T Cell Responses in Patients with COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ENSG Gene Encodes Effector TCR Pathway Costimulation Inhibitory/Exhaustion Synapse/Adhesion Chemokines/Receptors
ENSG Gene Encodes Effector TCR pathway Costimulation Inhibitory/exhaustion Synapse/adhesion Chemokines/receptors ENSG00000111537 IFNG IFNg x ENSG00000109471 IL2 IL-2 x ENSG00000232810 TNF TNFa x ENSG00000271503 CCL5 CCL5 x x ENSG00000139187 KLRG1 Klrg1 x ENSG00000117560 FASLG Fas ligand x ENSG00000121858 TNFSF10 TRAIL x ENSG00000134545 KLRC1 Klrc1 / NKG2A x ENSG00000213809 KLRK1 Klrk1 / NKG2D x ENSG00000188389 PDCD1 PD-1 x x ENSG00000117281 CD160 CD160 x x ENSG00000134460 IL2RA IL-2 receptor x subunit alpha ENSG00000110324 IL10RA IL-10 receptor x subunit alpha ENSG00000115604 IL18R1 IL-18 receptor 1 x ENSG00000115607 IL18RAP IL-18 receptor x accessory protein ENSG00000081985 IL12RB2 IL-12 receptor x beta 2 ENSG00000186810 CXCR3 CXCR3 x x ENSG00000005844 ITGAL CD11a x ENSG00000160255 ITGB2 CD18; Integrin x x beta-2 ENSG00000156886 ITGAD CD11d x ENSG00000140678 ITGAX; CD11c x x Integrin alpha-X ENSG00000115232 ITGA4 CD49d; Integrin x x alpha-4 ENSG00000169896 ITGAM CD11b; Integrin x x alpha-M ENSG00000138378 STAT4 Stat4 x ENSG00000115415 STAT1 Stat1 x ENSG00000170581 STAT2 Stat2 x ENSG00000126561 STAT5a Stat5a x ENSG00000162434 JAK1 Jak1 x ENSG00000100453 GZMB Granzyme B x ENSG00000145649 GZMA Granzyme A x ENSG00000180644 PRF1 Perforin 1 x ENSG00000115523 GNLY Granulysin x ENSG00000100450 GZMH Granzyme H x ENSG00000113088 GZMK Granzyme K x ENSG00000057657 PRDM1 Blimp-1 x ENSG00000073861 TBX21 T-bet x ENSG00000115738 ID2 ID2 x ENSG00000176083 ZNF683 Hobit x ENSG00000137265 IRF4 Interferon x regulatory factor 4 ENSG00000140968 IRF8 Interferon -

Influence of Infection and Inflammation on Biomarkers of Nutritional Status
A2.4 INFLUENCE OF INFECTION AND INFLAMMATION ON BIOMARKERS OF NUTRITIONAL STATUS A2.4 Influence of infection and inflammation on biomarkers of nutritional status with an emphasis on vitamin A and iron David I. Thurnham1 and George P. McCabe2 1 Northern Ireland Centre for Food and Health, University of Ulster, Coleraine, United Kingdom of Great Britain and Northern Ireland 2 Statistics Department, Purdue University, West Lafayette, Indiana, United States of America Corresponding author: David I. Thurnham; [email protected] Suggested citation: Thurnham DI, McCabe GP. Influence of infection and inflammation on biomarkers of nutritional status with an emphasis on vitamin A and iron. In: World Health Organization. Report: Priorities in the assessment of vitamin A and iron status in populations, Panama City, Panama, 15–17 September 2010. Geneva, World Health Organization, 2012. Abstract n Many plasma nutrients are influenced by infection or tissue damage. These effects may be passive and the result of changes in blood volume and capillary permeability. They may also be the direct effect of metabolic alterations that depress or increase the concentration of a nutrient or metabolite in the plasma. Where the nutrient or metabolite is a nutritional biomarker as in the case of plasma retinol, a depression in retinol concentrations will result in an overestimate of vitamin A deficiency. In contrast, where the biomarker is increased due to infection as in the case of plasma ferritin concentrations, inflammation will result in an underestimate of iron deficiency. Infection and tissue damage can be recognized by their clinical effects on the body but, unfortunately, subclinical infection or inflammation can only be recognized by measur- ing inflammation biomarkers in the blood. -

The Gut Microbiota and Inflammation
International Journal of Environmental Research and Public Health Review The Gut Microbiota and Inflammation: An Overview 1, 2 1, 1, , Zahraa Al Bander *, Marloes Dekker Nitert , Aya Mousa y and Negar Naderpoor * y 1 Monash Centre for Health Research and Implementation, School of Public Health and Preventive Medicine, Monash University, Melbourne 3168, Australia; [email protected] 2 School of Chemistry and Molecular Biosciences, The University of Queensland, Brisbane 4072, Australia; [email protected] * Correspondence: [email protected] (Z.A.B.); [email protected] (N.N.); Tel.: +61-38-572-2896 (N.N.) These authors contributed equally to this work. y Received: 10 September 2020; Accepted: 15 October 2020; Published: 19 October 2020 Abstract: The gut microbiota encompasses a diverse community of bacteria that carry out various functions influencing the overall health of the host. These comprise nutrient metabolism, immune system regulation and natural defence against infection. The presence of certain bacteria is associated with inflammatory molecules that may bring about inflammation in various body tissues. Inflammation underlies many chronic multisystem conditions including obesity, atherosclerosis, type 2 diabetes mellitus and inflammatory bowel disease. Inflammation may be triggered by structural components of the bacteria which can result in a cascade of inflammatory pathways involving interleukins and other cytokines. Similarly, by-products of metabolic processes in bacteria, including some short-chain fatty acids, can play a role in inhibiting inflammatory processes. In this review, we aimed to provide an overview of the relationship between the gut microbiota and inflammatory molecules and to highlight relevant knowledge gaps in this field. -

Four Diseases, PLAID, APLAID, FCAS3 and CVID and One Gene
Four diseases, PLAID, APLAID, FCAS3 and CVID and one gene (PHOSPHOLIPASE C, GAMMA-2; PLCG2 ) : striking clinical phenotypic overlap and difference Necil Kutukculer1, Ezgi Yilmaz1, Afig Berdeli1, Raziye Burcu G¨uven Bilgin1, Ayca Aykut1, Asude Durmaz1, Ozgur Cogulu1, G¨uzideAksu1, and Neslihan Karaca1 1Ege University Faculty of Medicine May 15, 2020 Abstract We suggest PLAID,APLAID and FCAS3 have to be considered as same diseases,because of our long-term clinical experiences and genetic results in six patients.Small proportion of CVID patients are also PLAID/APLAID/FCAS3 patients and all these have disease-causing-mutations in PLCG2-genes,so it may be better to define all of them as “PLCG2 deficiency”. Key Clinical Message: Germline mutations in PLCG2 gene cause PLAID,APLAID,FCAS3, and CVID.Clinical experiences in patients with PLCG2 mutations led us to consider that PLAID, APLAID and FCAS3 are same diseases.It may be better to define all of them as “PLCG2 deficiency”. INTRODUCTION The PLCG2 gene which is located on the 16th chromosome (16q23.3) encodes phospholipase Cg2 (PLCG2), a transmembrane signaling enzyme that catalyzes the production of second messenger molecules utilizing calcium as a cofactor and propagates downstream signals in several hematopoietic cells (1). Recently, het- erozygous germline mutations in human PLCG2 were linked to some clinical phenotypes with some overlap- ping features|PLCg2-associated antibody deficiency and immune dysregulation syndrome (PLAID) (OMIM 614878) and autoinflammation, antibody deficiency, and immune dysregulation syndrome (APLAID) (OMIM 614878) (2-4) and familial cold autoinflammatory syndrome (FCAS3) (OMIM 614468) (5). All of them are autosomal dominant inherited diseases. -

A1068-CD86 Polyclonal Antibody
BioVision 05/16 For research use only CD86 Polyclonal Antibody CATALOG NO: A1068-100 ALTERNATIVE NAMES: T-lymphocyte activation antigen CD86, Activation B7-2 antigen, B70, BU63, CTLA-4 counter-receptor B72, FUN-1, CD86, CD86, CD28LG2 Western blot analysis of CD86 in NCI-H292 cell line lysate AMOUNT: 100 µl IMMUNOGEN: KLH conjugated synthetic peptide between 269-298 amino acids from the C-terminal region of human CD86. MOLECULAR WEIGHT: 37 kDa HOST/ISOTYPE: Rabbit IgG SPECIES REACTIVITY: Human PURIFICATION: This antibody is purified through a protein A column, followed by peptide affinity purification. FORM: Liquid FORMULATION: Supplied in PBS with 0.09% (W/V) sodium azide. STORAGE CONDITIONS: Maintain refrigerated at 2-8°C for up to 6 months. For long term RELATED PRODUCTS storage store at -20°C in small aliquots to prevent freeze-thaw cycles. DESCRIPTION: This gene encodes a type I membrane protein that is a member of the immunoglobulin superfamily. This protein is expressed by Human CellExp™ B7-2 /CD86, human recombinant (Cat. No. 7496-10, -50) antigen-presenting cells, and it is the ligand for two proteins at the CD86 (Human) ELISA Kit (Cat. No. K4175-100) cell surface of T cells, CD28 antigen and cytotoxic T-lymphocyte- Human CellExp™LAG3 /CD223, human recombinant (Cat. No. 7278-10, -50) associated protein 4. Binding of this protein with CD28 antigen is a costimulatory signal for activation of the T-cell. Binding of this CD223 (LAG3) Polyclonal Antibody (Cat. No. A1067-100) protein with cytotoxic T-lymphocyte-associated protein 4 negatively regulates T-cell activation and diminishes the immune response. -

Molecular and Clinical Characterization of LAG3 in Breast Cancer Through 2994 Samples
Molecular and Clinical Characterization of LAG3 in Breast Cancer Through 2994 Samples Qiang Liu Chinese Academy of Medical Sciences & Peking Union Medical College Yihang Qi ( [email protected] ) Chinese Academy of Medical Sciences and Peking Union Medical College https://orcid.org/0000-0001- 7589-0333 Jie Zhai Chinese Academy of Medical Sciences & Peking Union Medical College Xiangyi Kong Chinese Academy of Medical Sciences & Peking Union Medical College Xiangyu Wang Chinese Academy of Medical Sciences & Peking Union Medical College Yi Fang Chinese Academy of Medical Sciences & Peking Union Medical College Jing Wang Chinese Academy of Medical Sciences & Peking Union Medical College Research Keywords: Cancer immunotherapy, CD223, LAG3, Immune response, Inammatory activity Posted Date: June 19th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-36422/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/33 Abstract Background Despite the promising impact of cancer immunotherapy targeting CTLA4 and PD1/PDL1, a large number of cancer patients fail to respond. LAG3 (Lymphocyte Activating 3), also named CD233, is a protein Coding gene served as alternative inhibitory receptors to be targeted in the clinic. The impact of LAG3 on immune cell populations and co-regulation of immune response in breast cancer remained largely unknown. Methods To characterize the role of LAG3 in breast cancer, we investigated transcriptome data and associated clinical information derived from a total of 2994 breast cancer patients. Results We observed that LAG3 was closely correlated with major molecular and clinical characteristics, and was more likely to be enriched in higher malignant subtype, suggesting LAG3 was a potential biomarker of triple-negative breast cancer. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Effector CD4 T-Cell Transition to Memory Requires Late Cognate Interactions That Induce Autocrine IL-2
ARTICLE Received 3 Jun 2014 | Accepted 24 Sep 2014 | Published 5 Nov 2014 DOI: 10.1038/ncomms6377 Effector CD4 T-cell transition to memory requires late cognate interactions that induce autocrine IL-2 K. Kai McKinstry1,*, Tara M. Strutt1,*, Bianca Bautista1, Wenliang Zhang1, Yi Kuang1, Andrea M. Cooper2 & Susan L. Swain1 It is unclear how CD4 T-cell memory formation is regulated following pathogen challenge, and when critical mechanisms act to determine effector T-cell fate. Here, we report that following influenza infection most effectors require signals from major histocompatibility complex class II molecules and CD70 during a late window well after initial priming to become memory. During this timeframe, effector cells must produce IL-2 or be exposed to high levels of paracrine or exogenously added IL-2 to survive an otherwise rapid default contraction phase. Late IL-2 promotes survival through acute downregulation of apoptotic pathways in effector T cells and by permanently upregulating their IL-7 receptor expression, enabling IL-7 to sustain them as memory T cells. This new paradigm defines a late checkpoint during the effector phase at which cognate interactions direct CD4 T-cell memory generation. 1 Department of Pathology, University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, Massachusetts 01655, USA. 2 Trudeau Institute, 154 Algonquin Avenue, Saranac Lake, New York 12983, USA. * These authors contributed equally to this work. Correspondence and requests for materials should be addressed to K.K.M. (email: [email protected]). NATURE COMMUNICATIONS | 5:5377 | DOI: 10.1038/ncomms6377 | www.nature.com/naturecommunications 1 & 2014 Macmillan Publishers Limited. -
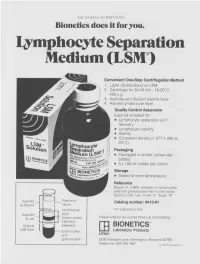
Lymphocyte Separation Medium (LSM
THE JOURNAL OF IMMUNOLOGY Bionetics does it for you. Lymphocyte Separation Medium (LSM wenient One-Step Centrifugation Method _ayer diluted blood on LSM. 2,entrifuge for 30-40 min., 18-20°C, ~.00 x g. ~,spirate and discard plasma layer -larvest lymphocyte layer. Quality Control Assurance Each lot is tested for: • Lymphocyte separation and recovery. • Lymphocyte viability. • Sterility. • Consistent density (1.077-1.080 at 20°C). Packaging • Packaged in amber, screw-cap bottles. • 5 x 100 ml bottles per carton. Storage. • Stored at room temperature. Reference Boyum, A. (1968): Isolation of mononuclear cells and granulocytes from human blood. Scand J. Clin. Lab. Invest. 21, Suppl. 97. Aspirate I IC[OI I IC~ LJI Catalog number: 8410-01 & discard serum Lymphocyte For Laboratory Use Aspirate layer & use (mononuclear Please write for our current Price List and Catalog. cells and Original platelets) ITi BIONETICS° LSM layer Erythrocytes Laboratory Products and Litton granulocytes 5516 Nicholson Lane, Kensington, Maryland 20795 Telephone: (301) 881-1557 1979 Litton Bionetics, tnc Get the most out of your high quality cytotoxic antibodies with LOW-TOX-M RABBIT COMPLEMENT LOW TOXICITY HIGH ACTIVITY Presentation: CL 3051 5 x 1 ml, lyophilized $30.00 When it comes to COMPLEMENT... come to CEDARLANE Direct orders or inquiries to: UNITED STATES: WORLDWIDE EXCEPT U.S. ,4 C~L CEDARLANE ACCURATE CHEMICAL & LABORATO RI ES SCIENTIFIC CORPORATION LIMITED 5516-8TH LINE, R.R. 2 28 TEC STREET, HICKSVtLLE, N.Y. 11801 HORNBY, ONTARIO, CANADA LOP 1E0 Telephone -

Abstract: Age-Related Immune Dysregulation and Increases In
Abstract: Age-related immune dysregulation and increases in inflammation, termed inflammaging, have been consistently implicated in most common age-related diseases, but the precise etiology of inter- individual differences in inflammaging are unknown. Changes in immunity and inflammation occur throughout the life course, but research on these processes among non-elderly populations has been limited. This is important because identifying sources of biological aging and inflammation before individuals reach older age may help identify points for intervention. The composition of the gut microbiota has been shown in animal models to have profound influence over, and interactions with, the immune system. Findings from germ-free mice suggest that commensal gut microbes are a key cause of inflammaging, but this hypothesis has not been well explored in humans. There are currently very few data examining how the microbiome relates to the fundamental aspects of aging biology, specifically inflammatory phenotypes and genomic markers of biological age. We propose to fill gaps in current microbiome research on aging, through the collection and analysis of oral and gut microbiome data in The National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative longitudinal cohort of adults with extensive social environment data and existing or ongoing analyses of genomic and phenotypic markers of inflammation and aging. The specific aims include the: 1) Collection of tongue and stool specimens with which to characterize the oral and gut microbiome in a nationally-representative sample (N ~10,155) of Add Health participants (mean age ~40); 2) Testing the association between the microbiome and biomarkers of aging and inflammation, and the creation of a novel “microbiome age clock”; 3) Examination of the relationships between life course exposures and microbiome species related to biomarkers of aging and inflammation as an adult; 4) Documentation and dissemination of data generated from this project. -

Stress and the Immune System Tracy B
4 World Health • 47th Yeor, No. 2, Morch-Aprill994 Stress and the immune system Tracy B. Herbert any people have the effects of factors as diverse as experienced the examinations, bereavement, divorce, Mconnection between stress unemployment, mental arithmetic, and getting sick. Colds, influenza, and looking after a relative with herpes and allergies seem worse Alzheimer's di sease. In general, when we are severely stressed at these studies find that stress is work or in the home. Others are related to changes in both the never sick until they go on vacation numbers of white blood cells in (that is, after the stress is over), and circulation and the quantity of then they spend the whole time antibody in the blood. Moreover, fighting the virus. Because of stress is associated with changes in intrinsic connections like these, the functioning of immune cells. many researchers are today That is, there is a relatively large exploring whether (and how) stress decrease in both lymphocyte and illness are actually linked. One proliferation and natural killer cell specific focus of this research is to activity in individuals who have study the effects of stress on the experienced stress. There seems to immune systems; after all, if stress A lymphocyte: stress may weaken the capacity be some connection between the affects immunity, that would be one of lymphocytes to combat infection. duration of the stress and the amount way in which stress could contribute of immune change. For example, the to illness. longer the stress, the greater the The function of the immune proliferation"- by incubating these decrease in the number of specific system is to protect us from cells for several days with types of white blood cells. -

Memory T Cells + Maintenance of CD8 the Dual Role of IL-2 in the Generation
The Dual Role of IL-2 in the Generation and Maintenance of CD8 + Memory T Cells Zhenhua Dai, Bogumila T. Konieczny and Fadi G. Lakkis This information is current as J Immunol 2000; 165:3031-3036; ; of September 30, 2021. doi: 10.4049/jimmunol.165.6.3031 http://www.jimmunol.org/content/165/6/3031 Downloaded from References This article cites 31 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/165/6/3031.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 30, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Dual Role of IL-2 in the Generation and Maintenance of CD8؉ Memory T Cells1 Zhenhua Dai, Bogumila T. Konieczny, and Fadi G. Lakkis2 The mechanisms responsible for the generation and maintenance of T cell memory are unclear. In this study, we tested the role of IL-2 in allospecific CD8؉ T cell memory by analyzing the long-term survival, phenotype, and functional characteristics of IL-2-replete (IL-2؉/؉) and IL-2-deficient (IL-2؊/؊) CD8؉ TCR-transgenic lymphocytes in an adoptive transfer model.