Genetic and Pharmacologic Studies Towards Prevention of Opioid Use Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Naloxegol (Movantik) Reference Number: ERX.NSMN.02 Effective Date: 07/16 Last Review Date: 03/16
Clinical Policy: naloxegol (Movantik) Reference Number: ERX.NSMN.02 Effective Date: 07/16 Last Review Date: 03/16 Clinical policies are intended to be reflective of current scientific research and clinical thinking. This policy is current at the time of approval, may be updated and therefore is subject to change. This Clinical Policy is not intended to dictate to providers how to practice medicine, nor does it constitute a contract or guarantee regarding payment or results. Providers are expected to exercise professional medical judgment in providing the most appropriate care, and are solely responsible for the medical advice and treatment of members. This policy is the property of Envolve Pharmacy Solutions. Unauthorized copying, use, and distribution of this Policy or any information contained herein is strictly prohibited. By accessing this policy, you agree to be bound by the foregoing terms and conditions, in addition to the Site Use Agreement for Health Plans associated with Envolve Pharmacy Solutions. Description The intent of the criteria is to ensure that patients follow selection elements established by Envolve Pharmacy Solutions for the use of naloxegol (MovantikTM). Policy/Criteria It is the policy of health plans affiliated with Envolve Pharmacy Solutions that naloxegol (Movantik) is medically necessary for members meeting the following criteria: Initial Approval Criteria: I. Opioid-Induced Constipation (OIC) (must meet all) A. Age is ≥ 18 years old; B. Diagnosis of opioid-induced constipation; C. Member has used an opioid analgesic ≥ 4 weeks; D. Member is not being treated for cancer pain; E. Member has failed ≥ 2 non-bulk forming laxatives (see Table A) from different classes while on opioid therapy, unless contraindicated; F. -

204760Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 204760Orig1s000 OTHER REVIEW(S) MEMORANDUM DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH DATE: September 16, 2014 FROM: Julie Beitz, MD SUBJECT: Approval Action TO: NDA 204760 Movantik (naloxegol) tablets AstraZeneca Pharmaceuticals LP Summary Naloxegol is an antagonist of opioid binding at the muͲopioid receptor. When administered at the recommended dose levels, naloxegol functions as a peripherallyͲacting opioid receptor antagonist in tissues such as the gastrointestinal tract, thereby decreasing the constipating effects of opioids. Naloxegol is a PEGylated derivative of naloxone and a new molecular entity. Pegylation confers the following properties: naloxegol has reduced passive permeability across membranes compared to naloxone; naloxegol is a PͲglycoprotein (PͲgp) efflux transporter substrate; and naloxegol is orally bioavailable. The reduced passive permeability and PͲgp efflux transporter properties limit CNS entry of naloxegol compared to naloxone. This memo documents my concurrence with the Division of Gastroenterology and Inborn Errors Product’s recommendation for approval of NDA 204760 for Movantik (naloxegol) tablets for the treatment of opioidͲinduced constipation (OIC) in adult patients with chronic nonͲcancer pain. Discussions regarding product labeling, and postmarketing study requirements and commitments have been satisfactorily completed. There are no inspectional issues that preclude approval. Dosing The recommended dose of Movantik (naloxegol) tablets is 25 mg taken once daily in the morning on an empty stomach. Patients who do not tolerate this dose, may reduce the dose to 12.5 mg once daily. Maintenance laxatives should be discontinued prior to initiation of therapy with Movantik. -

Design and Synthesis of Cyclic Analogs of the Kappa Opioid Receptor Antagonist Arodyn
Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn By © 2018 Solomon Aguta Gisemba Submitted to the graduate degree program in Medicinal Chemistry and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Dr. Michael Rafferty Dr. Teruna Siahaan Dr. Thomas Tolbert Date Defended: 18 April 2018 The dissertation committee for Solomon Aguta Gisemba certifies that this is the approved version of the following dissertation: Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Date Approved: 10 June 2018 ii Abstract Opioid receptors are important therapeutic targets for mood disorders and pain. Kappa opioid receptor (KOR) antagonists have recently shown potential for treating drug addiction and 1,2,3 4 8 depression. Arodyn (Ac[Phe ,Arg ,D-Ala ]Dyn A(1-11)-NH2), an acetylated dynorphin A (Dyn A) analog, has demonstrated potent and selective KOR antagonism, but can be rapidly metabolized by proteases. Cyclization of arodyn could enhance metabolic stability and potentially stabilize the bioactive conformation to give potent and selective analogs. Accordingly, novel cyclization strategies utilizing ring closing metathesis (RCM) were pursued. However, side reactions involving olefin isomerization of O-allyl groups limited the scope of the RCM reactions, and their use to explore structure-activity relationships of aromatic residues. Here we developed synthetic methodology in a model dipeptide study to facilitate RCM involving Tyr(All) residues. Optimized conditions that included microwave heating and the use of isomerization suppressants were applied to the synthesis of cyclic arodyn analogs. -

Characterization and Re-Evaluation of Experimental Pain Models in Healthy Subjects
pain models in healthy subje healthy in models pain re-evaluation of experimental Chara pieter siebenga CharaCterization and C terization and re-evaluation of experimental pain models in healthy subjeCts pieter siebenga C ts 342_Omslag_01.indd 1 04-02-20 12:59 CharaCterization and re-evaluation of experimental pain models in healthy subjeCts 04-02-20 12:59 04-02-20 2 342_Omslag_01.indd CharaCterization and re-evaluation of experimental pain models in healthy subjeCts proefsChrift Ter verkrijging van de graad van Doctor aan de Universiteit Leiden, op gezag van Rector Magnificus prof. Mr. C.J.J.M. Stolker, volgens besluit van het College voor Promoties te verdedigen op woensdag 04 maart 2020 klokke 10:00 uur door Pieter Sjoerd Siebenga geboren te Dronten in 1984 Promotor 1 Pharmacodynamic Evaluation: Pain Methodologies — 7 Prof. dr. A.F. Cohen SECTION I The efficacy of different (novel) analgesics by using the Co-promotor PainCart Dr. G.J. Groeneveld 2 Analgesic potential of pf-06372865, an α2/α3/α5 subtype Leden promotiecommissie selective GABAA partial agonist, demonstrated using a battery Prof. dr. A. Dahan of evoked pain tasks in humans — 53 Prof. dr. A.E.W. Evers Dr. J.L.M. Jongen 3 Demonstration of an anti-hyperalgesic effect of a novel Prof. dr. E.C.M. de Lange pan-Trk inhibitor pf-06273340 in a battery of human evoked pain models — 73 4 Lack of detection of the analgesic properties of pf-05089771, a selective Nav1.7 inhibitor, using a battery of pain models in healthy subjects — 93 SECTION II Validation and improvement of human -

Moventig, INN-Naloxegol
Package leaflet: Information for the patient Moventig 12.5 mg film-coated tablets Moventig 25 mg film-coated tablets naloxegol Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor, pharmacist or nurse. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Moventig is and what it is used for 2. What you need to know before you take Moventig 3. How to take Moventig 4. Possible side effects 5. How to store Moventig 6. Contents of the pack and other information 1. What Moventig is and what it is used for Moventig contains the active substance naloxegol. It is a medicine used in adults to treat constipation specifically caused by pain medicines, called opioids, (e.g. morphine, oxycodone, fentanyl, tramadol, codeine) taken on a regular basis. It is used when laxatives have not provided acceptable relief of constipation. Constipation related to opioids can result in symptoms such as: • stomach pain • rectal straining (having to push very hard to move the stool out of the rectum, which can also cause pain in the anus during pushing) • hard stools (stools which are hard “like a rock”) • incomplete emptying of the rectum (after having a bowel movement, the feeling as if a stool is still in the rectum which needs to come out) In patients taking opioids with constipation, who have tried at least one laxative and had incomplete relief of constipation, Moventig has been shown in clinical trials to increase the number of bowel movements and improve symptoms of constipation caused by opioids. -
Methylnaltrexone Nonf
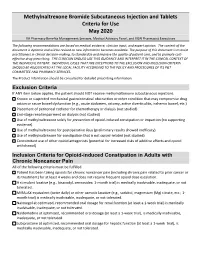
Methylnaltrexone Bromide Subcutaneous Injection and Tablets Criteria for Use May 2020 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The following recommendations are based on medical evidence, clinician input, and expert opinion. The content of the document is dynamic and will be revised as new information becomes available. The purpose of this document is to assist practitioners in clinical decision-making, to standardize and improve the quality of patient care, and to promote cost- effective drug prescribing. THE CLINICIAN SHOULD USE THIS GUIDANCE AND INTERPRET IT IN THE CLINICAL CONTEXT OF THE INDIVIDUAL PATIENT. INDIVIDUAL CASES THAT ARE EXCEPTIONS TO THE EXCLUSION AND INCLUSION CRITERIA SHOULD BE ADJUDICATED AT THE LOCAL FACILITY ACCORDING TO THE POLICY AND PROCEDURES OF ITS P&T COMMITTEE AND PHARMACY SERVICES. The Product Information should be consulted for detailed prescribing information. Exclusion Criteria If ANY item below applies, the patient should NOT receive methylnaltrexone subcutaneous injections. Known or suspected mechanical gastrointestinal obstruction or other condition that may compromise drug action or cause bowel dysfunction (e.g., acute abdomen, ostomy, active diverticulitis, ischemic bowel, etc.) Placement of peritoneal catheter for chemotherapy or dialysis (not studied) End-stage renal impairment on dialysis (not studied) Use of methylnaltrexone solely for prevention of opioid-induced constipation or impaction (no supporting evidence). Use of methylnaltrexone for postoperative ileus (preliminary results showed inefficacy). Use of methylnaltrexone for constipation that is not opioid-related (not studied) Concomitant use of other opioid antagonists (potential for increased risks of additive effects and opioid withdrawal) Inclusion Criteria for Opioid-induced Constipation in Adults with Chronic Noncancer Pain All of the following criteria must be fulfilled. -

Prescriber Update Vo.39 No.2. June 2018
Prescriber Update Vol. 39 No. 2 June 2018 www.medsafe.govt.nz ISSN 1172-5648 (print) ISSN 1179-075X (online) Contents Spotlight on Codeine 18 Making Medicines Safer: New e-Learning Module on Reporting Adverse Reactions Launched 19 Tenofovir Disoproxil – a Salty Tale 20 Medicines Interacting with Methadone 20 Hyoscine Butylbromide Injection and Cardiovascular Adverse Reactions 22 Using New Zealand Data to Review the Risk of Venous Thromboembolism with Combined Oral Contraceptives 23 Hypocalcaemia – a Risk with Zoledronic Acid 24 Pharmacogenomics – Helps Reduce Rash Decisions 25 MARC’s Remarks: March 2018 Meeting 27 Gathering Knowledge from Adverse Reaction Reports: June 2018 28 Medicines Monitoring: Dabigatran and gout or gout-like symptoms 29 Recent Approvals of Medicines Containing a New Active Ingredient 29 The Medsafe Files – Episode Six: Global Pharmacovigilance 29 Correction: Adverse Reaction Reporting in New Zealand – 2017 30 Medicine Classification Update – November 2017 31 Quarterly Summary of Recent Safety Communications 31 Report Adverse Drug Reactions 31 Subscribe to Prescriber Update 32 Spotlight on Codeine Key Messages phenotypes varies between populations. The relative frequencies of these phenotypes in the z The following patients should not use New Zealand population are not known. codeine as the risks of harm outweigh Poor metabolisers are unable to convert codeine any benefit: to morphine and receive little if any, analgesic – children aged under 12 years benefit. Extensive metabolisers convert 5–15% – adolescents aged under 18 years: for of codeine to morphine via the CYP2D6 enzyme. pain following surgery to remove In these patients, a 30 mg dose of codeine tonsils or adenoids, for symptomatic phosphate would yield approximately 1.5 mg to relief of cough, or in patients whose 4.5 mg of morphine. -

Oncology & Haematology
Oncology & Haematology Specialist Formulary List – NON-CHEMOTHERAPY DRUGS **Other indications for particular drugs may be included on completion of further specialist lists** For information on use of unlicensed medicines or medicines used 'off-label' - click here The following medicines are approved for prescribing by or on the recommendation of a prescribing oncology or haematology specialist (including non-medical prescribers where appropriate): In the event of a broken link please forward details to [email protected] Please include the location and full title of the link MEDICINE SUMMARY OF RESTRICTED INDICATION CATEGORY PROTOCOL Aprepitant capsules Adjunct to dexamethasone and a 5HT3-receptor antagonist NOSCAN (North of Scotland Cancer in preventing nausea and vomiting associated with cisplatin Network) Antiemetic Protocol pending. containing chemotherapy regimes. Granisetron tablets, injection Chemotherapy-induced nausea and vomiting (2nd line). Prophylaxis of Chemotherapy Induced Usually given pre-chemotherapy. Nausea and Vomiting follow MASCC guidelines Levomepromazine tablets, injection Chemotherapy-induced nausea and vomiting (3rd line). www.mascc.org 6mg tablets available. Tablets may be halved. Usual dose 3mg or 6mg twice daily. Lorazepam tablets, injection Anticipatory nausea and vomiting. 0.5mg to 1mg the night before and morning of chemotherapy. Palonosetron Injection Chemotherapy-induced nausea and vomiting. Given as a single dose IV pre-chemotherapy Granisetron transdermal patch Prevention of nausea and vomiting -

Intravenous Oxycodone Versus Other Intravenous Strong Opioids for Acute Postoperative Pain Control: a Systematic Review of Randomized Controlled Trials
Pain Ther (2019) 8:19–39 https://doi.org/10.1007/s40122-019-0122-4 REVIEW Intravenous Oxycodone Versus Other Intravenous Strong Opioids for Acute Postoperative Pain Control: A Systematic Review of Randomized Controlled Trials Milton Raff . Anissa Belbachir . Salah El-Tallawy . Kok Yuen Ho . Eric Nagtalon . Amar Salti . Jeong-Hwa Seo . Aida Rosita Tantri . Hongwei Wang . Tianlong Wang . Kristal Cielo Buemio . Consuelo Gutierrez . Yacine Hadjiat Received: January 3, 2019 / Published online: April 19, 2019 Ó The Author(s) 2019 ABSTRACT (inclusive) that evaluated the acute postopera- tive analgesic efficacy of intravenous oxy- Introduction: Optimal pain management is codone against fentanyl, morphine, sufentanil, crucial to the postoperative recovery process. pethidine, and hydromorphone in adult We aimed to evaluate the efficacy and safety of patients (age C 18 years). Outcomes examined intravenous oxycodone with intravenous fen- included analgesic consumption, pain intensity tanyl, morphine, sufentanil, pethidine, and levels, side effects, and patient satisfaction. hydromorphone for acute postoperative pain. Results: Eleven studies were included in the Methods: A systematic literature search of review; six compared oxycodone with fentanyl, PubMed, Cochrane Library, and EMBASE data- two compared oxycodone with morphine, and bases was performed for randomized controlled three compared oxycodone with sufentanil. trials published from 2008 through 2017 There were no eligible studies comparing oxy- codone with pethidine or hydromorphone. Overall, analgesic consumption was lower with oxycodone than with fentanyl or sufentanil. Enhanced Digital Features To view enhanced digital Oxycodone exhibited better analgesic efficacy features for this article go to: https://doi.org/10.6084/ m9.figshare.7931558. than fentanyl and sufentanil, and comparable analgesic efficacy to morphine. -

Problems of Drug Dependence 1982 Proceedings of the 44Th Annual Scientific Meeting The
National Institute Drug Abuse MONOGRAPH SERIES Problems of Drug Dependence 1982 Proceedings of the 44th Annual Scientific Meeting The Committee on Problems of Drug Dependence, Inc. U. S. DEPARTMENT OF HEALTH AND HUMAN SERVICE • Public Health Service • Alcohol, Drug Abuse, and Mental Health Administration Problems of Drug Dependence, 1982 Proceedings of the 44th Annual Scientific Meeting, The Committee on Problems of Drug Dependence, Inc. Editor, Louis S. Harris, Ph.D. NIDA Research Monograph 43 April 1983 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse Office of Science 5600 Fishers Lane Rockville, Maryland 20657 NIDA Research Monographs are prepared by the research divisions of the National Institute on Drug Abuse and published by its Office of Science. The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art confer- ences, integrative research reviews and significant original research. Its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisory Board Avram Goldstein, M.D. Addiction Research Foundation Palo Alto, California Jerome Jaffe, M.D. University of Connecticut School of Medicine Farmington, Connecticut Reese T. Jones, M.D. Langley Porter Neuropsychiatric Institute University of California San Francisco, California Jack Mendelson, M.D. Alcohol and Drug Abuse Research Center Harvard Medical School McLean Hospital Belmont, Massachusetts Helen Nowlis, Ph.D. Rochester, New York Lee Robins, Ph.D. Washington University School of Medicine St. Louis, Missouri NIDA Research Monograph Series William Pollin, M.D. -

Journal of Pharmaceutical and Pharmacological Sciences
Journal of Pharmaceutical and Pharmacological Sciences Eldalal OA, et al. J Pharma Pharma Sci: 4: 186. Review Article DOI: 10.29011/2574-7711.100086 The Correlation between Pharmacological Parameters of Oxycodone and Opioid Epidemic Othman A. Eldalal1,3,4*, Farag E S Mosa2,3, Oladayo A. Oyebanji1, Avinash Satyanarayan. Mahajan1, Terry L Oroszi1 1Department of Pharmacology and Toxicology, Boonshoft School of Medicine, Wright State University, Dayton, Ohio, USA 2Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton, Alberta, Canada 3School of pharmacy, Omar Almukhtar University, Libya 4Department of Drug Technology, Faculty of Medical Technology, Derna, Libya *Corresponding author: Othman A. Eldalal, Department of Pharmacology and Toxicology, Boonshoft School of Medicine, Wright State University, Dayton, Ohio, USA Citation: Eldalal OA, Mosa FES, Oyebanji OA, Mahajan AS, Oroszi TL (2020) The Correlation between Pharmacological Param- eters of Oxycodone and Opioid Epidemic. J Pharma Pharma Sci: 4: 186. DOI: 10.29011/2574-7711.100086 Received Date: 16 March, 2020; Accepted Date: 30 March, 2020; Published Date: 06 April, 2020 Abstract Despite its high risk of abuse and diversion, Oxycodone remains a common choice in the management of moderate-to-se- vere pain. Increased consumption, largely secondary to increased prescription over the last 2 decades, has led to renewed interests in its pharmacology, and opioids in general. The behavioral impacts of oxycodone (and other opioids) are associated with several factors such as its chemical properties, pharmacodynamic properties, and pharmacokinetic parameters. The solubility and rate of absorption are essential factors that participate in the rapid concentration of oxycodone in the brain. Alterations in oxycodone metabolism have been associated with dose‐dependent kinetics, first-pass metabolism, and variations in genetic characters (poor or extensive metabolizers). -

(2) Patent Application Publication (10) Pub. No.: US 2017/0020885 A1 Hsu (43) Pub
US 20170020885A1 (19) United States (2) Patent Application Publication (10) Pub. No.: US 2017/0020885 A1 Hsu (43) Pub. Date: Jan. 26, 2017 (54) COMPOSITION COMPRISING A (52) U.S. CI. THERAPEUTIC AGENT AND A CPC ......... A61K 31/5377 (2013.01); A61K 9/0053 RESPIRATORY STIMULANT AND (2013.01); A61K 31/485 (2013.01); A61 K METHODS FOR THE USE THEREOF 9/5073 (2013.01); A61K 9/5047 (2013.01): A61K 45/06 (2013.01); A61K 9/0019 (71) Applicant: John Hsu, Rowland Heights, CA (US) (2013.01); A61K 9/209 (2013.01) (72) Inventor: John Hsu, Rowland Heights, CA (US) (57) ABSTRACT (21) Appl. No.: 15/214,421 (22) Filed: Jul. 19, 2016 The present disclosure provides a safe method for anesthesia or the treatment of pain by safely administering an amount Related U.S. Application Data of active agent to a patient while reducing the incidence or severity of suppressed respiration. The present disclosure (60) Provisional application No. 62/195,769, filed on Jul. provides a pharmaceutical composition comprising a thera 22, 2015. peutic agent and a chemoreceptor respiratory stimulant. In one aspect, the compositions oppose effects of respiratory Publication Classification suppressants by combining a chemoreceptor respiratory (51) Int. Cl. stimulant with an opioid receptor agonist or other respira A6 IK 31/5377 (2006.01) tory-depressing drug. The combination of the two chemical A6 IK 9/24 (2006.01) agents, that is, the therapeutic agent and the respiratory A6 IK 9/50 (2006.01) stimulant, may be herein described as the “drugs.” The A6 IK 45/06 (2006.01) present compositions may be used to treat acute and chronic A6 IK 9/00 (2006.01) pain, sleep apnea, and other conditions, leaving only non A6 IK 31/485 (2006.01) lethal side effects.