI G.V.Ramanaiah PSHM MPPS S.R.Nagar 01/01/1960 SC Madiga MP/ZP 1985 Nellore PSHM promotion 11/07/2003 2 S.R.PURAM 0823074 KALIVELA K.Vijayababu PSHM MPUPS Devamma Cheruvu 04/04/1963 SC Madiga MP/ZP 1986 Nellore PSHM promotion 02/12/2009 3 S.R.PURAM 0822538 THIRUVAIPATHI T. Sanjeevarao PSHM MPUPS N.R.Peta 15/06/1959 SC Mala MP/ZP 1984 Nellore PSHM promotion 18/07/2009 4 S.R.PURAM 0823046 JYOTHI J. Mala Kondaiah PSHM MPPS Pandrangi 15/07/1961 SC Mala MP/ZP 1985 Nellore PSHM promotion 02/12/2009 5 KONDAPURAM0818486 CHITTURI Karunakumari Chitturi PSHM MPPS Saipeta Main 01/03/1962 SC ADIANDHARA MP/ZP 1988 Nellore PSHM promotion 02/02/2009 6 KONDAPURAM0829294 MOCHERLA Venkataramanamma Mocherla PSHM MPPS Kovivaripalli 15/08/1960 SC HARIJANA -
C.G.No.Nellore 2 Order.No.86
BEFORE THE FORUM FOR REDRESSAL OF CONSUMER GRIEVANCES IN SOUTHERN POWER DISTRIBUTION COMPANY OF A.P LIMITED TIRUPATI On this the 31st day of August 2015 In C.G.No:86/ 2015-16/Nellore Circle Present Sri P.Venkateswara Prasad Chairperson Sri A.Sreenivasula Reddy Member (Accounts) Sri T. Rajeswara Rao Member (Legal) Between Sri Putta Sreenivasulu ,Sarpanch Complainant Kalluru grama panchayat of Vakadu Nellore-Dist 524403 AND 1.Assistant Engineer/Vakadu Respondents 2. Assistant Divisional Engineer/Kota 3. Divisional Engineer/Gudur 4.Superintending Engineer/Nellore *** Sri Putta Sreenivasulu Sarpanch of Kalluru Gram Panchayati of Vakudu Mandal ,Nellore -Dist, here in called the complainant, In his complaint dt:29.04.2015filed in the Forum on dt:29.04.2015 under clause 5 (7) of APERC regulation 1/2004 read with section 42 (5) of I.E.Act 2003 has stated that: 1. He is Ne Sarpanch of Kalluru Gram Panchayati of Vakudu Mandal Nellore –Dist. 2. He said that twenty families are living in harijana (SC) Colony , Kodiwaka Village. The heights of the Electrical lines in that colony are not adequate for them , as C.G.No:86/2015-16/Nellore Circle Electrical poles are located in low heights . In 1987 Govt sanctioned Housing colonies for BC colony people , at that time Govt. Deployed electrical poles for them, now they became so Older. BC Colony people built new houses in place of older ones as Govt. sanctioned new houses for them. But the height of poles remains same . Unfortunately the people living in the BC Colony also facing low height of electrical lines problem as Electrical lines are touching their houses . -

Volunteer Name with Reg No State (District)
Volunteer Name with Reg No State (District) (Block) Mobile no TEMBURU DILLESWARA ANDHRA PRADESH (Srikakulam) (Kotturu ) 8985832170 RAO (63838) AGATHAMUDI SRILATA (63742) ANDHRA PRADESH (Srikakulam) (Gara ) 9291389567 DASARI YOGESWARARAO (63869) ANDHRA PRADESH (Srikakulam) (Mandasa ) 9573933397 ANDHRA MUDADLA CHAKRADHAR (63868) 9908758528 PRADESH (Srikakulam) (Veeraghattam ) BALIVADA SURENDRA ANDHRA PRADESH (Srikakulam) (Palakonda ) 9381761383 KUMAR (63867) PUTHI SRAVAN KUMAR (63866) ANDHRA PRADESH (Srikakulam) (Palakonda ) 8186829362 NITYANANDA BADITYA (63864) ANDHRA PRADESH (Srikakulam) (Ichapuram) 9640480629 PANCHIREDDY ANDHRA PRADESH (Srikakulam) (Gara ) 9966353032 SIVAKUMAR (63863) BOMMALI CHANDINI (63848) ANDHRA PRADESH (Srikakulam) (Ichapuram) 7702668113 BOORE NARENDRA ANDHRA PRADESH (Srikakulam) (Tekkali) 9989512521 CHAKRAVARTHI (63847) DASARI SHANMUKHARAO (63846) ANDHRA PRADESH (Srikakulam) (Tekkali) 9494042926 ANDHRA VANJARAPU MOHAN RAO (63843) 7893862127 PRADESH (Srikakulam) (Kotabommali) ANDHRA BATCHALA NAGARAJU (63841) 9177212779 PRADESH (Srikakulam) (Kotabommali) GANADUBILLI ANDHRA 7075576526 PAVANKUMAR (63697) PRADESH (Srikakulam) (Amadalavalasa ) KOTTISA HARITHA (63871) ANDHRA PRADESH (Srikakulam) (Gara ) 9966153952 ANDHRA PALAPARTI SATEESH (63817) 9492820189 PRADESH (Srikakulam) (Seethampeta ) ANDI VEERA BHADRAYYA (63745) ANDHRA PRADESH (Srikakulam) (Rajam ) 8008929291 ANDHRA RAKOTI SHIVA KUMAR (63733) 7396243916 PRADESH (Srikakulam) (Amadalavalasa ) BASAVA KUSUMA (63747) ANDHRA PRADESH (Srikakulam) (Rajam ) 9959900618 -

Hand Book of Statistics S.P.S. Nellore District 2014
HAND BOOK OF STATISTICS S.P.S. NELLORE DISTRICT 2014 Compiled and Published by CHIEF PLANNING OFFICER Sri Potti Sriramulu Nellore District OFFICERS & STAFF ASSOCIATED WITH THE PUBLICATION Sl No Name of the Officer Designation 1 Sri K.T.VENKAIAH CHIEF PLANNING OFFICER [FAC] 2 Sri K.MADHUSUDHAN ASSISTANT DIRECTOR 3 Sri M.V.SRINIVASAN STATISTICAL OFFICER 4 Smt. M.V.RATNAM DY. STATISTICAL OFFICER 5 Sri A.V.RAMESH A.S.O. 6 Sri C.YUGANDHAR TYPIST <<<>>> HAND BOOK OF STATISTICS - S.P.S. NELLORE DIST - 2014 INDEX TABLE ITEM PAGE NO. NO. 1 SALIENT FEATURES OF S.P.S.R.NELLORE DISTRICT 1 2 COMPARISON OF DISTRICT WITH STATE FOR THE YEAR 2013-14 7 3 ADMINISTRATIVE DIVISIONS IN THE DISTRICT - 2014 13 4 PUBLIC REPRESENTATIVES/ NON-OFFICIALS AS ON 31.03.2014 15 PROFILE OF ASSEBLY/ PARLIAMENTARY CONSTITUENCY AS PER DELIMITATION 5 21 ACT, 2002 1 - POPULATION 1.1 VARIATION IN POPULATION OF - 1901 TO 2011 24 1.2 POPULATION STATISTICS SUMMEARY-POPULATION CENSUS, 2001- 2011 25 TOTAL NO.OF VILLAGES, HMLETS, HOUSEHOLDS, AREA, POPULATION, DENSITY 1.3 26 OF POPULATION AND SEX RATIO, MANDAL-WISE- POPULATION CENSUS, 2011 1.4 RURAL AND URBAN POPULATION , MANDAL - WISE, 2011 POPULATION CENSUS 28 1.5 POPULATION OF TOWNS AND CITIES - 2011 POPULATION CENSUS 29 1.6 LITERACY, MANDAL - WISE, POPULATION CENSUS 2011 30 SCHEDULED CASTE POPULATION AND LITERACY RATE - POPULATION CENSUS 1.7 31 2011 SCHEDULED TRIBES POPULATION AND LITERACY RATE,POPULATION CENSUS 1.8 32 2001 DISTRIBUTION OF POPULATION BY WORKERS AND NON WORKERS - 1.9 33 MANDAL WISE , 2011 POPULATION CENSUS CLASSIFICATION -

BEFORE the NATIONAL GREEN TRIBUNAL SOUTHERN ZONE, CHENNAI Application No. 216 of 2015 (SZ) in the MATTER OF: Nimmala Ankaiah S
BEFORE THE NATIONAL GREEN TRIBUNAL SOUTHERN ZONE, CHENNAI Application No. 216 of 2015 (SZ) IN THE MATTER OF: Nimmala Ankaiah S/o.Ankaiah Vittaiahjpalem (V) Chilamattur (Post) Varadaiiah Palem (Mandal), Chittoor District, Andhra Pradesh - 517 541 ... Applicant AND 1. Union of India rep by Secretary to Government, Ministry of Environment, Forests and Climate Change, New Delhi 110 003. 2. The State of Andhra Pradesh, Rep. by its Secretary Environment, Forest, Science and Technology Department, A.P.Secretariat, Hyderabad 500 004. 3. The Srate of Andhra Pradesh, Rep. By its Secretary, Industries and Commerce Department, A.P.Secretariat, Hyderabad- 500 004 4. The Andhra Pradpesh Industrial Infrastructure Corporation Ltd., Rep. By its Managing Director, ParishramaBhavan, Basheerbagh, Hyderabad -500 036. 5. The Collector and District Magistrate cum Chairman, Pulicat ESZ Monitoring Committee, PSR Nellore District, Nellore - 524 001. 6. M/S.GVK EMRI Devarayamzal Post, Medchal Road, Hyderabad.-500 078 7. M/s. GROB Machine Tools India Private Ltd., Sy.No.145, Plot NO.132/B, 4th Floor, Sardar Patel Nagar, Hyder Nagar, Kukatpally, Hyderabad - 500 072. 8. Andhra Pradesh State Pollution Control Board, Rep. By its Member Secretary, PayavaranBhawn - A- III, Industrial Estate, Sanath Nagar, Hyderabad - 500 018. ... Respondent(s) Counsel appearing for the Applicant: Mr.T.Mohan , Sr.Counsel for Rema Smrithi V.K. Counsel appearing for the Respondents: Mr. G.M. Syed Nurullah Sheriff for R-1 Mrs. H.Yasmeen Ali for R2 to R5 Mr.T.Sai Krishnan for R8 M/s. N.Jayakumar for R6. ORDER PRESENT: HON’BLE SHRI JUSTICE DR. P. JYOTHIMANI, JUDICIAL MEMBER HON’BLE SHRI P.S. -
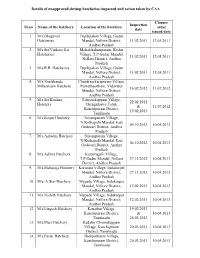
List of Unapproved Shrimp Hatcheries Inspected and Action Taken By
Details of unapproved shrimp hatcheries inspected and action taken by CAA Closure Inspection Sl.no Name of the hatchery Location of the hatchery order date issued date 1. M/s.Bhagavan Tupilipalem Village, Gudur Hatcheries Mandal, Nellore District, 11.02.2011 12.05.2011 Andhra Pradesh 2. M/s.Sri Venkata Sai Mahalakshmipuram, Kodur Hatcheries Village, T.P.Gudur Mandal, 11.02.2011 12.05.2011 Nellore District, Andhra Pradesh 3. M/s.R.R. Hatcheries Tupilipalem Village, Gudur Mandal, Nellore District, 11.02.2011 12.05.2011 Andhra Pradesh 4. M/s.Neelakanda Chandrasekarapuram Village, Millennium Hatchery Ramatheertham, Vidavalur 16.02.2012 11.07.2012 Mandal, Nellore District, Andhra Pradesh 5. M/s.Sri Krishna Edaiyurkuppam Village, 22.02.2012 Hatchery Chengalpattu Taluk, & 11.07.2012 Kanchipuram District, 19.02.2013 Tamilnadu 6. M/s.Kaijin Hatchery Srirampuram Village, U.Kothapalli Mandal, East 04.10.2012 10.04.2013 Godavari District, Andhra Pradesh 7. M/s.Ashwini Hatchery Srirampuram Village, U.Kothapalli Mandal, East 04.10.2012 10.04.2013 Godavari District, Andhra Pradesh 8. M/s.Aditya Hatchery Kattuvapalli Village, T.P.Gudur Mandal, Nellore 27.11.2012 10.04.2013 District, Andhra Pradesh 9. M/s.Maharaja Hatchery Koruturu Village, Indukurpet Mandal, Nellore District, 27.11.2012 10.04.2013 Andhra Pradesh 10. M/s/.A Star Hatchery Mypadu Village, Indukurpet Mandal, Nellore District, 12.02.2013 10.04.2013 Andhra Pradesh 11. M/s.Nishith Hatchery Mypadu Village, Indukurpet Mandal, Nellore District, 12.02.2013 10.04.2013 Andhra Pradesh 12. M/s.Lingesh Hatchery Kanathur Village, 19.02.2013 Kanchipuram District, & 10.04.2013 Tamilnadu 26.03.2013 13. -
Copy of LEFT VACANCIES
LIST OF THE LEFT OVER VACANCIES AFTER TRANSFER COUNSELLING - JULY - 2012 SPSR NELLORE DISTRICT No.Vacan S.No DESIG-MGT NAME OF THE SCHOOL MANDAL REMARKS cies 1 PSHM-LB MPPS, CHEJARLA MAIN CHEJERLA 1 2 PSHM-LB MPPS, T.K.PADU HW CHEJERLA 1 3 PSHM-LB MPPS VALLIPEDU CHILLAKUR 1 4 PSHM-LB MPPS, CHILLAKUR MAIN CHILLAKUR 1 5 PSHM-LB MPPS, N.R.PALLI MAIN CHILLAKUR 1 6 PSHM-LB MPPS, PALLAMALA CHILLAKUR 1 7 PSHM-LB MPPS, PENTAPADU CHILLAKUR 1 8 PSHM-LB MPPS, VARAGALI HW CHILLAKUR 1 9 PSHM-LB MPPS, CHITTAMUR CHITTAMUR 1 10 PSHM-LB MPPS, ESWARAWAKA CHITTAMUR 1 11 PSHM-LB MPPS DAGGAVOLU DAKKILI 1 12 PSHM-LB MPPS, Utchuru DORAVARISATRAM 1 13 PSHM-LB MPPS VEDICHERLA HW GUDUR 1 14 PSHM-LB MPPS, JALADANKI MAIN JALADANKI 1 15 PSHM-LB MPPS GUDLADONA (EAST) KALIGIRI 1 16 PSHM-LB MPPS, KALIGIRI MAIN KALIGIRI 1 17 PSHM-LB MPPS CHEEPINAPI MAIN KALUVOYA 1 18 PSHM-LB MPPS VERUBOTLAPALLI M KALUVOYA 1 19 PSHM-LB MPPS TC PALEM KAVALI 1 20 PSHM-LB MPPS KOMMI KONDAPURAM 1 21 PSHM-LB MPPS, KOTA (GP) KOTA 1 22 PSHM-LB MPPS, SIDDAMMA KANDRIGA KOTA 1 23 PSHM-LB MPPS, SIDDAVARAM KOTA 1 24 PSHM-LB MPPS, Thimmanaidupalem KOTA 1 25 PSHM-LB MPPS, Venkannapalem KOTA 1 26 PSHM-LB MPPS, K.R.PURAM AW MANUBOLU 1 27 PSHM-LB MPPS NEREDANAMPADU MARRIPADU 1 28 PSHM-LB MPPS, Kothapalem of Pynapuram MUTHUKUR 1 29 PSHM-LB MPPS, Krishnaptanam MUTHUKUR 1 30 PSHM-LB MPPS, Venkannapalem MUTHUKUR 1 31 PSHM-LB MPPS SOUTHMOPUR MAIN NELLORE 1 32 PSHM-LB MPPS DIGUVACHAVALI PELLAKUR 1 33 PSHM-LB MPPS NANDIMALA PELLAKUR 1 34 PSHM-LB MPPS, CHEMBEDU PELLAKUR 1 35 PSHM-LB MPPS PARLAPALLI PODALAKUR